Introduction
Researchers expect climate change to alter human health in important ways, with significant regional variations. This change has the potential to affect human health in many ways.
Aim
To systematically review relevant literature in relation to the effect of climatic variables on cardiopulmonary function as an emerging health challenge.
Materials and Methods
The present systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The key words “environment”, “weather”, “chronic obstructive pulmonary disease”, climate change” were used in combination with the Boolean operators “OR” and “AND”. We did electronic searches on PubMed, Science Direct, Springer Link and Google Scholar. The search was conducted with publication year limitation between January 2006 to June 2016.
Results
A total of 1021 articles were extracted and 13 articles were selected for final review, based on the objective of the study. Results suggested that climate changes are not only an environmental and economic problem but also play a role in population health. Climate change parameters like temperature, humidity and air pollution can affect cardiopulmonary health.
Conclusion
The study shows the effect of climate change on cardiopulmonary health, and identifies it as an emerging phenomenon that needs effective planning for emerging and re-emerging concerns.
Introduction
The United Nations Framework Convention on Climate Change (UNFCCC), states “climate change” as “a change of climate which is attributed directly or indirectly to human” [1]. Climate change refers to long term shifts in weather conditions and pattern changes in global weather [2].
This complicated phenomenon includes changes in the average or distribution of weather determinants (i.e., extreme weather events). Mountain glaciers are contracting, ocean water is becoming more acidic, and extreme weather events (unusual precipitations and hurricanes) occur more often [3]. Climate change can affect physical or mental health. Concentration of ambient air pollution have been associated with a range of adverse health effects [4,5].
In recent years, great efforts have been made regarding the diagnosis and treatment of Non-Communicable Diseases (NCDs). For prevention and control of NCDs the United Nations has identified four major chronic diseases: cardiovascular diseases including stroke; cancer; chronic respiratory disease; and diabetes mellitus as the major contributors of worldwide disease burden [6,7]. Extremely high air temperature might trigger the onset of cardiovascular events in the vulnerable people. The cardiopulmonary system and the gastrointestinal tract are vulnerable to the adverse effects of climate change too [7,8].
Another potential effect of climate change is extreme heat waves which are a severe threat to human well-being and health [9]. Then heat-health plans need to accommodate the effects of temperature as well as humidity at different times of the day [10]. According to studies the higher relative humidity was also associated with mortality due to acute myocardial infarction. Seasonal change in death was also found, with the average daily deaths caused by acute myocardial infarction in winter being almost 32% higher than summer [8]. Also, meteorological variations were most marked in the immediate 72 hours prior to heart failure hospitalisation [11].
Studies have shown that environmental temperature and humidity may play a role in angina. Then, there is an impact of humidity on health, especially in case of climate-sensitive infectious and respiratory system disease. A seasonal variation in acute myocardial infarction has important clinical implications. There is an association between outdoor heat and respiratory hospitalisation in the elderly people. Also, the relationship between heat and respiratory morbidity was found [12-18].
Controlling release of black carbon, ozone, and methane could prevent millions of deaths. According to World Health Organization (WHO) report, annually 3.7 million premature deaths occur because of exposure to outdoor air pollution and household air pollution from burning solid fuel. Also, these pollutants cause millions of deaths by strokes and ischemic heart diseases [19]. People who live in these polluted areas are susceptible to asthma [20]. Elevated concentrations of greenhouse gases and carbon dioxide in the earth’s atmosphere have already warmed the planet substantially, causing more severe and prolonged heat waves, temperature variability, forest fires, floods, air pollution and droughts, all of which put respiratory health at risk [21-23].
One potential effect of heat waves is that they can duplicate adverse effect of chronic lung disease [24]. The greater risk of mortality due to cold waves was shown for several diseases such as cardiorespiratory diseases, hypertension, stroke, Congestive Heart Failure (CHF), Chronic Obstructive Pulmonary Disease (COPD) and, pneumonia [25]. The greatest increase in number of diseases was found with pneumonia and influenza (16%), bronchitis and emphysema (12%), and COPD (14%) [26,27]. Respiratory viral incidence patterns are often preparing a comprehensive global model of respiratory infections with seasonal details in different geographical zones which might decrease the morbidity and mortality rate in exacerbation of COPD [28]. COPD happens in all four seasons especially in winter [29-31].
Since, cardiopulmonary disease is a multifactorial health concern in which environmental perturbation or climate change is considered as an emerging parameter for the inducement of these problems. It is so important that we can understand the effects of climate change on cardiopulmonary health in order to prevent them. With this background, the improvement in our knowledge is essential in order to develop effective strategies for mitigation and prevention meant to reduce the potential impacts of climate changes in future. A collaborative effort of physicians, nurses, scientists, industry, and government is needed to protect health and increase awareness regarding climate change.
