Case Series
Focal Fibrous Hyperplasia
Case 1: A 45-year-old female presented with an overgrowth on buccal aspect of 32 and 33, of two months duration. Patient had a history of trauma due to food impaction at the site approximately two months back. Clinical examination revealed pinkish red, sessile overgrowth which was firm in consistency [Table/Fig-1a].
Solitary, nodular growth noted on a) Gingiva; b) Palate; c) Right lateral border of tongue and; d) Buccal Mucosa diagnosed as FFH; e) Photomicrograph of Case 4 (FFH) demonstrating parakeratinised stratified squamous epithelium covering a fibrous connective stroma. (H&E, 40X).
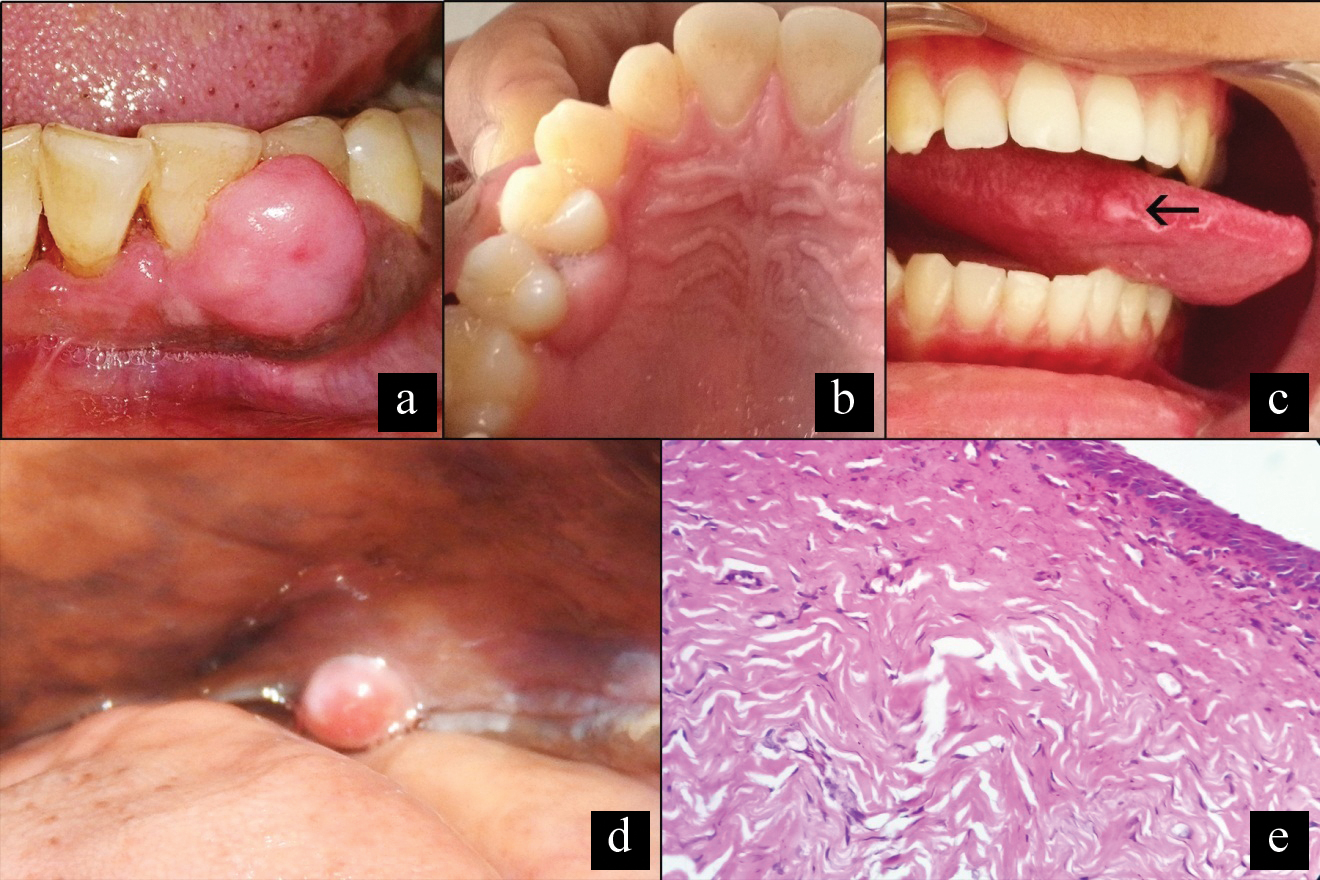
Intraoral radiograph did not show any abnormalities. Excisional specimen was sent for histopathological examination, H&E stained sections demonstrated moderately dense collagenous connective tissue covered by parakeratinised epithelium of variable thickness. Thick collagen bundles were noted focally. Based on clinical and histological features, the diagnosis of FFH was established. The case was followed up for one year; no recurrence was reported.
