Acute urinary retention secondary to BPH is a urological emergency characterised by inability to pass urine which is of sudden onset and is associated with pain. In clinical practice, the AUR associated with BPH is known as spontaneous AUR. There are several risk factors which have been identified in different studies. These are advanced age, severe LUTS, low peak flow rate, high PVR, enlarged prostate volume and raised serum Prostate-Specific Antigen (PSA) [1,2]. When the AUR develops due to a precipitating event it is known as precipitated AUR. The conditions which can precipitate AUR are non-prostate related surgery, regional anaesthesia, urethral catheterisation, and excessive fluid intake, urinary tract infection and intake of medications such as anticholinergics, antihistaminics or sympathomimetics [3].
The management of AUR is immediate urethral catheterisation. If per-urethral catheterisation fails, then suprapubic catheterisation is the next step. In the past, early surgery was the first approach and it was safer also as it could avoid prolonged catheterisation [4]. Long-term catheterisation (either per-urethral or suprapubic) was the second approach but with the disadvantages like haematuria, urinary leakage, bladder calculus, urosepsis associated with it. The third approach was the TWOC with medication in the form of alpha blocker. The TWOC is the current standard practice worldwide because it is advantageous to the patient when it is successful. It was associated with reasonably good success rate of 23-40% [5].
Studies have shown old age (≥70 years), prostate size ≥50 mL, severe LUTS, drained volume at catheterisation ≥1 litre, IPP and spontaneous AUR to be the predictors for unsuccessful outcome of TWOC [6]. This study was done to evaluate the factors predicting outcome of TWOC in patients with AUR due to BPH. It also identifies the subset of patients unlikely to benefit from this treatment so that early definitive treatment can be provided.
Materials and Methods
Study Design
Prospective observational study was conducted from March 2015 to November 2016. Approval was taken from the Ethical Committee of the institution.
Study Place
The study was conducted in the department of Urology, RG Kar Medical College and Hospital, Kolkata, West Bengal, India.
Inclusion and Exclusion Criteria
A total of 128 male patients with AUR secondary to clinical diagnosis of BPH, attending the emergency department were enrolled for the study. Written informed consent was taken from all the patients. About 38 patients were excluded from the study because of backpressure changes in six, prior failed history of TWOC in seven, recurrent haematuria in three, recurrent UTI in nine, history of neurological illness in five or recent use of five α-reductase inhibitors, tricyclic antidepressants, anticholinergics, sympathomimetics, or first-generation antihistamines in eight patients. Rest of the 90 patients were included in the study.
Data Collection
Detailed clinical history and examination including DRE was performed. All patients were catheterised via the urethra, Residual Urine Volume (RV) drained after catheterisation was recorded, and urine was collected for urinalysis. USG of Kidney, Urinary Bladder and Prostate (KUBP) was done after relief of retention. Tablet Tamsulosin 0.4 mg was advised orally once daily for three days. Catheter was removed in the Urology department of R G Kar Medical College and Hospital under all aseptic conditions on fourth day morning and patients were observed for six hours for urination. Uroflowmetry and PVR urine measurement by USG were done in patients able to pass urine. Patients failing to pass urine were recatheterised. The TWOC was considered successful if the patient voided within six hours of catheter removal with a maximum flow rate >5 mL/second and PVR <200 mL. We considered ultrasonographic intravesical prostatic protrusion of <5 mm, 5-10 mm, >10 mm as Grade I, II, III respectively.
Statistical Analysis
Analysis was performed with the available version of standard statistical software SPSS version 20.0. It was considered statistically significant when the p-value <0.05. Logistic regression analysis was done to identify the predictive factors for the outcome of TWOC. Chi-square test was used to test the association between categorical variables and it was a distribution free test. Shapiro Wilk, Kolmogorov Simonov were done to test the normality of a variable and if it was found to be not normally distributed then non-parametric tests were performed for subsequent analysis. The ROC was prepared to determine the cut off value of factors like duration of LUTS, drained urinary volume and prostate volume (ultrasound) for predicting the outcome of TWOC.
