A Rare Case of Ulceronodular Cutaneous Metastases from Nasopharyngeal Carcinoma
Richa Chauhan1, Naveen Kuna2, Vinita Trivedi3, Rita Rani4, Usha Singh5, Vasudha Singh6
1 Senior Consultant, Department of Radiation Oncology, Mahavir Cancer Sansthan, Patna, Bihar, India.
2 Resident, Department of Radiation Oncology, Mahavir Cancer Sansthan, Patna, Bihar, India.
3 Head of Department, Department of Radiation Oncology, Mahavir Cancer Sansthan, Patna, Bihar, India.
4 Senior Consultant, Department of Radiation Oncology, Mahavir Cancer Sansthan, Patna, Bihar, India.
5 Consultant, Department of Radiation Oncology, Mahavir Cancer Sansthan, Patna, Bihar, India.
6 Senior Resident, Department of Radiation Oncology, Mahavir Cancer Sansthan, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Naveen Kuna, Resident, Department of Radiation Oncology, Mahavir Cancer Sansthan, Phulwarisharif, Patna-801505, Bihar, India.
E-mail: kuuna.naveen@gmail.com
Nasopharyngeal cancer is a rare cancer in most part of the world, but commonly seen in natives of southern China, Southeast Asia, the Arctic, and the Middle East/North Africa. It is sensitive to radiotherapy and chemotherapy and is usually treated by chemoradiation. It is highly predisposed to nodal and distant metastasis. Still, cutaneous metastasis is rarely seen. Here in this report, we present the case of nasopharyngeal carcinoma with an ulceronodular type of cutaneous metastasis, presenting six years after the initial diagnosis without any visceral metastases. Another feature noted in our patient was the sensitivity to low dose radiotherapy both for bulky primary disease which was progressive on 5Fluorouracil (5FU) and cisplatin based chemotherapy, and subsequent metastases. Theoretically, skin metastases can occur through spread via dermal lymphatics or when the pulmonary filtration is bypassed via the vertebral venous system and Batson’s plexus allowing skin implantation. Further, resistance to chemotherapy and high sensitivity to radiation suggests heterogeneity among nasopharyngeal cancers with intrinsic molecular subtype. The good response of metastatic disease to short course radiation suggests that patients with cutaneous and nodal metastases without visceral metastases could be aggressively treated and the patient can have a good quality of life.
Chemoresistance, Nasopharyngeal cancer, Radiosensitivity
Case Report
A 28-year-old male patient presented to our hospital in August 2011 with complains of multiple, painless nodal swelling on left side of neck for the past 1.5 months. He underwent a biopsy and the histopathological report was suggestive of Non- Hodgkin’s Lymphoma.
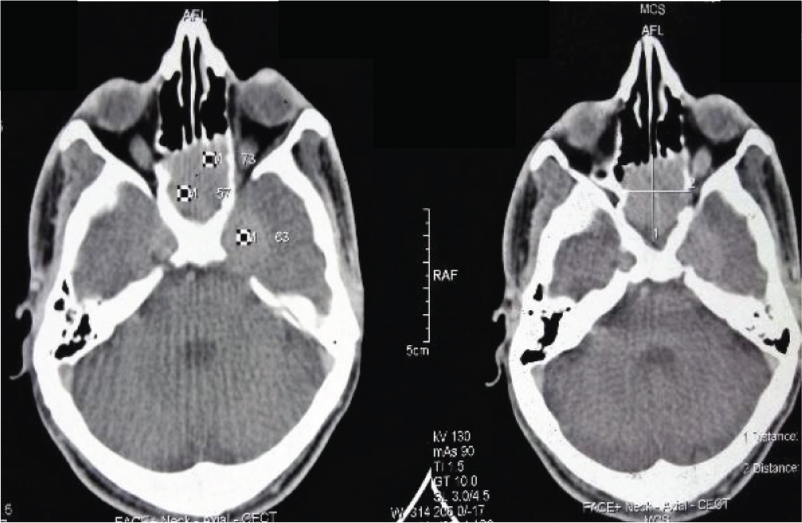
Initially, the patient received two cycles of chemotherapy with Cyclophosphamide, Adriamycin, Vincristine and Prednisolone (CHOP regimen) with progressive disease. Subsequently, a repeat biopsy was done which suggested metastatic undifferentiated carcinoma of nasopharynx. The IHC was negative for CD30 and CD68 markers and positive for cytokeratin and Epithelial Membrane Antigen (EMA). A Contrast Enhanced Computed Tomography (CECT) scan of the face and neck region showed growth in the nasopharynx infiltrating sphenoid sinuses and bulky 10 x 8 cm left cervical neck nodes [Table/Fig-1,2]. In view of the locally advanced disease, the patient was planned for neoadjuvant chemotherapy with 5FU and cisplatin followed by radical chemoradiation. However, as the disease progressed on chemotherapy showing an increase in the size of neck nodes to 14 cm x 10 cm, the patient was referred for palliative radiotherapy.