Case 2: A 36-year-old male presented with a growth present on palate from the last 15 days. Patient gave a history of tooth pick trauma at the site 10-12 days back. Clinical examination revealed pinkish red, flaccid overgrowth which was firm in consistency [Table/Fig-1b]. Intaoral radiograph did not show any abnormalities. Excisional specimen was sent for histopathological examination. H&E stained slides showed stratified squamous surface epithelium supported by fibrocellular connective tissue. Thick bundles of collagen with spindle shaped fibroblasts were noted. Diffuse moderate inflammatory cell infiltrate was also noted. Based on clinicopathological correlation, the diagnosis of FFH was rendered. The patient was followed up for six months, recurrence was not noted.
Case 3: A 22-year-old female visited our institute with the chief complaint of a nodule on lateral border of tongue since two years. Clinical examination revealed red, ulcerated overgrowth on right lateral border of anterior two-third of tongue [Table/Fig-1c]. Excisional biopsy was performed and the tissue was sent for histopathological examination. H&E slides revealed dense fibrocellular connective tissue covered by parakeratinised stratified squamous epithelium. Dense bundles of collagen were noted. The diagnosis of FFH was established by taking into account both clinical and histological features. The patient did not show recurrence at six months of follow up.
Case 4: A 59-year-old male presented with a nodular mass present on left posterior buccal mucosa, of six months duration. Patient gave a history of tobacco consumption since 20 years, three to four times a day. Clinical examination revealed pinkish red, pedunculated overgrowth which was firm in consistency [Table/Fig-1d]. On intraoral radiograph no abnormalities were evident. Histopathological examination revealed a stretched out surface epithelium and underlying dense fibrous connective tissue. Thick bundles of collagen interspersed with spindle fibroblasts were present throughout. Diffuse mild chronic inflammatory cell infiltrate was noted [Table/Fig-1e] with clinicopathological correlation the lesion was diagnosed as FFH. The patient was followed up for one year.
Pyogenic Granuloma
Case 5: A 59-year-old female presented with a round or oval overgrowth present on palate of six months duration. Clinical examination revealed pinkish red, sessile overgrowth which showed bright red areas as areas of proliferation [Table/Fig-2a].
Reddish pink, pedunculated growth noted on palate: a) Labial aspect of gingiva; b and c) Diagnosed as PG; d) Photomicrograph of case 7(PG) demonstrating fibrovascular connective tissue composed of numerous vascular channels, chronic inflammatory cell infiltrate and extravasated RBCs. (H&E 10X) Inset shows higher magnification of engorged vascular channels. (H&E 40X).