Results
The baseline characteristics of the study were the mean age of the patients in the successful group was 65.41±7.134 years (p=0.026) and that in the failure group was 64.82±10.177 years (p=0.006), the mean duration of LUTS in the successful group was 7.22±9.626 months (p=0.000) and in the failure group was 9.74±9.904 months (p=0.000), the mean drained urinary volume post catheterisation in the successful group was 749±172.189 mL (p=0.000) and that in the failure group was 883.33±125.831 mL (p=0.007).
A total of 90 patients with age ranging from 46 to 95 years were enrolled for the study and the mean age of the patients was 65.16±8.53 years. The duration of LUTS of the patients ranged from one month to 48 months and the mean value was 8.31±9.773 months. The patients had drained urinary volume ranging from 500 mL to 1100 mL and the mean value was 807.22±167.023 mL. The ultrasonographically measured prostate volume ranged from 26 mL to 105 mL and the mean value was 58.87±15.980 mL. Among the 90 patients, 87.78% (79) had thickened bladder wall and rest were having normal bladder wall. After measuring the IPP of the patients, it was observed that 33.3% (30), 42.2% (38), 24.4% (22) of them had Grade I, II, III intravesical prostatic projection respectively.
A successful trial without catheter was observed in 56.7% (51) of the patients.
Grade I BPH on DRE is appreciated as easy accessibility of upper limit of prostate, Grade II as accessibility of upper limit with effort and Grade III as accessibility of upper limit with marked difficulty. After analyzing the DRE prostate size, we found 10% (9) patients with Grade I, 75.6% (68) with Grade II and 14.4% (13) with Grade III prostate. It was also observed that 66.7% cases (6 out of 9) of Grade I, 58.8% cases (40 out of 68) of Grade II and 38.5% cases (5 out of 13) of Grade III had successful TWOC.
The bladder wall thickness was measured in all the patients with the help of ultrasound and they were marked as thickened if the wall thickness was ≥5 mm. Among 51 patients in the successful group 80.4% (41) had thickened bladder wall and in the failure group, it was 97.4% (38) among 39 patients. Almost all the patients in the failure group were having urinary bladder wall thickened in ultrasound and it was statistically significant also (p=0.014).
The prostate volume was measured by taking all the parameters on ultrasound and analyzed by the formula (height × width × antero posterior diameter × 0.52). The mean prostate volume in the successful group was 56.8±17.495 mL (p=0.090) and the same for the failure group was 61.4±13.535 mL (p=0.079).
It was also observed that the failure rate of TWOC was 10% (three out of 30), 52.6% (20 out of 38) and 72.7% (16 out of 22) for Grade I, II, III IPP respectively. After determining the odds ratio it was seen that failure rate of Grade III was 18.9 times that of Grade I and 1.13 times that of Grade II. So, IPP had a significant influence on the outcome of TWOC (p=0.001).
Multiple regression analysis were performed to identify the predictive factors of outcome of TWOC adjusting the confounding variables and it was found that IPP (p=0.002) and drained urinary volume (p=0.001) were the significant predictive factors. Other factors like age, duration of LUTS, thickened bladder wall, prostate volume were also analyzed although their values were not statistically significant (p>0.05) [Table/Fig-1].
Multiple regression analysis of the compounding variables of the equation.
