A Case of Insulinoma with Improved Reactive Hypoglycaemia after Operation
Shunsuke Funazaki1, Hodaka Yamada2, Yuko Matsumoto3, Kazuo Hara4
1 Clinical Fellow, Division of Endocrinology and Metabolism, Jichi Medical University Saitama Medical Center, Saitama, Japan.
2 Assistant Professor, Division of Endocrinology and Metabolism, Jichi Medical University Saitama Medical Center, Saitama, Japan.
3 Clinical Fellow, Division of Endocrinology and Metabolism, Jichi Medical University Saitama Medical Center, Saitama, Japan.
4 Professor, Division of Endocrinology and Metabolism, Jichi Medical University Saitama Medical Center, Saitama, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hodaka Yamada, Jichi Medical University Saitama Medical Center, 1-847 Amanuma-Cho, Omiya-Ku, 330-8503, Saitama, Japan.
E-mail: hyamada0510@jichi.ac.jp
It is well known that fasting hypoglycaemia is common in insulinoma, but postprandial hypoglycaemia has also been reported. In almost all cases, the serum Immunoreactive Insulin (IRI) level is not suppressed. A 54-year-old Japanese woman experienced repeated temporary loss of consciousness simultaneously with hypoglycaemia. 5-hour on admission, she had repeated hypoglycaemia without suppression of insulin. A 5-hour Oral 75 gm Glucose Tolerance Test (5-hour OGTT) showed reactive hypoglycaemia. Her serum IRI level was suppressed. Enhanced pancreatic Magnetic Resonance Imaging (MRI) revealed a 10 mm sized tumour in the pancreas; we thus diagnosed her with insulinoma. A laparoscopic distal pancreatectomy was performed. The 5-hour OGTT was performed again post operatively. Her abnormal glucose tolerance remained, but her reactive hypoglycaemia improved.
We conclude that reactive hypoglycaemia may occur in cases of insulinoma, and may be eliminated through operation. This case report has two important points. Firstly, the patient’s reactive hypoglycaemia was demonstrated. Secondly, her improving reactive hypoglycaemic state was recorded in detail.
Diabetes mellitus, Insulin, Pancreatic endocrine tumour
Case Report
A 54-year-old Japanese woman had suffered from temporary loss of consciousness for approximately 1.5 years, and her body weight had increased by 5 kg. She underwent her annual medical check up, but neither diabetes mellitus nor any abnormal findings were observed. One winter day, she visited a local clinic because her family identified strange behaviour several times. She was unable to open the door with her key and forgot where the lavatory was in her own house. The doctor suspected epilepsy, but electroencephalogram and brain MRI revealed no abnormality, except for a small pineal tumour.
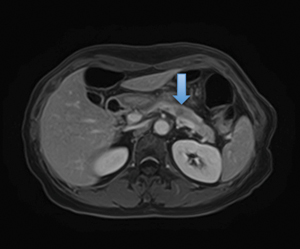
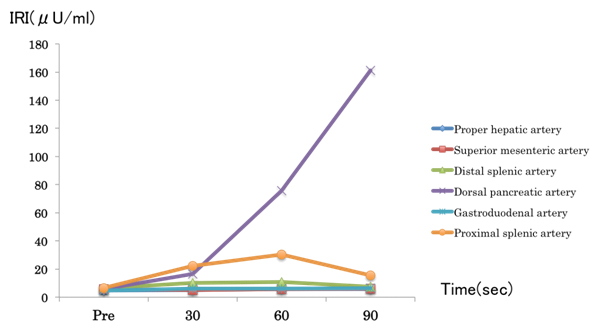
Four months later, her family again noticed that she was behaving strangely and was having loss of consciousness; therefore, she was admitted to our hospital. Her level of consciousness was E1V1M4 (Glasgow coma scale) with heavy cold sweats. The initial physical findings were as follows: height 152.4 cm; weight 52.4 kg; body mass index, 22.6 kg/m2; blood pressure, 136/65 mmHg; heart rate 69 beats/minute; body temperature 36.7°C; and respiratory rate 22 breaths/minute. Her blood glucose level was too low to measure. Blood test results revealed normal liver function, kidney function, and electrolyte levels. Her plasma glucose level was 33 mg/dL. serum IRI level was 4.2 μU/mL, serum C-peptide level was 1.16 ng/mL, and cortisol level was 27.1 ng/mL [Table/Fig-1]. The blood examinations suggested that endogenous insulin production was not suppressed despite severe hypoglycemia. After a 40 mg glucose injection, her plasma glucose level was elevated, and her consciousness improved. The 5-hour OGTT revealed impaired glucose tolerance and