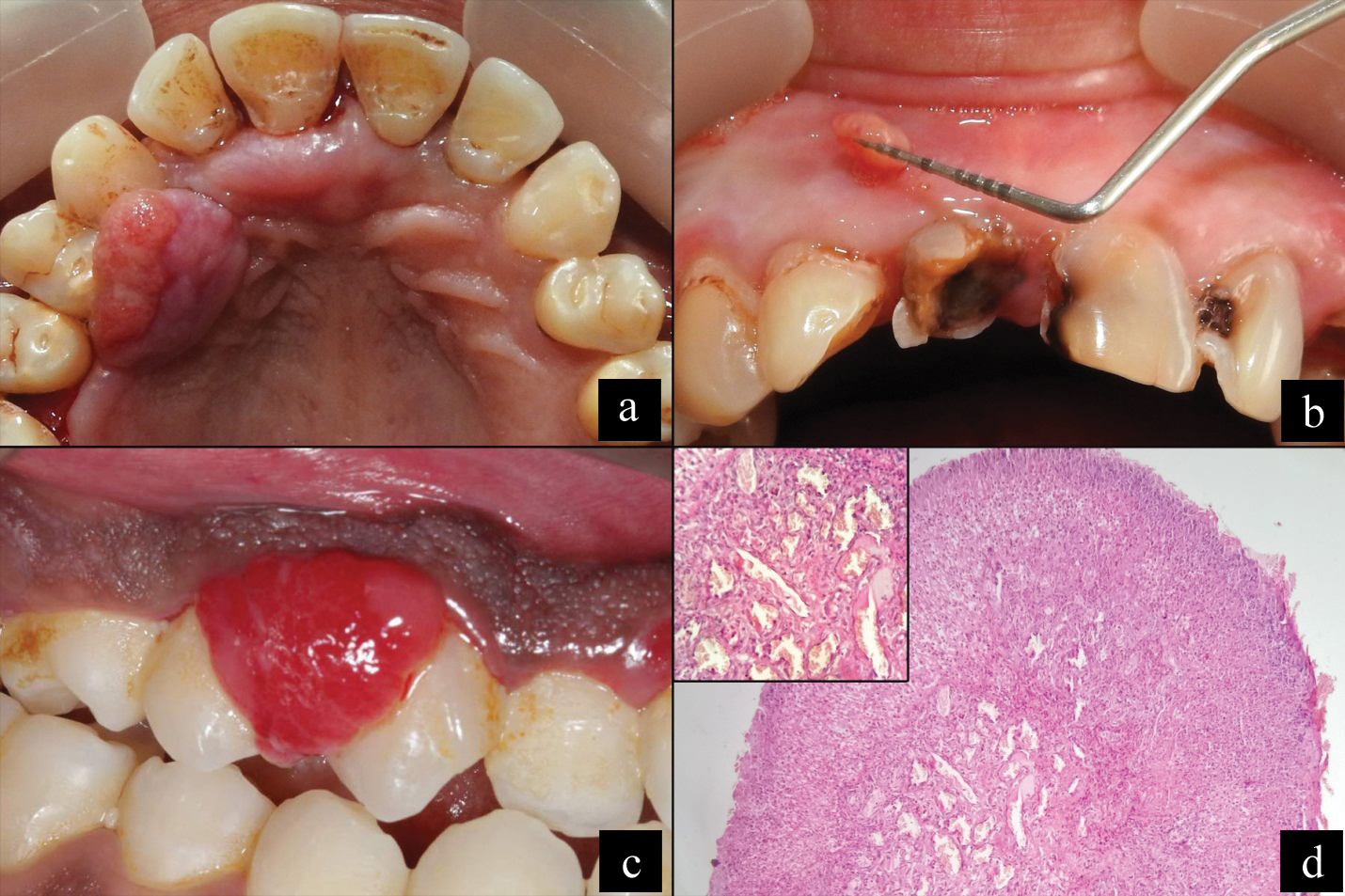
Intraoral periapical radiograph did not reveal any abnormalities. Excision was done, histopathological examination revealed, a highly vascular tissue lined by discontinuous surface epithelium. Numerous endothelium lined blood vessels engorged with RBCs were noted in connective tissue; Thus, diagnosis of PG was established. The patient was followed up for 10 months, recurrence was not noted.