| Variables | B | df* | Sig.# | Exp (B)§ | 95% CI for Exp (B) |
|---|
| Lower | Upper |
|---|
| Age | -0.026 | 1 | 0.446 | 0.974 | 0.910 | 1.042 |
| Duration of LUTS | 0.024 | 1 | 0.472 | 1.024 | 0.959 | 1.094 |
| USG UB wall (1) | 2.203 | 1 | 0.080 | 9.055 | 0.766 | 107.028 |
| USG prostate volume | 0.008 | 1 | 0.660 | 1.008 | 0.972 | 1.046 |
| USG IPP | - | 2 | 0.002 | - | - | - |
| USG IPP (1) | -2.939 | 1 | 0.001 | 0.053 | 0.009 | 0.304 |
| USG IPP (2) | -0.127 | 1 | 0.852 | 0.881 | 0.232 | 3.350 |
| Drained urine volume | 0.007 | 1 | 0.001 | 1.007 | 1.003 | 1.011 |
| Constant | -5.786 | 1 | 0.083 | 0.003 | - | - |
*Degree of freedom
#Significance
§Exponential of B
CI- Confidence Interval
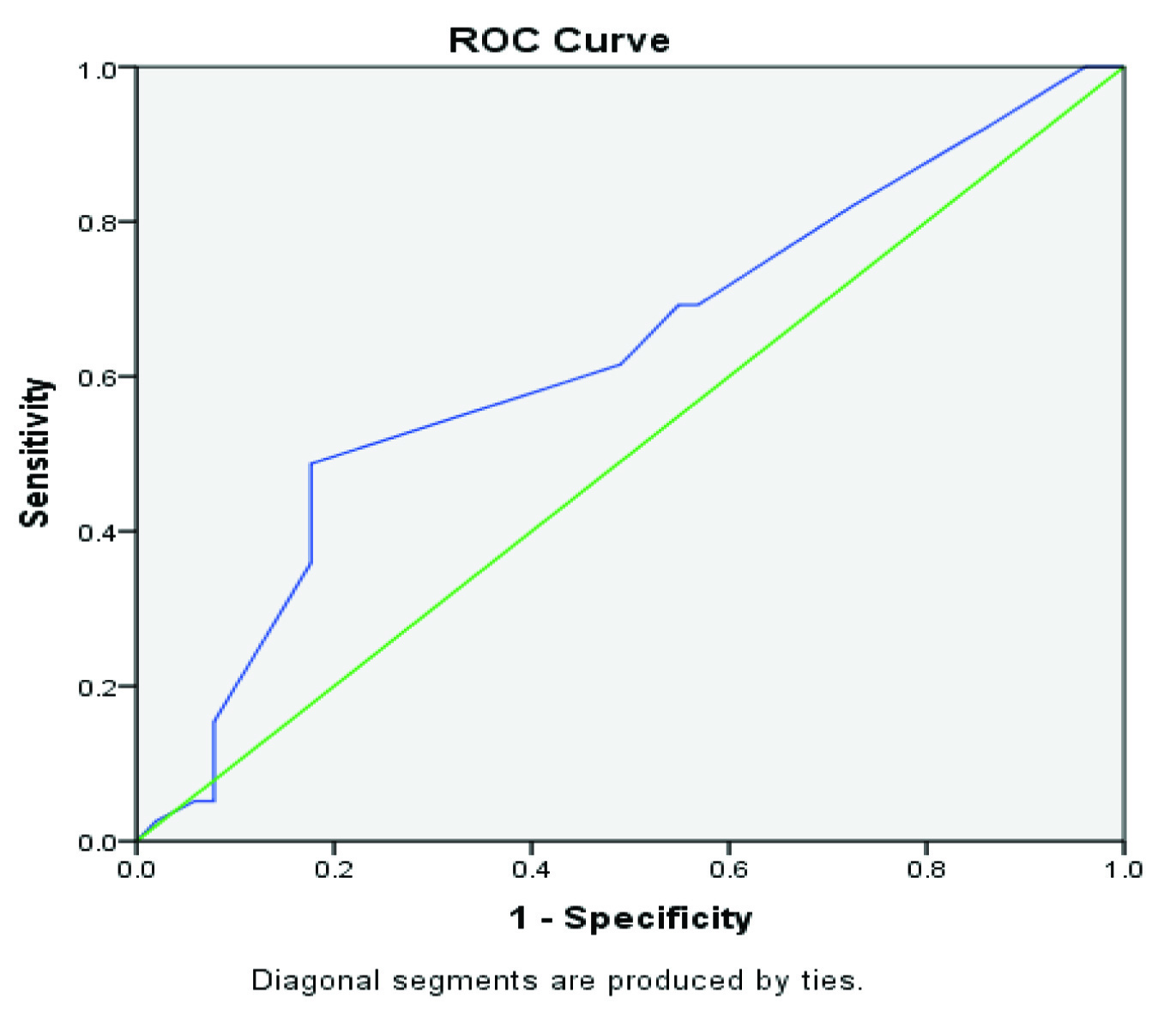
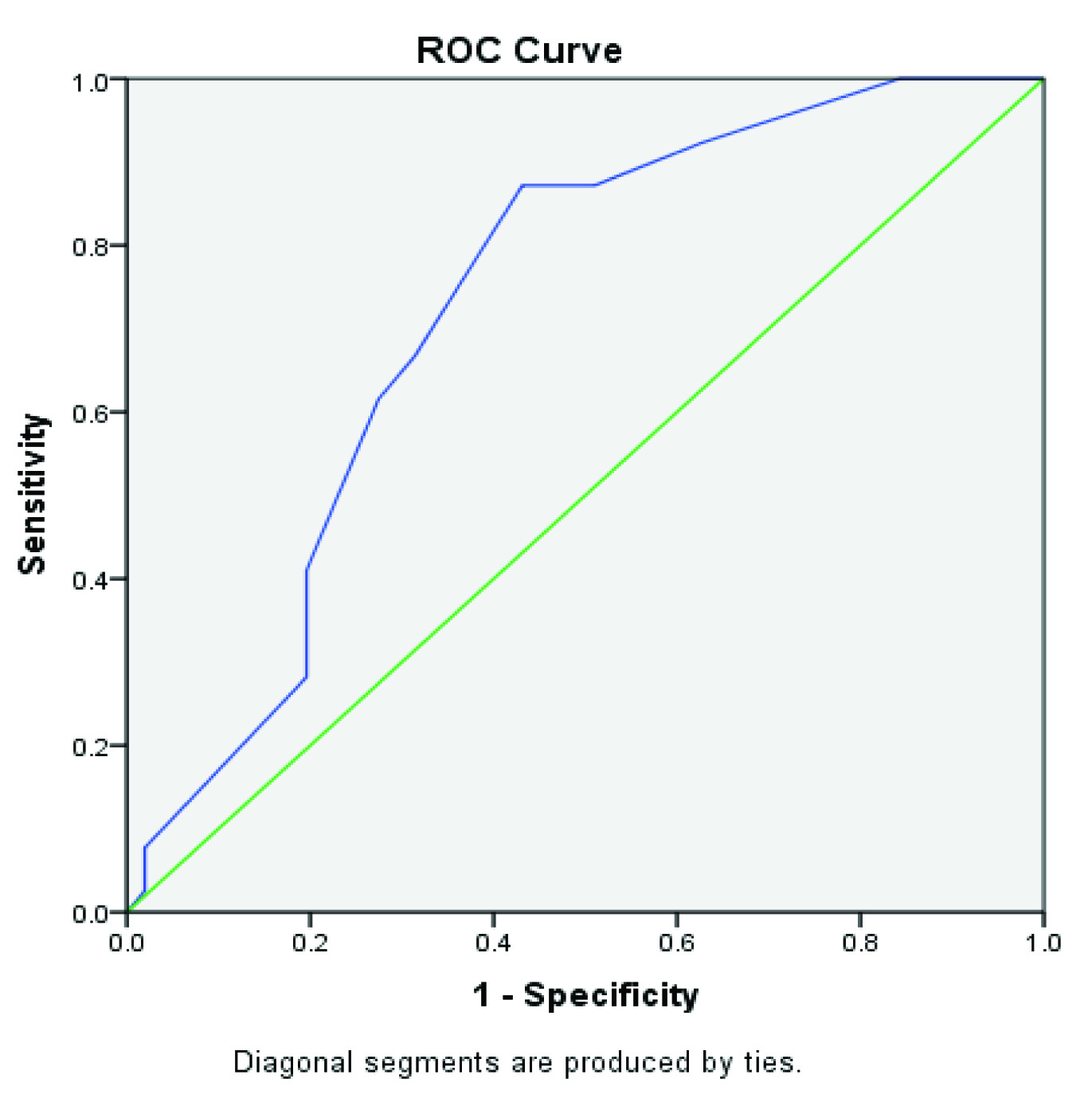
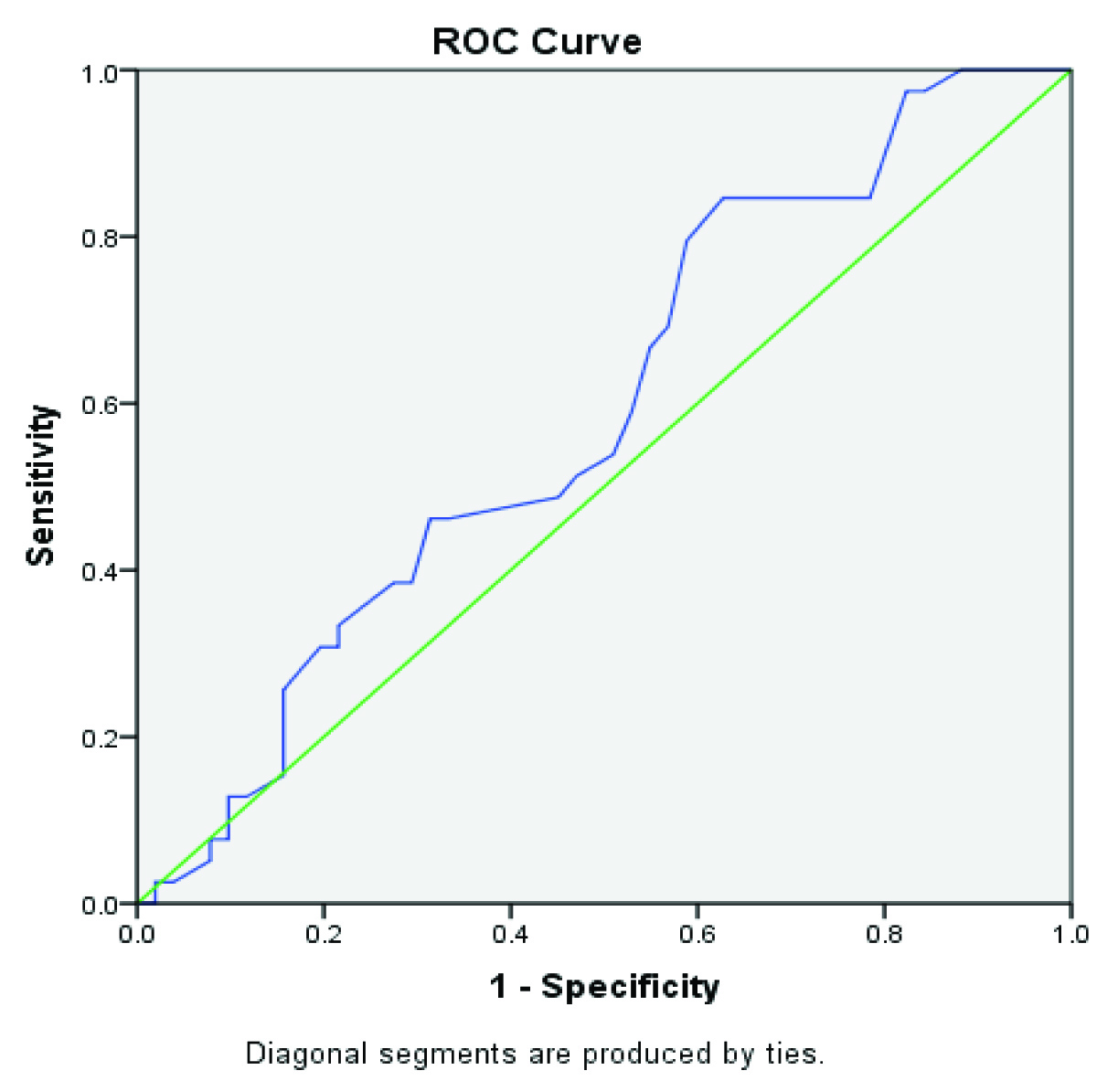
It was observed that a cut-off of two and a half months for duration of LUTS detected TWOC failure with a sensitivity of 82.1% with area under the ROC was 0.625 [Table/Fig-2]. A cut-off value of 775 mL for drained urinary volume (post catheterisation) detected TWOC failure with a sensitivity of 87.2% (area under ROC=0.726) [Table/Fig-3]. A cut-off value of 49.5 mL for prostate volume on USG detected failure with a sensitivity of 84.6% and area under the ROC was 0.588 [Table/Fig-4].