CECT film showing nasopharyngeal growth extending into surrounding structure.
The patient received palliative radiotherapy to the primary and the neck nodes to a dose of 40 Gy for 16 fraction i.e., 2.5 Gy per fraction, five days a week over three weeks by bilateral conventional portals on a Cobalt-60 teletherapy machine. The disease responded well and there was a complete clinical response seen at first follow up after six weeks. The patient became asymptomatic and defaulted.
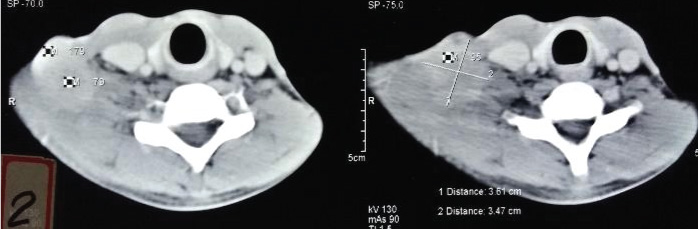
The patient came back after three years in December, 2015 with an ulcerated, hard fixed 8 cm x 6 cm nodal mass in the right supraclavicular region [Table/Fig-3]. A biopsy was done which showed metastatic nasopharyngeal carcinoma. The metastatic work up done was normal. As the nodal mass was inoperable, the patient was planned for reirradiation. The patient was treated to a dose of 40 Gy for 16 fraction i.e., 2.5 Gy per fraction, five days a week over three weeks by 3D Conformal Radiation Therapy (CRT) technique. There was a complete clinical response and the patient again defaulted.
Suggesting nodal recurrence.
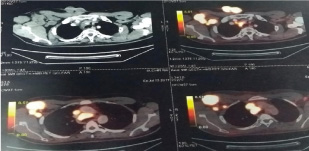
Then, the patient came back after 1.5 years in June, 2017 with a bleeding, ulcerated nodular growth over anterior chest wall and swelling over right anterior axillary fold [Table/Fig-4]. A biopsy was done which showed metastatic nasopharyngeal carcinoma. Finally, a Positron Emission Tomography-Computed Tomography (PET-CT) was done which showed a heterogeneously enhancing FDG avid exophytic cutaneous and sub cutaneous soft tissue lesions in right anterior chest wall and multiple FDG avid heterogeneously enhancing enlarged right axillary and subpectoral nodes. Few small mild FDG avid lymph nodes in left axillary and mediastinal nodes were also seen [Table/Fig-5].
Ulcerated cutaneous metastasis over chest wall.

PET-CT Scan film showing cutaneous, right axillary and mediastinal metastses.
Patient was again treated with a short course of palliative radiotherapy to control bleeding of the skin lesion with a dose of Total 30 Gy in 10 fractions, 3 Gy per fraction. five days a week for three weeks. The patient again showed complete regression of the ulcerated growth and nodal mass two weeks after completion of radiation [Table/Fig-6,7]. The patient was planned for palliative chemotherapy in view of multiple mediastinal lymph nodes. On last follow up of the patient, chest wall growth was completely resolved.