Case 6: A 45-year-old female presented with a small overgrowth present on buccal aspect of maxillary anterior gingiva since six months. Clinical examination revealed pinkish red, pedunculated overgrowth [Table/Fig-2b]. The lesion was excised and sent for histopathological diagnosis. Ulcerated surface epithelium was noted and the connective tissue was highly vascular with numerous endothelium lined blood vessels. Extravasated RBCs and diffuse chronic inflammatory cell was noted. The case was followed up for eight months and the lesion did not show recurrence.
Case 7: A 31-year-old female presented with an overgrowth present on buccal aspect of 13, 14, since 20 days. Clinical examination revealed red, pedunculated, lobulated overgrowth [Table/Fig-2c]. Excisional biopsy was performed. On histopathological examination, fibrovascular stroma covered with discontinuous surface epithelium replaced by fibropurulent membrane was evident. Numerous vascular channels with endothelial proliferation, areas of hemorrhage and chronic inflammatory infiltrate were noted [Table/Fig-2d]. The lesion was followed up for nine months. No recurrence noted.
Peripheral Ossifying Fibroma
Case 8: A 39-year-old female presented with an overgrowth present on buccal aspect of 42, 43, of one month duration. Clinical examination revealed pinkish red, pedunculated overgrowth with lobulated surface [Table/Fig-3a]. Radiograph did not reveal any abnormalities. Excisional biopsy was performed. On histopathological examination parakeratinised stratified epithelium with long and slender rete ridges was noted. Epithelium was supported by fibrocellular stroma exhibiting thick bundles of collagen fibers interspersed with plump fibroblasts.
Solitary lobulated, pedunculated growth on labial aspect of gingiva: a) diagnosed as POF; b) Photomicrograph of case 8 (POF) demonstrating parakeratinized stratified squamous epithelium covering a fibrocellular connective stroma with discrete calcifications. Inset shows higher magnification of ostoid lined by osteoblasts (H&E 40X).
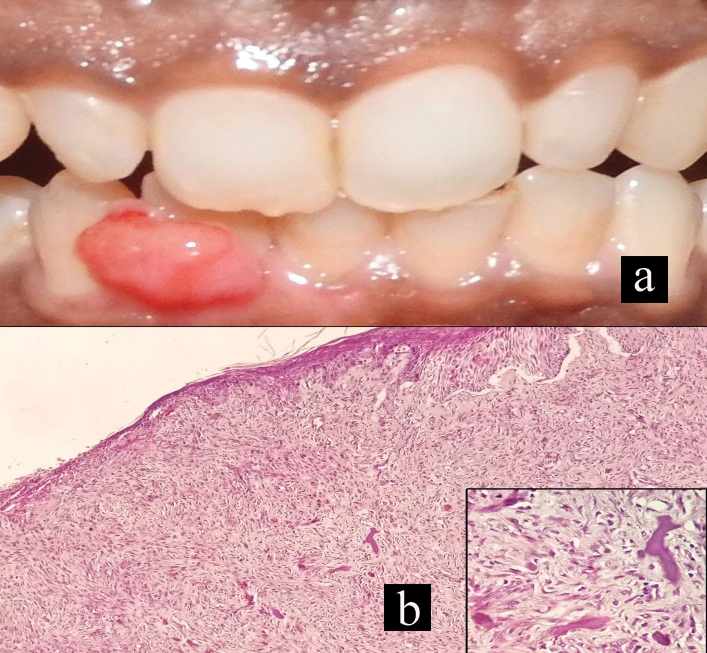
Focally mineralised component was noted resembling osteoid lined by osteoblasts [Table/Fig-3b]. After Histopathological examination of Peripheral Ossifying Fibroma (POF) was rendered. The lesion recurred in two months. Careful excision was carried out and histological features of the recurred excised specimen were similar to the earlier biopsy sample. The patient was followed up for one year. No further recurrence was noted.