ROC curve for cut-off of duration of LUTS.
ROC curve for cut-off of drained urine volume.
ROC curve for cut-off of prostate volume on ultrasound.
Discussion
The success rate of TWOC in our study was 56.7% which is similar to most of the observational studies where success rates range from 48 to 62% [7-11]. Another study stated that TWOC after a median of three days of catheterisation has become standard practice in France for men with BPH and AUR [8]. In our study, we considered TWOC in our patients after three days of catheterisation with good success rate.
In a large Reten study, patients of less than 70 years of age were associated with a successful TWOC [6]. Alfaur study also reported that higher rate of failed TWOC in men aged >65 years of age [12]. In our study, our mean age of successful TWOC patients was 65 years (61years for the failed patients). However, our results were similar to the Malaysian study which concluded that age of patients had no significant influence on the outcome of TWOC [13].
Our study found marginally significant correlation between duration of LUTS less than two and a half months and successful TWOC. Another study found significant marginal correlation between less than three months of duration of LUTS and successful TWOC [14]. In the largest international study to date, 63% reported LUTS previously [15].
We found a significant correlation of the drained urinary volume with failure of TWOC and our cut-off value was 775 mL (p=0.001). Lim KB et al., reported that 79 men with first spontaneous AUR due to BPH for which residual volume of more than 800 mL correlated with failure of TWOC but no statistical significance was noted [16]. In the Reten study univariate analysis showed that residual volume of less than 1000 mL was associated with a successful TWOC (p<0.001) and this was confirmed by results of multivariate analysis [6].
We have found a marginally significant correlation (p=0.162) of increasing success of TWOC as the clinical prostate gland size decreased. Another study obtained similar result where 68.42% of Grade I, 44.83% of Grade 2, and 40% of Grade 3 had successful TWOC (p=0.097) [14]. In the Reten study, estimates of prostate size were based on DRE alone, univariate regression analysis for trial at a median of 5 days (41.3% for <3 days) showed that size of <50 g was associated with a successful TWOC (p<0.001).
None of the studies has described bladder wall thickness as a factor for predicting outcome of TWOC in patients with AUR due to BPH. In our study, almost all (97.4%) of the patients who failed TWOC had bladder wall thickened on ultrasound and it was statistically significant (p=0.014). Multiple regression analysis also identified it as a predictive factor for outcome of TWOC although, it was not statistically significant (p=0.08).
In one study [14], 62.07% of the patients with prostate volume of less than 45 mL had a successful trial and 39.29% of cases with a prostate volume more than 45 ml had an unsuccessful trial. In another study, Bhattachan CL and Bhomi KK reported prostate size of 40 gm on transabdominal ultrasound to predict the outcome of TWOC with a specificity of 73% and a sensitivity of 84% [17]. In our study, 49.5ml of prostate volume was the cut-off above which there was a high chance of TWOC failure.
In our study 10% of cases of Grade I, 52.6% cases of Grade II and 72.7% cases of Grade III IPP failed TWOC. The failure rate of Grade III IPP was 18.9 times that of Grade I IPP and 1.13 times that of Grade II IPP. Similar results was found in other three studies, one of them revealed that a cut-off of 8.2 mm for intravesical prostatic protrusion detected failures of TWOC with a specificity of 87% and successes with a specificity of 64% [18], another study showed that men with an IPP of 10 mm or less compared to those with a larger IPP were six times more likely to have a successful trial without catheter [19], other one revealed that Grade III IPP is a strong predictor in the failure of outcome of TWOC [13].
Limitation
The limitation of our study was that the number of patients with Grade III IPP was less compared to that with Grade I or II IPP and this could have been improved by increasing the duration and selecting more number of cases for the study.
Conclusion
Duration of prior LUTS, drained urinary volume, DRE prostate size, thickened bladder wall, prostate volume on ultrasound and IPP are predictive factors of the outcome of TWOC in patients with AUR due to BPH but the statistically significant ones among them are IPP and drained urinary volume. Age is not a significant factor for predicting outcome of TWOC in patients with AUR secondary to BPH.
*Degree of freedom
#Significance
§Exponential of B
CI- Confidence Interval