hypoglycaemia at 240 minutes [Table/Fig-2]. In a hypoglycaemic state, her serum IRI level was suppressed. This data was considered unreasonable, because hyperinsulinism is characteristic of hypoglycaemia via endogenous hyperinsulinemic hypoglycaemia. We judged the patient to have reactive hypoglycaemia. After admission, we performed the starvation test. Eight hours later, she experienced cold sweats and palpitations. Her blood test results revealed a plasma glucose level of 33 mg/dL, so we discontinued the test. At the time, her IRI level was 6.2 μU/mL, and serum C-peptide level was 2.62 ng/mL. Before the glucagon (1mg) injection test, the plasma glucose level was 43 mg/dL; whereas, after the test, the plasma glucose levels at 10, 20, and 30 minutes were 103, 135 and 132 mg/dL, respectively. Because her serum IRI and C-peptide levels were not suppressed, we suspected that she had endogenous hyperinsulinemic hypoglycaemia; e.g. insulinoma. Enhanced pancreas MRI indicated a 10 mm neuroendocrine tumour in the body of the pancreas [Table/Fig-3]. Endoscopic ultrasound revealed a single 10 × 7 mm sized low echoic lesion in the pancreas, with a clear border. Selective arterial calcium stimulation test srevealed insulin production by the pancreas [Table/Fig-4].
Laboratory data of the patient during a hypoglycaemic state.
| Parameter | Patient value | Reference range |
|---|
| Glycated hemoglobin | 4.8% | 4.6-6.2% |
| Total protein | 7.6 gm/dL | 6.5-8.0 gm/dL |
| Serum albumin | 5.3 gm/dL | 4.0-5.0 gm/dL |
| Aspartate transaminase | 27 U/L | 10-35 U/L |
| Alanine transaminase | 22 U/L | 5-30 U/L |
| Creatinine kinase | 225 U/L | 50-170 U/L |
| Serum sodium | 140 mEq/L | 138-145 mEq/L |
| Serum potassium | 4.5 mEq/L | 3.5-4.8 mEq/L |
| Serum chloride | 104 mEq/L | 101-108 mEq/L |
| Total cholesterol | 220 mg/dL | 130-220 mg/dL |
| Triglyceride | 78 mg/dL | 30-150 mg/dL |
| Blood urea nitrogen | 14 mg/dL | 8-20 mg/dL |
| Creatinine | 0.51 mg/dL | 0.4-0.8 mg/dL |
| Glucose | 33 mg/dL | 73-109 mg/dL |
| IRI | 4.2 μU/mL | 2.7-10.4 μU/mL |
| C-peptide | 1.16 ng/mL | 1.2-2.0 ng/mL |
| TSH | 2.4 μIU/mL | 0.35-4.94 μIU/mL |
| Cortisol | 27.1 ng/mL | 4.0-23.3 μg/mL |
IRI: immunoreactive insulin; TSH: thyroid-stimulating hormone
Data from the 5-hour OGTT at pre operation in a 54-year-old female patient*.
| Time (minutes) | 0 | 30 | 60 | 90 | 120 | 180 | 240 | 300 |
| Glucose (mg/dL) | 66 | 138 | 189 | 162 | 175 | 89 | 55 | 49 |
| IRI (μU/mL) | 3.5 | 21.8 | 24.9 | 16.8 | 11.8 | 2.7 | 1.6 | 2.8 |
Insulinogenic index = 0.25; IRI: immunoreactive insulin; OGTT: oral glucose tolerance test
*At 120 minutes, the patient’s glucose level was higher than 140 mg/dL. She had impaired glucose tolerance. At 240 and 300 minutes, she experienced hyperglycaemia. At that time, her serum IRI level was suppressed
Enhanced pancreatic magnetic resonance imaging of a 54-year-old woman revealing a 10 mm tumour in the body of the pancreas.
Immunoreactive insulin (IRI) status based on a selective arterial calcium stimulation test (calcium gluconate, 0.025 mg/kg infusion)*.
*The IRI level in the hepatic vein was elevated after we stimulated the dorsal pancreatic artery. The proximal splenic artery was slightly influenced
After two weeks, a laparoscopic distal pancreatectomy was performed. The tumour was strongly positive for insulin, synaptophysin, and chromogranin. Its histological examination didn’t contradict pancreatic insulinoma. The tumour was negative for MIB-1 index (ki-67); thus, the tumour had a low risk for malignancy. After the operation, her glucose levels recovered to normal range. She had no recurrence of strange behavior or loss of consciousness. Follow up 5-hour OGTT [Table/Fig-5] demonstrated impaired glucose tolerance, but reactive hypoglycaemia improved.