Discussion
Oral mucosa is constantly subjected to chemicomechanical insults resulting in the variety of mucosal lesions [1]. All the gingival overgrowths were historically referred to as “Epulides” [2]. These overgrowths are most commonly occurring mucosal lesions [3]. Kfir Y et al., classified reactive hyperplasic lesions as PG, PGCG, POF and FH [3]. Daley TD et al., suggested the term FROG for these lesions [4]. Recently, Puranik RS et al., suggested the abbreviation “FROG” for the same [5].
Focal Reactive Overgrowths have different clinical and histological appearance than other inflammatory enlargements [6]. All these lesions are a response to chronic, low-grade stimulus caused by plaque, calculus, or any other irritant [7]. FROGs are usually associated with poor oral hygiene, indicating towards their reactive nature [8]. All FROG have similar aetiology and clinical features, but their histological appearance varies according to the intensity of irritation, duration of the lesion and other factors [5].
Focal Reactive Overgrowths are more common in females; thus, implicating the role of female hormones in the pathogenesis of FROG [3]. Clinically, the lesions under FROGs have many overlapping characteristics and usually are either sessile or pedunculated [9]. The most commonly affected site is gingiva, typically in the maxillary anterior region [8]. FROGs may occur on gingival as well as extragingival sites. It is important to note that POF and PG may occur at extra-gingival sites but POF and PGCG are strictly restricted to gingiva [9]. Histopathologically, FROGs represent a spectrum, wherein FFH and POF are predominantly fibrous and PG and PGCG have fibrous as well as endothelial component [5]. Histopathological investigations are mandatory to validate the clinical diagnosis of FROGs [10].
Focal fibrous hyperplasia: FFH is most common among FROG’s accounting for about 57-62% of cases [1]. These lesions may serve as end stage for some epulides like angiogranulomas [1]. Literature suggests gingiva to be most common site followed by buccal mucosa [1,3,8,9,11]. The lesion is usually asymptomatic [1]. Female predilection has been attributed to increased production and accumulation of collagen by fibroblasts, in the presence of a chronic injury under the influence of female hormones [12]. FFH exhibits limited growth potential. FFH needs to be differentiated from Giant Cell Fibroma (GCF) [13]. GCF is characterised by the presence of plump, giant and spindle/stellate fibroblasts, juxtaepithelially [13].
Pyogenic granuloma: Hartzell in 1904 coined the term PG [7]. The term is a misnomer since, clinically there is no evidence of purulent material and histopathologically it is not a granuloma [7]. It is the second most common FROG which accounts for almost 18-23% of all cases [1,6]. Around 5% of pregnant women present with PG, typically during second or third trimester [4,7]. Daley TD et al., demonstrated a positive relation between serum progesterone and PG [4]. They suggested that increased hormonal levels may render oral mucosa susceptible to chronic irritation by local factors thus, increasing its incidence [4]. Presence of inclusion bodies in papillary fibroblasts of PG which result from C-type virus infection has been noted, suggesting that a disordered protein metabolism could be another possible aetiology [7]. The differential diagnoses of PG include haemangiomas, metastatic tumours, Kaposi sarcoma, bacillary angiomatosis etc. Histopathological examination aids in differentiating them from PG [7].
Peripheral ossifying fibroma: POF is the third most common FROG accounting for about 27% cases. POF occurs more commonly in younger age group mostly in second and third decade [8]. The exclusive occurrence of POF on the gingiva, the presence of oxytalan fibers interspersed among the calcified deposits and fewer incidences in older age (due to loss of permanent teeth) indicate that POF originates from the periodontal ligament [14]. The presence of cells capable of forming cementum and bone in PDL warrants aforementioned statement [8]. The clinical implication of POF is its high recurrence rate (8-45%) [14]. A similar finding was observed in POF in the present case series, which recurred two months after excision. The similarity in the terminologies of POF and ossifying fibroma may evoke some confusion. However, ossifying fibroma is a true neoplasm which is essentially intraosseous, whereas POF is a reactive lesion occurring strictly on gingiva [14]. Hence, the term POF is a misnomer and we suggest the use of term fibrous hyperplasia with calcification for the same.