Immediate response after completion of radiation.

Complete response two weeks after Radiation.

Discussion
Nasopharyngeal cancer is a rare cancer in most parts of the world, but commonly seen in a few well-defined populations, like the natives of southern China, Southeast Asia, the Arctic, and the Middle East/North Africa. Both environmental and genetic factors contribute to this distinctive racial/ethnic and geographic distribution [1]. Among head and neck cancers, it is the most limitation of the study.
Predisposed to nodal and distant metastases. Spread of cancer to regional cervical lymph nodes can be found in up to 90% of the patients because of a rich lymphatic network [2]. Distant hematogenous metastases is also common especially in patients with lower neck node involvement [3]. The most common site of distant metastases remains bone, followed by lungs and liver. Brain and skin metastases rarely occurs [2]. In fact, the incidence of skin metastases from internal malignancies has been reported to range from 1% to 10% in Asian and Caucasian populations respectively [4,5]. These are most commonly associated with breast or lung primaries [6]. A literature review of cutaneous metastases from squamous cell carcinoma of head and neck region shows a much lower incidence between 0.8% to 1.3% [7]. Skin metastasis can present in various patterns like skin nodules, ulcers, erythematous patches, plaques which may at times may mimic infective skin lesions like erythema annulare, contact dermatitis, tinea infections, erysipelas [8]. Theoretically, skin metastases can occur via dermal lymphatics or when the pulmonary filtration is bypassed via the vertebral venous system and Batson’s plexus allowing skin implantation [9]. Skin metastasis can also occur via the pulmonary circulation itself, with tumour cells that survive the filtration process [10].
Cutaneous metastases from nasopharyngeal cancer has been reported in the form of small metastatic nodules, subcutaneous metastasis and even zosteriform pattern metastasis, but never as a large ulcerated nodule as seen in our patient [11,12].
Another feature noted in our patient was the three years disease free period after a short course radiotherapy for bulky disease which was progressive on 5FU and cisplatin based chemotherapy. The standard treatment of locally advanced nasopharyngeal carcinoma is chemoradiation [13]. Cisplatin is a platinum-based chemo drug used most commonly in the treatment of nasopharyngeal cancer with good response rate. Cisplatin causes cell cycle arrest and induce apoptosis by forming adducts with the DNA of the cancer cells. Cisplatin-based chemotherapy has shown to improve the overall and progression-free survival in such patients [14]. However, at times the tumour may have inherent resistant to cisplatin as seen in our patient [15].
Radiotherapy to a dose of about 70 Gy for 35 fraction is the standard treatment for all nasopharyngeal carcinoma, with a five-year survival rate of. Studies have shown that nasopharyngeal cancer includes a heterogeneous group of tumors that range from radiosensitive to radioresistant subtype. [16] Our patient received a short course of radiotherapy (40 Gy for 16 fraction i.e., 2.5 Gy per fraction) which was biologically equivalent to 50Gy. The complete response for three years seen in our patient also suggests that there are highly radiosensitive sub groups which can be treated with low dose radiotherapy, as also reported by Xu BQ et al., [16]. A recent study by Xu BQ et al., also concluded that in a subset of radiosensitive nasopharyngeal cancer patients, 50Gy radiotherapy conferred a high long-term survival rate and good quality of life [16].
Further, our patient showed ulceronodular cutaneous metastasis about 60 months after treatment of the primary tumor without any visceral metastases. This is again different from the cases reported in the literature, in which skin metastases were observed 5 to 35 months after treatment and were associated with visceral metastases and poor survival [12].
Conclusion
In general, skin metastasis from nasopharyngeal cancer is very rare and usually presents as a terminal stage of malignancy with visceral metastases. However, in the absence of internal visceral organ metastasis, some cancer patients with metastasis of skin only may show a complete response to treatment with a good quality of life. Till date there is no consensus on their management so, their treatment has to be individualized depending up on the response of the initial disease and performance status of the patient.