Materials and Methods
Data Sources and Search Strategy
We performed an electronic search on PubMed using the following terms between January 2006 to June 2016: “climate change,” “climate variability,” “meteorological factors,” “weather,” “Chronic Obstructive Pulmonary Disease/COPD,” “human health,” “health effects,” “cardiovascular disease,” “cardiopulmonary disease,” and “respiratory disease”. Using OR and AND, key words were combined and entered in the search box of the databases as follows: (climate change OR climate variability OR meteorological factors OR weather) AND (human health OR health effects OR cardiovascular disease OR cardiopulmonary disease OR respiratory disease OR Chronic Obstructive Pulmonary Disease/COPD).
The references of all retrieved original articles and reviews were assessed for additional relevant items. We also reviewed recent reports on the relationship between climate and human health from non-biomedical journals like journal articles published by World Meteorological Organization (WMO) as well as from regulatory documents produced by environmental and health agencies. The set describes the climate and weather, including climate variables (such as temperature, humidity), or meteorological hazards (such as drought, flood, and heat waves Inputs from subject experts were further obtained to revise the search strategy and to locate additional citations.
A comprehensive literature search was conducted using Web of Science/Knowledge, Google Scholar (http://scholar.google.com), Elsevier Science Direct (http://www.sciencedirect.com/), Springer Online Journals (http://link.springer.com/) and PubMed (http://www.pubmed.com/). The focus was on the peer-reviewed articles in English between January 2006 to June 2016.
Other major and closely relevant synthesis reports were also reviewed, including WHO. Finally, 13 articles were included for this review research. These publications share a focus on the effects of climate change on cardiopulmonary health.
Inclusion Criteria
The following eligibility criteria were used in this study:
- Articles written in English.
- Types of studies: The present review included peer-reviewed original, case study, review and editorial articles. Thus, books and conference abstracts were excluded.
- Research factors: Only studies in which climate change was one of the exposure indicators of interest were considered.
Study Selection and Data Extraction
The quality of articles that met the inclusion criteria, was assessed. Three of the authors independently assessed the potential relevance of all publications, identified the database search, based on the information provided in the titles and abstracts. After screening by titles and abstracts, the full texts of the remaining articles were then obtained and critically reviewed by the authors and extracted data from the final selected references. All data extraction was performed by the author and cross-checked by another researcher. Any error identified was corrected through discussion among all authors.
Results
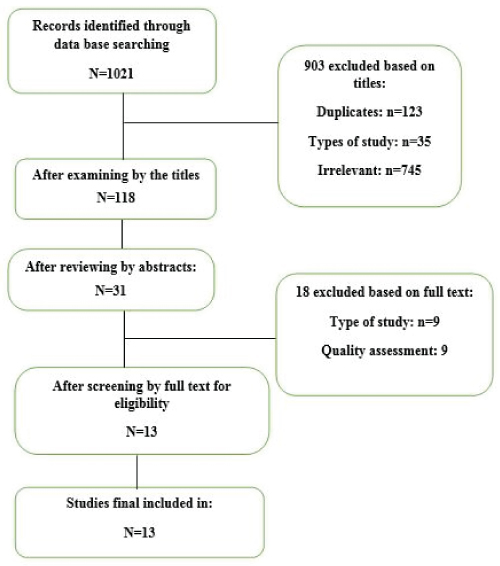
A total of 1021 records were identified from the electronic search of the databases. After exclusion by titles, types of study (the ones that were not clear to classify in terms of year limitation and language), irrelevant (the quality of studies, books and references was too low) and repeated articles, 118 articles were reviewed. At this stage, 903 articles were excluded. After reviewing by abstract, 31 articles were included in the study. After full text review, according to PRISMA checklist, 18 articles were excluded after considering type of articles and quality assessment. Finally, 13 papers were investigated for inclusion in this systematic review [Table/Fig-1]. Then assessment and data synthesis were performed to obtain the key results presented and summarised in [Table/Fig-2].
Flow chart of the screening and selection process of the study articles.