Peripheral giant cell granuloma: PGCG is the least common of all four with occurrence up to 6.22% among all cases [1]. In contrast to other lesions under FROG, PGCG is common in elder age group [11]. PGCG is thought to arise from multinucleated giant cells derived from osteoclasts left from physiologic resorption of teeth or as a reaction to periodontal injury [15]. As some of the PGCG may show “cupping” superficial resorption of the underlying alveolar bony crest; it should be differentiated from a central giant cell granuloma eroding through the cortical plate into the gingival soft tissues [15]. The comparison of all the lesions under FROG is depicted in [Table/Fig-4].
Key differences between FROGs.
| Parameters | FFH | PG | POF | PGCG |
|---|
| Age (years) | 31-40 years (42.8) [11] | 18-40 years (33.9) [11] | 21-30 years (41.3) [11] | 12-66 years (43.2) [11] |
| Sex (M:F ratio) | 1:1.31 [11] | 1:2.25 [11] | 1:1.58 [11] | 1:1.07 [11] |
| Site | Mandibular gingiva [1] | Equally in maxillary and mandibular anterior region [3] | Maxillary anterior gingiva [1] | Mandibular posterior buccal area [3] |
| Clinical Presentation | Firm pink, non inflamed mass usually growing under free gingival margin or interdental papilla [6] | Smooth surfaced, characteristically reddish pink in color, compressible [6] | Nodular mass either pedunculated or sessile, pink to red colored and surface is usually but not always ulcerated [6] | Purplish red cyanotic color. Most aggressive of FROGs. Erosion of cortical bone is usually seen [6] |
| Histological presentation | Reactive fibroblastic proliferation. Discrete and polypoid but non-encapsulated. Epithelium may be ulcerated [6] | Ulcerated fibrovascular lesion composed to numerous blood vessels with endothelial proliferation. [6,7]. Histopathological variants: 1. LCH type 2. Non LCH type | Foci of discrete irregular dystrophic calcification. Cementicles/bony trabacule may be found [6] | Variable number of multinucleated giant cells interspersed amongst the mononuclear cells which derived from monocytes.The stroma is fibrovascular [6] |
| Treatment | Surgical excision [1] | Surgical excision [1] | Surgical excision [1] | Surgical excision [1] |
| Recurrence | Rare [1] | Very rare [1] | Rare [1] | Very rare [1] |
FFH-Focal Fibrous Hyperplasia; PG-Pyogenic Granuloma; POF-Peripheral Ossifying Fibroma; PGCG-Peripheral Giant Cell Granuloma; LCH: Langerhans Cell Histiocytosis
The differential diagnoses of FROGs include infective periapical diseases/periodontal abscess, tumours like peripheral odontogenic tumours, various benign and malignant connective tissue tumours and metastatic tumours of the jaws [8]. The differential diagnoses of FROGs are depicted in [Table/Fig-5]. Thus, segregating the lesions of FROGs will not only facilitate their differentiation from other lesions but also aid in their diagnosis and treatment.