[1]. Chang ET, Adami HO, The enigmatic epidemiology of nasopharyngeal carcinomaCancer Epidemiology and Biomarkers Prevention 2006 15(10):1765-77. [Google Scholar]
[2]. Halperin EC, Perez CA, Perez Brady WL, Principles and practice of radiation oncology 2013 6th edLippincott Williams and Wilkins:1936 [Google Scholar]
[3]. Sham JS, Choy D, Choi PH, Nasopharyngeal carcinoma: the significance of neck node involvement in relation to the pattern of distant failureThe British journal of radiology 1990 63(746):108-13. [Google Scholar]
[4]. Hu SS, Chen GS, Lu YW, Wu CS, Lan CC, Cutaneous metastases from different internal malignancies: a clinical and prognostic appraisalJournal of the European Academy of Dermatology and Venereology 2008 22(6):735-40. [Google Scholar]
[5]. Lookingbill DP, Spangler N, Helm KF, Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patientsJournal of the American Academy of Dermatology 1993 29(2):228-36. [Google Scholar]
[6]. Wollina U, Graefe T, Konrad H, Schonlebe J, Koch A, Hansel G, Cutaneous metastases of internal cancerActa Dermatovenerologica Alpina Panonica Et Adriatica 2004 13(3):79-85. [Google Scholar]
[7]. Yoskovitch A, Hier MP, Okrainec A, Black MJ, Rochon L, Skin metastases in squamous cell carcinoma of the head and neckOtolaryngology—Head and Neck Surgery 2001 124(3):248-52. [Google Scholar]
[8]. Poovaneswaran S, Paleri V, Charlton F, Dobrowsky W, Kelly C, Cutaneous metastases from head and neck squamous cell carcinomaMed J Malaysia 2012 67(4):431 [Google Scholar]
[9]. Batson OV, The role of the vertebral veins in metastatic processesAnnals of Internal Medicine 1942 16(1):38-45. [Google Scholar]
[10]. Caloglu M, Uygun K, Altaner S, Uzal C, Kocak Z, Piskin S, Nasopharyngeal carcinoma with extensive nodular skin metastases: A case reportTumori 2006 92(2):181-84. [Google Scholar]
[11]. Luk NM, Yu KH, Choi CL, Yeung WK, Skin metastasis from nasopharyngeal carcinoma in four Chinese patientsClinical and Experimental Dermatology 2004 29(1):28-31. [Google Scholar]
[12]. González García A, Fernández EG, Barbolla Díaz I, Ballester A, Pian H, Fraile G, A Rare Case of Zosteriform Cutaneous Metastases from a Nasopharyngeal CarcinomaCase Reports in Dermatological Medicine 2015 2015:415393 [Google Scholar]
[13]. Su SF, Han F, Zhao C, Chen CY, Xiao WW, Li JX, Long-term outcomes of early-stage nasopharyngeal carcinoma patients treated with intensity-modulated radiotherapy aloneInternational Journal of Radiation Oncology* Biology* Physics 2012 82(1):327-33. [Google Scholar]
[14]. Xiao WW, Huang SM, Han F, Wu SX, Lu LX, Lin CG, Local control, survival, and late toxicities of locally advanced nasopharyngeal carcinoma treated by simultaneous modulated accelerated radiotherapy combined with cisplatin concurrent chemotherapyCancer 2011 117(9):1874-83. [Google Scholar]
[15]. Liu RY, Dong Z, Liu J, Yin JY, Zhou L, Wu X, Role of eIF3a in regulating cisplatin sensitivity and in translational control of nucleotide excision repair of nasopharyngeal carcinomaOncogene 2011 30(48):4814-23. [Google Scholar]
[16]. Xu BQ, Tu ZW, Tao YL, Liu ZG, Li XH, Yi W, Forty-six cases of nasopharyngeal carcinoma treated with 50 Gy radiotherapy plus hematoporphyrin derivative: 20 years of follow-up and outcomes from the Sun Yat-sen University Cancer CenterChinese journal of cancer 2016 35(1):37 [Google Scholar]