The results of studies conducted in different countries.
| Author and year | Reference No. | Study region and period | Target population | Study design and analysis method | Exposure variable | Health impact |
|---|
| Cheng TO (2009) | [15] | US | - | Editorial | Cold temperatureHumiditySeasonal variationAir pollution | Acute myocardial infarction |
| Cheng X and Su H (2010) | [8] | China | - | Review | TemperatureExtreme heatExtreme cold | Sudden cardiovascular event |
| Bhaskaran K et al., (2012) | [12] | England and Wales June 2003 to August 2009 | 24861 hospital admissions for myocardial infarction occurring in 11 conurbations | Case-crossover study Odds ratio | Higher temperatures | Myocardial infarction |
| Chockalingam A et al., (2012) | [6] | US | - | Editors page | Air pollution | CVD(Cardiovascular disease) non communicable disease |
| Anderson GB et al., (2013) | [16] | USJanuary 1, 1999 to December 31 | 12.5 million Medi-care beneficiaries in 213 United States counties | Observational studyUsing Bayesian hierarchical models | Respiratory diseases associated with outdoor heat | Heat-related emergency hospitalisations respiratory diseases |
| Gao J et al., (2014) | [14] | ChinaUntil March 2013 | - | ReviewSTROBE method | Ambient humidity | Weather-related health outcomes, particularly among children. Infectious diseases, Diarrheal diseases, respiratory system diseases, and paediatric allergic diseases |
| Rice MB et al., (2014) | [18] | US | - | Review | Climate changeRising CO2 levels | Cardiopulmonary health |
| Gerardi DA and Kellerman RA (2014) | [22] | US | - | Review | Nature of climate change and both its immediate and long-term effects on human respiratory health | Climate change leads to an increase in the prevalence of certain respiratory diseases, exacerbations of chronic lung disease, premature mortality, allergic responses, and declines in lung function |
| Das D et al., (2014) | [11] | In 30 countries | 7141 patients at 398 sites in 30 countries | Clinical trial, Acute Study of Clinical, Effectiveness of Nesiritde in Decompensated Heart Failure (ASCEND-HF) trial | Global meteorological conditions temperature and humidity | Meteorological fluctuations were most evident in the immediate 72 hours prior to the heart failure hospitalisation but also seen as far out as 7 days prior |
| Franchini M and Mannucci PM (2015) | [7] | ItalyUntil November 30, 2014 | - | Review | Heat waves, hurricanes, cyclones, drought, warm temperature, cold temperatures, heat stroke, heat exhaustion, cold-related mortality/morbidity, greenhouse gases, global warming | Human health, allergen vector borne infectious disease, cardiopulmonary system, gastrointestinal tract typhus, cholera, malaria, dengue and West, Nile virus infection pneumonia (bronchitis and arthritis), death, morbidity |
| Goldie J et al., (2015) | [10] | Australia | Patients from the 5 hospitals | Cohort study, Univariate and bivariate Poisson generalised linear models | Temperature and humidity heat | At different times of day temperature and humidity act differently on the health of people. Healthcare providers in climatically similar locations may benefit from considering temperature and humidity separately |
| De Blois J et al., (2015) | [17] | US | People with pre-existing, Medical conditions such as CVD and the elderly are particularly vulnerable susceptible individuals with preexisting cardiopulmonary disease | ReviewPRISMA checklist | Climate change, heat exposure and increasing heat | Climate changes have a variety of negative effects on health, including cardiac health |
| Xiaoxu W et al., (2016) | [3] | China1990 to 2015 | Relationships between climate change, human infectious diseases and human society | Review | Vector-borne disease | The health effects of climate change (including changes in climate variables and extreme weather events) on human infectious diseases are imposed through impacts on pathogens, hosts/vectors, and disease transmission |
Discussion
The purpose of this systematic review was to summarise key findings related to the effect of climate change on cardiopulmonary health, and identify the relationship between them. The systematic review of the 10 included publications performed demonstrates that climate change plays a role in the incidence and prevalence of cardiopulmonary diseases [6-8,11,14-18,22]. Considering the expected continuity of climate change, the adverse influence of ambient humidity on vulnerable individuals may become increasingly serious. Environmental changes do have an influence on cardiac health.
As mentioned earlier according to studies, deaths from heart disease increase in winter [8]. This shows the association of temperature with excess winter mortality. The cold stress may be related with the flu season and an increase respiratory tract infection that could also affect the cardiovascular system. In this case influenza vaccination can be helpful and reduce incidence of cardiovascular abnormality and sudden cardiac death. These approaches may be important for developing strategies in preventing cardiovascular events [30]. The effect of extreme climatic change on cardiovascular disease is hard to predict, because the extent to which the temperature-mortality association changes by gender, age and other factors is difficult to address. Climatic changes especially for cold stress could be considered a new potential risk factor of cardiovascular events in human health, and there is need for community-based study of cardiovascular events to deeply explore the risk factors, to schedule preventive strategies.