Differential diagnosis of gingival overgrowths.
| S. No. | Gingival overgrowths | Site | Clinical features | Histopathological features |
|---|
| 1 | FROG | Anterior maxillary and mandibular gingiva | Lesions included are FFH, PG, POF, PGCG isolated overgrowths seen on marginal gingiva to attached gingiva. Also, seen on extragingival sites. Develop in response to low grade stimulus | Varies on maturation of lesion, i.e., from fibrous to predominant proliferated endothelial component and calcified material like osteoid and cementum. PGCG contains giant cells. |
| 2 | Haemangioma [7] | Tongue | Bluish red in colour.Diascopy-applying pressure to suspected area to visualise colour change | In contrast to PG, it has more plump histiocytoic cells and endothelial proliferation in absence of acute inflammatory infiltrate |
| 3 | Periapical abscess/ Periodontal abscess [10] | Localised, predilection for maxilla | Periapical abscess- associated with non vital tooth, radiolucent area observed along apex of rootPeriodontal abscess- Diffuse and extends to attached mucosa | Purulent material in connective tissue, dense infiltration of neutrophils and vascular engorgement |
| 4 | Pregnancy tumour [7] | Maxillary attached gingiva | Seen more frequently in third trimester of pregnancy | Histopathologically same as that of PG. |
| 5 | Drug induced enlargement [10] | Generalised, prominent in maxillary and mandibular anterior region | Associated with use of drugs like calcium channel blockers, anti epileptic drugs and immune-suppressants | Long rete ridges, increased chronic infiltrate and increased vascularity |
| 6 | False enlgargement [10] | Generalised | Result of excessive bony growth.No abnormal clinical growth other than growth in size. e.g.,- tori, cherubism | Usually normal gingival tissue with or without inflammatory component |
| 7 | Vitamin C deficiency [10] | Generalised | Seen when Vitamin C levels are < 2μ/mL Bluish red, soft with a shiny and smooth surface.Spontaneous bleeding | Hs-CRP level may be significantly elevated |
| 8 | Hereditary enlargement [10] | Generalised | Syndrome associated gingival growthe.g., GorlinGoltz syndrome, Wilson syndrome | Dense hypovascular, hypocellular collagenous tissue.Inflammation absent to mild |
| 9 | Wegener’s Granulomatosis [10] | Generalised | Strawberry gingivitis- reddish purple exophyticpatechial haemmorageSystemic involvement seen | Granulomatous tissue |
| 10 | Metastatic tumours [7] | Attached gingiva | Resemble hyperplastic lesions or PGIn 30% cases it is first indication of metastasis | Microscopic picture resemble the tissue of origin of malignancy |
| 11 | Leukaemia [7] | Generalised | Mimics inflammatory enlargement, other findings include oral ulceration, petechiae, spontaneous bleeding, superimposed herpatic and candidal infections | Massive infiltration of leukaemic cells in gingival tissue.Confirmatory diagnosis to be made by total blood cell count |
| 12 | HIV associated overgrowths [7] | Localised | Mimics other gingival enlargements like PG.Bacillary angiomatosis more common | Warthin Ostarry stain depicts dense extracellular deposits of pale hematoxyphilic granular material that represents masses of bacilli. |
| 13 | Kaposis sarcoma [7] | Localised | Mimics other gingival overgrowths like PG.Associated with HIV AIDS | Vascular clefts, dysplastic spindle cells, intracellular hyaline globules and extravasated erythrocytes. |
| 14 | Tuberculous enlargement [10] | Localised | Very rare, painless gingival overgrowth with lymphadenopathy and systemic involvement | Complete blood count, evidence of microorganisms on histopathology. |
| 15 | Plasma cell gingivitis [10] | Generalised | Allergy associated, diffuse enlargement which bleeds on provocation, burning sensation on eating spicy foods. | Hyperplastic tissue with large influx of plasma cells. |
FFH-Focal Fibrous Hyperplasia; PG-Pyogenic Granuloma; POF-Peripheral Ossifying Fibroma; PGCG-Peripheral Giant Cell Granuloma; hs-CRP-High-sensitivity C-Reactive Protein
Conclusion
Focal reactive overgrowths have a distinct histopathology that show similar clinical and biological behaviour and excision is the treatment of choice for them. Removing the aetiological factors like plaque, calculus will aid in avoiding recurrence of these lesions.