Data from the 5-hour OGTT at post operation in a 54-year-old female patient*.
| Time (minutes) | 0 | 30 | 60 | 90 | 120 | 180 | 240 | 300 |
| Glucose (mg/dL) | 104 | 208 | 150 | 168 | 130 | 86 | 81 | 97 |
| IRI (μU/mL) | 2.3 | 81.4 | 25.2 | 43.5 | 28.8 | 4.4 | 1.4 | 0.9 |
Insulinogenic index = 0.76; IRI: immunoreactive insulin; OGTT: oral glucose tolerance test
*For 5 hours, the patient did not experience hypoglycaemia. At 120 minutes, her glucose level was lower than 140 mg/dL. Her appropriate insulin secretory potential was recovered
Discussion
Insulinoma is a rare, with an incidence of 0.4/1,00,000 person years, and is more frequently observed in the fifth decade of life [1]. There are many different diagnostic criteria for insulinoma. The Endocrine Society Clinical Practice Guidelines recommend that plasma glucose levels of <55 mg/dL (3.0 mmol/L), insulin levels of at least 3.0 μU/mL (21.5 pmol/L), C-peptide levels of at least 0.6 ng/mL (0.2 nmol/L) [2]. One report indicated that an insulin level of 6.0 μU/mL during hypoglycaemia indicated abnormal insulin secretion [3]. Our patient’s laboratory data fulfilled the above criteria.
After the starvation test, she experienced fasting hypoglycaemia. She experienced hypoglycaemia after the 5-hour OGTT. The well-known clinical manifestation of insulinoma is fasting hypoglycaemia. However, postprandial hypoglycaemia may also be an evident feature or even the “sole” manifestation of hypoglycaemia in some patients [4]. A study reported that 21% of patients with insulinoma had both fasting and postprandial hypoglycaemia [4]. Some case reports reported insulinoma with postprandial hypoglycaemia [5,6]. In both cases, the serum IRI level was not suppressed; whereas, it was suppressed in our case. In this case report, we defined reactive hypoglycaemia as postprandial hypoglycaemia with suppressed insulin, and defined postprandial hypoglycaemia as postprandial hypoglycaemia without suppressed insulin. Both postprandial hypoglycaemia and reactive hypoglycaemia may occur in patients with insulinoma.
The effectiveness of the 5-hour OGTT in the diagnosis of insulinoma had long been mentioned [7]. More recently, a new report was published [8]. According to the study, the 5-hour OGTT can distinguish between insulinoma and reactive hypoglycaemia. Compared with reactive hypoglycaemia, the postprandial hypoglycaemia observed in insulinoma has higher ratios of serum concentrations of IRI and C-peptide to glucose. The model assuming an IRI to glucose ratio at 5-hour post load greater than 20.45 pmol/mmol is effective for insulinoma prediction. In our case, the IRI to glucose ratio at 5 hours post test was 7.38. The patient’s serum IRI level was suppressed. Considering the above criteria [2], her 5-hour OGTT data at pre operation did not align with that of insulinoma. We judged this case to be reactive hypoglycaemia. After the operation, 5-hour OGTT revealed that her reactive hypoglycaemia had vanished. In short, patients with insulinoma may have reactive hypoglycaemia, which can be improved by the resection of lesions.
Why did this occur in our case? To begin, the patient had Impaired Glucose Tolerance (IGT). It has been reported that the patients with IGT may suffer from reactive hypoglycaemia [9]. This explains why her serum IRI level was suppressed in spite of the insulinoma. In addition, improving her insulin secretory potential was important. Insulinogenic Index (II) is one of the parameters for pancreatic β-cell function II is calculated as the score of the IRI (μU/mL) at 30 minutes minus the fasting IRI divided by the plasma glucose level (mg/dL). An II level less than 0.4 suggests weak β-cell function [10]. The current case’s II level at pre operation was 0.25; in other words, her insulin secretory capacity had decreased. It is known that the normal β-cell function is suppressed in insulinoma [11]. After the operation, her II level had increased to 0.76, suggesting that her insulin secretory capacity had recovered. Establishing an appropriate insulin secretory capacity to normalise the glucose variation was effective in improving her reactive hypoglycaemia. Proinsulin might have been influenced; however, we did not test the serum proinsulin level in the present case. The possibility of this influence remains purely speculative, and further study will be necessary to confirm it.