Prevention to reduce health risks resulting from global influences is a formidable challenge. It requires insights beyond the conventional understanding of causation and prevention [32]. Furthermore, higher temperatures seem to be associated with increased risk of myocardial infarction after exposure. Policies aimed at reducing the health effects of hot weather should include consideration of effects operating at sub-daily time scales. The temperature-myocardial infarction association may be larger on the first day of a hot weather period than other high temperature days.
Extreme change in weather may cause fatal damages in people’s health because people show low adaptability in abnormal weather conditions. In order to prevent these damages, the patients who have chronic diseases can manage a healthy life through primary health care. They should check weather forecasting daily and can receive better health related meteorological information. It is possible to obtain lots of advantages in the prevention and management of patients [33].
Heat and cold waves are risk factors for cardiovascular and respiratory diseases. The Diurnal Temperature Range (DTR) may affect the rate of hospital admissions for cardiovascular- and respiratory-related diseases. [34].
The sustainable development goals are a principle declaration to stop climate change in the world. The agencies and governments should take more equitable global policies to protect people [35].
Finally, the review of literature found effects of climate change on cardiopulmonary health. It shows that climate change is not only an environmental and economic problem but also has an important impact on population health.
Limitation
This review is limited by its emphasis on papers published in English in peer-reviewed journal databases, so we may have missed potentially useful studies.
Conclusion
This study shows the effect of climate change on cardiopulmonary health. Through knowledge of these effects we can develop population-specific strategies to have an impact on these important global health issues. Identifying climate change effects is an emerging phenomenon, needs planning for emerging and reemerging concerns. Also, it can inform the local health officials and policy-makers to make and implement necessary preparations (mitigation and prevention), ultimately contributing to better health outcomes for populations.
[1]. Gender, climate change and health Geneva-Switzerland: Public health & environment department; 2014 [updated 4/30/2017]. Available from: http://www.who.int/globalchange/GenderClimateChangeHealthfinal.pdf?ua=1 [Google Scholar]
[2]. Hales S, Kovats S, Lloyd S, Campbell-Lendrum D, Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s 2014 [updated 4/30/2017]Available from: http://apps.who.int/iris/bitstream/10665/134014/1/9789241507691_eng.pdf [Google Scholar]
[3]. Xiaoxu W, Yongmei L, Zhou S, Chen L, Bing X, Impact of climate change on human infectious diseases: Empirical evidence and human adaptationEnviron Int 2016 86:14-23. [Google Scholar]
[4]. Hoek G, Krishnan RM, Beelen R, Peters A, Ostiro B, Brunekreef B, Long-term air pollution exposure and cardio-respiratory mortality: A reviewEnvir Health 2013 12:43 [Google Scholar]
[5]. Willox AC, Stephenson E, Allen J, Bourque F, Drossos A, Elgaroy S, Examining relationships between climate change and mental health in the Circumpolar NorthReg Environ Chang 2015 15(1):169-82. [Google Scholar]
[6]. Chockalingam A, Tolunay HE, Prabhakaran D, Narula J, Household air pollution: An emerging risk factor for CVDEur J Int Med 2012 7(3):197-99. [Google Scholar]
[7]. Franchini M, Mannucci PM, Impact on human health of climate changesEur J Int Med 2015 26(1):01-05. [Google Scholar]
[8]. Cheng X, Su H, Effects of climatic temperature stress on cardiovascular diseasesEuropean J Int Med 2010 21(3):164-67. [Google Scholar]
[9]. MacMichael AJ, Lindgren E, Climate change: present and future risks to health, and necessary responsesJ Int Med 2011 270(5):401-13. [Google Scholar]
[10]. Goldie J, Sherwood SC, Green D, Alexander L, Temperature and humidity effects on hospital morbidity in Darwin, AustraliaAnnals of Global Health 2015 81(3):333-41. [Google Scholar]
[11]. Das D, Bakal J, Armstrong P, Ezekowitz J, The association between meterological events and acute heart failure: new insights from ascend-HFCanadian J Cardiology 2014 30(10):198-99. [Google Scholar]