FFH-Focal Fibrous Hyperplasia; PG-Pyogenic Granuloma; POF-Peripheral Ossifying Fibroma; PGCG-Peripheral Giant Cell Granuloma; LCH: Langerhans Cell Histiocytosis
FFH-Focal Fibrous Hyperplasia; PG-Pyogenic Granuloma; POF-Peripheral Ossifying Fibroma; PGCG-Peripheral Giant Cell Granuloma; hs-CRP-High-sensitivity C-Reactive Protein
[1]. Reddy V, Saxena S, Saxena S, Reddy M, Reactive hyperplastic lesions of the oral cavity: A ten year observational study on north Indian populationJ Clin Exp Dent 2012 4(3):e136-40. [Google Scholar]
[2]. Parwani S, Parwani RN, Diagnosis and management of focal reactive overgrowths of gingiva--a case seriesJ Mich Dent Assoc 2014 96(7):36-47. [Google Scholar]
[3]. Kfir Y, Buchner A, Hansen LS, Reactive lesions of the gingiva. A clinico-pathological study of 741 casesJ Periodontol 1980 51(11):655-61. [Google Scholar]
[4]. Daley TD, Wysocki GP, Wysocki PD, Wysocki DM, The major epulides: clinicopathological correlationsJ Can Dent Assoc 1990 56(7):627-30. [Google Scholar]
[5]. Puranik RS, Puranik SR, Localized gingival growths: do they belong to the common spectrum called frog?Aust Dent J 2011 56(1):109 [Google Scholar]
[6]. Savage NW, Daly CG, Gingival enlargements and localized gingival overgrowthsAust Dent J 2010 55(Suppl1):55-60. [Google Scholar]
[7]. Jafarzadeh H, Sanatkhani M, Mohtasham N, Oral pyogenic granuloma: A reviewJ Oral Sci 2006 48(4):167-75. [Google Scholar]
[8]. Effiom OA, Adeyemo WL, Soyele OO, Focal reactive lesions of the gingiva: An analysis of 314 cases at a tertiary health institution in NigeriaNiger Med J 2011 52(1):35-40. [Google Scholar]
[9]. Vidyanath S, Shameena PM, Johns DA, Shivashankar VY, Sudha S, Varma S, Reactive hyperplasic lesions of the oral cavity: A survey of 295 cases at a tertiary Health Institution in KeralaJ Oral Maxillofac Pathol 2015 19(3):330-34. [Google Scholar]
[10]. Agrawal AA, Gingival enlargements: Differential diagnosis and review of literatureWorld J Clin Cases 2015 3(9):779-88. [Google Scholar]
[11]. Buchner A, Shnaiderman-Shapiro A, Vered M, Relative frequency of localized reactive hyperplastic lesions of the gingiva: a retrospective study of 1675 cases from IsraelJ Oral Pathol Med 2010 39(8):631-38. [Google Scholar]
[12]. De Santana Santos T, Martins-Filho PRS, Piva MR, de Souza Andrade ES, Focal fibrous hyperplasia: A review of 193 casesJ Oral Maxillofac Pathol 2014 18(Suppl 1):S86-S89. [Google Scholar]
[13]. Datar UV, Mohan BC, Hallikerimath S, Angadi P, Kale A, Mane D, Clinicopathologic study of a series of giant cell fibroma using picrosirius red polarizing microscopy techniqueArch Iran Med 2014 17(11):746-49. [Google Scholar]
[14]. Mergoni G, Meleti M, Magnolo S, Giovannacci I, Corcione L, Vescovi P, Peripheral ossifying fibroma: A clinicopathologic study of 27 cases and review of the literature with emphasis on histomorphologic featuresJ Indian Soc Periodontol 2015 19(1):83-87. [Google Scholar]
[15]. Tandon PN, Gupta SK, Gupta DS, Jurel SK, Saraswat A, Peripheral giant cell granulomaContemp Clin Dent 2012 3(5):S118-21. [Google Scholar]