Conclusion
Insulinoma causes fasting and postprandial hypoglycaemia via endogenous hyperinsulinism. Reactive hypoglycaemia may occur in patients with insulinoma. The 5-hour OGTT is useful for the diagnosis of insulinoma, but cannot completely rule out insulinoma even if reactive hypoglycaemia is observed. Reactive hypoglycaemia in patients with insulinoma may be improved through operation. The underlying mechanism is not well known, but the improvement of β-cell function may be influenced to suppress reactive hypoglycaemia. The clinical course of the current case supports the above hypothesis, thanks to the detailed data collected from the 5-hour OGTT at pre and post operation.
IRI: immunoreactive insulin; TSH: thyroid-stimulating hormone
Insulinogenic index = 0.25; IRI: immunoreactive insulin; OGTT: oral glucose tolerance test
*At 120 minutes, the patient’s glucose level was higher than 140 mg/dL. She had impaired glucose tolerance. At 240 and 300 minutes, she experienced hyperglycaemia. At that time, her serum IRI level was suppressed
Insulinogenic index = 0.76; IRI: immunoreactive insulin; OGTT: oral glucose tolerance test
*For 5 hours, the patient did not experience hypoglycaemia. At 120 minutes, her glucose level was lower than 140 mg/dL. Her appropriate insulin secretory potential was recovered
[1]. Service FJ, McMahon MM, O’Brien PC, Ballard DJ, Functioning insulinoma-incidence, recurrence, and long-term survival of patients: a 60-year studyMayo Clin Proc 1999 66(7):711-19.10.1016/S0025-6196(12)62083-7 [Google Scholar] [CrossRef]
[2]. Cryer PE, Axelrod L, Grossman AB, Heller SR, Montori VM, Seaquist ER, Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice GuidelineJ Clin Endocrinol Metab 2009 94(3):709-28.10.1210/jc.2008-141019088155 [Google Scholar] [CrossRef] [PubMed]
[3]. Service FJ, Hypoglycemic disordersNew Engl J Med 1995 332(17):1144-52.10.1056/NEJM1995042733217077700289 [Google Scholar] [CrossRef] [PubMed]
[4]. Placzkowski KA, Vella A, Thompson GB, Grant CS, Reading CC, Charboneau JW, Secular trends in the presentation and management of functioning insulinoma at the Mayo Clinic, 1987-2007J Clin Endocrinol Metab 2009 94(4):1069-73.10.1210/jc.2008-203119141587 [Google Scholar] [CrossRef] [PubMed]
[5]. Iida K, Ohara T, Hino Y, Nobuhara M, Ishida J, Chihara K, Glucose-responsive insulinoma in a patient with postprandial hypoglycemia in the morningIntern Med 2010 49(19):2123-27.10.2169/internalmedicine.49.385420930440 [Google Scholar] [CrossRef] [PubMed]
[6]. Shreenivas AV, Leung V, A rare case of insulinoma presenting with postprandial hypoglycemiaAm J Case Rep 2014 15:488-91.10.12659/AJCR.89133625381469 [Google Scholar] [CrossRef] [PubMed]
[7]. Konng YG, Value of 5-hour glucose tolerance test in the diagnosis of insulinomaZhonghua Wai Ke Za Zhi 1990 28(6):331-32. [Google Scholar]
[8]. Li X, Zhang F, Chen H, Yu H, Zhou J, Li M, Diagnosis of insulinoma using the ratios of serum concentrations of insulin and C-peptide to glucose during a 5-hour oral glucose tolerance testEndocr J 2017 64(1):49-57.10.1507/endocrj.EJ16-029227725372 [Google Scholar] [CrossRef] [PubMed]
[9]. Hofeldt FD, Reactive hypoglycemiaEndocrinol Metab Clin North Am 1989 18(1):185-201.10.1016/S0889-8529(18)30396-7 [Google Scholar] [CrossRef]
[10]. Kosaka K, Kuzuya T, Hagura R, Yoshinaga H, Insulin response to oral glucose load is consistently decreased in established non-insulin-dependent diabetes mellitus: the usefulness of decreased early insulin response as a predictor of non-insulin-dependent diabetes mellitusDiabet Med 1996 13(Suppl 9):S109-S19.10.1002/dme.1996.13.s6.109 [Google Scholar] [CrossRef]
[11]. O’Hare MMT, Shaw C, Swanston-Flatt SK, Marcelli M, Buchanan KD, Flatt PR, Influence of a transplantable insulinoma on the pancreatic status of insulin and pancreatic polypeptide in the ratDiabetologia 1985 28:157-60. [Google Scholar]