[12]. Bhaskaran K, Armstrong B, Hajat S, Haines A, Wilkinson P, Smeeth LH, Heat and risk of myocardial infarction: Hourly level case-crossover analysis of MINAP databaseBMJ 2012 345:e8050 [Google Scholar]
[13]. Abrignani MG, Corrao S, Biondo GB, Lombardo RM, Di Girolamo P, Braschi A, Effects of ambient temperature, humidity, and other meteorological variables on hospital admissions for angina pectorisEur J Prev Cardiol 2012 19(3):342-48. [Google Scholar]
[14]. Gao J, Sun Y, Lu Y, Li L, Impact of ambient humidity on child health: a systematic reviewPloS One 2014 9(12):e112508 [Google Scholar]
[15]. Cheng TO, Seasonal variation in acute myocardial infarctionInt J Cardio 2009 :277-79. [Google Scholar]
[16]. Anderson G, Dominici F, Wang Y, Cormack M, Bell M, Peng R, Heat-related emergency hospitalizations for respiratory diseases in the Medicare populationAm J Respir Crit Care Med 2013 187(10):1098-103. [Google Scholar]
[17]. De Blois J, Kjellstrom T, Agewall S, Ezekowitz JA, Armstrong PW, Atar D, The effects of climate change on cardiac healthCardiology 2015 131(4):209-17. [Google Scholar]
[18]. Rice MB, Thurston GD, Balmes JR, Pinkerton KE, Climate change. A global threat to cardiopulmonary healthAm J Respir Crit Care Med 2014 189(5):512-19. [Google Scholar]
[19]. Gulland A, Reduction in climate pollutants could save five million lives a year, WHO report saysBMJ 2015 351:h5688 [Google Scholar]
[20]. To T, Zhu J, Larsen K, Simatovic J, Feldman L, Ryckman K, Progression from asthma to Chronic Obstructive Pulmonary Disease (COPD): Is air pollution a risk factor?Am J Respir Crit Care Med 2016 194(4):429-38. [Google Scholar]
[21]. Bernstein AS, Rice MB, Lungs in a warming world climate change and respiratory healthChest2013(5):1455-59. [Google Scholar]
[22]. Gerardi DA, Kellerman RA, Climate change and respiratory healthJournal of Occupational and Environmental Medicine/American College of Occup Environ Med 2014 56(Suppl 10):S49-54. [Google Scholar]
[23]. Forino G, Meding Jv, Brewer G, Gajendran T, Disaster risk reduction and climate change adaptation policy in AustraliaProcedia Economics and Finance 2014 18:473-82. [Google Scholar]
[24]. Witt C, Schubert AJ, Jehn M, Holzgrev A, Liebers U, Endlicher W, The effects of climate change on patients with chronic lung diseaseDeutsches Arzteblatt Int 2015 112(51-52):878-83. [Google Scholar]
[25]. Qiu H, Tian L, Ho KF, Yu IT, Thach TQ, Wong CM, Who is more vulnerable to death from extremely cold temperatures? A case-only approach in Hong Kong with a temperate climateInt J Bio 2016 60(5):711-17. [Google Scholar]
[26]. Fuhrmann CM, Sugg MM, Konrad CE, Waller A, Impact of extreme heat events on emergency department visits in north Carolina (2007-2011)J Community Health 2016 41(1):146-56. [Google Scholar]
[27]. Almagro P, Hernandez C, Martinez-Cambor P, Tresserras R, Escarrabill J, Seasonality, ambient temperatures and hospitalizations for acute exacerbation of COPD: a population-based study in a metropolitan areaInt J COPD 2015 10:899-908. [Google Scholar]
[28]. Hosseini SS, Ghasemian E, Jamaati H, Tabaraie B, Amini Z, Cox K, Association between respiratory viruses and exacerbation of COPD: A case-control studyInfect Dis 2015 47(8):523-29. [Google Scholar]
[29]. Djamin RS, Uzun S, Snelders E, Kluytmans JJ, Hoogsteden HC, Aerts JG, Occurrence of virus-induced COPD exacerbations during four seasonsInfect Dis 2015 47(2):96-100. [Google Scholar]
[30]. Alahmari AD, Mackay AJ, Patel AR, Kowlessar BS, Singh R, Brill SE, Influence of weather and atmospheric pollution on physical activity in patients with COPDRespir Res 2015 16:71 [Google Scholar]
[31]. Hansel NN, Cormack MC, Kim V, The effects of air pollution and temperature on COPDCOPD 2016 13(3):372-79. [Google Scholar]
[32]. MacMichael M, Globalization, climate change, and human healthN Engl J Med 2013 368(14):1335-43. [Google Scholar]
[33]. Oh J, Kim B, Prediction model for demands of the health meteorological information using a decision tree methodAsian Nurs Res 2010 4(3):151-62. [Google Scholar]
[34]. Lim YH, Hong YC, Kim H, Effects of diurnal temperature range on cardiovascular and respiratory hospital admissions in KoreaSci Total Environ 2012 417-418:55-60. [Google Scholar]
[35]. Adel D, Björn H, Debarati GS, What is the association between absolute child poverty, poor governance, and natural disasters? A global comparison of some of the realities of climate changePloS One 2016 11(4):e0153296 [Google Scholar]