Inflammatory Myofibroblastic Tumour –An Unusual Tumour with Intermediate Malignant Potential- Report of Three Cases
Indusarath1, Sangeetha K Nayanar2, Nizamudheen M Pareekutty3, B Satheesan4, Satheesh Babu5
1 Senior Resident, Department of Onco-Pathology, Malabar Cancer Centre, Thalassery, Kerala, India.
2 Professor, Department of Onco-Pathology, Malabar Cancer Centre, Thalassery, Kerala, India.
3 Associate Professor, Department of Surgical Oncology, Malabar Cancer Centre, Thalassery, Kerala, India.
4 Professor, Department of Surgical Oncology, Malabar Cancer Centre, Thalassery, Kerala, India.
5 Assistant Professor, Department of Imageology, Malabar Cancer Centre, Thalassery, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Indusarath, Senior Resident, Department of Onco-Pathology, Malabar Cancer Centre, Sreyas, Thuvakkunnu, Thalassery-670693, Kerala, India.
E-mail: indusarath@gmail.com
Inflammatory Myofibroblastic Tumour (IMT) is a rare mesenchymal neoplasm of borderline malignancy. It is characterised by proliferation of myofibroblasts and fibroblasts with variable amount of inflammatory infiltrate. About 50-60% of the cases show Anaplastic Lymphoma Kinase (ALK) rearrangements. The recurrence rate and metastasis depends on the anatomic site, resectability, size and presence of ALK rearrangements. In this case series, we are presenting three cases diagnosed as IMT. All the patients were elderly. Sites included abdomen, subcutaneous tissue over scapula and orbit. Scapular lesion presented as recurrence in six months after first excision. All three cases were ALK negative. IMTs that occur in elderly persons can mimic malignancy. Surgical excision is the treatment of choice. Diagnosis depends on histopathological features and immunohistochemical examination. Correct histological diagnosis is crucial for further management. Chance of recurrence and metastasis is more in abdominopelvic location, large size and ALK negativity. This case series aims to create awareness of the non-specific presentation of this tumour and need of follow up as this tumour may recur in a very short interval.
Mesentery, Orbit, Pseudotumour, Scapula
Case Series
This case series aims to create awareness of the non-specific presentation of IMT and the need of follow up as this tumour may recur in a very short interval.
Case I
A 67-year-old female patient with good general condition presented with two months history of abdominal fullness and early satiety. On examination, a mobile non-tender lump was palpable in the left lumbar region. Ultrasonographic examination showed a well-defined lobulated solid hypoechoic mass measuring 11.2x10.1x7.6 cm in left hypochondrium with internal vascularity. In Computed Tomography (CT), the lesion was seen as a heterodense mass with hypodense areas and contrast enhancement [Table/Fig-1a] with a possible diagnosis of malignant gastrointestinal stromal tumour. It was proceeded with laparotomic excision.
a) well-defined homogenously enhancing lesion (marked using arrow) in left side of abdomen encasing inferior mesenteric artery; b) Well circumscribed grey-white lobulated mass with myxoid areas in mesentery adherent to colon.
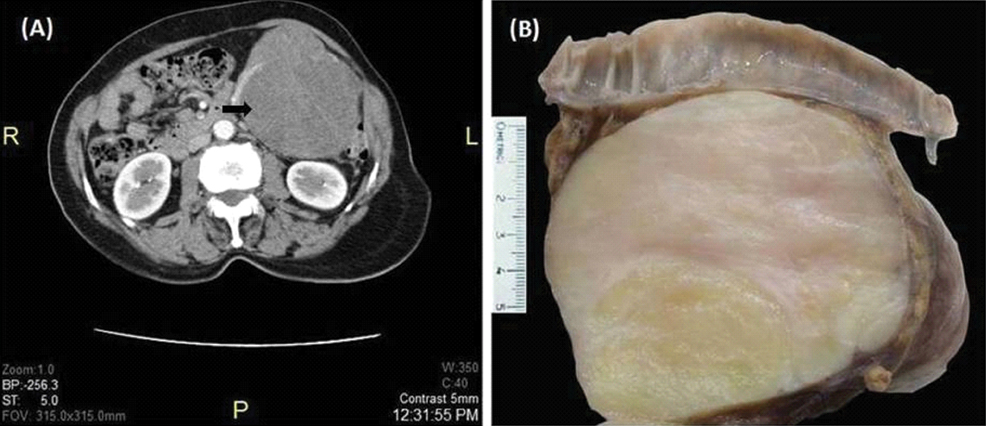
Peroperatively, tumour was seen arising from the mesentery near splenic flexure, adherent to the bowel wall. Tumour was resected along with portion of transverse colon and descending colon including splenic flexure and submitted to the Pathology department in 10% buffered formalin. On gross examination, a well-circumscribed nodular mass measuring 12x9.5x9 cm was seen adherent to portion of large intestine by a thin fascia. Cut section was multi-lobulated, grey white and myxoid in appearance [Table/Fig-1b]. There was no necrosis or haemorrhage. Attached intestine showed no significant pathology.
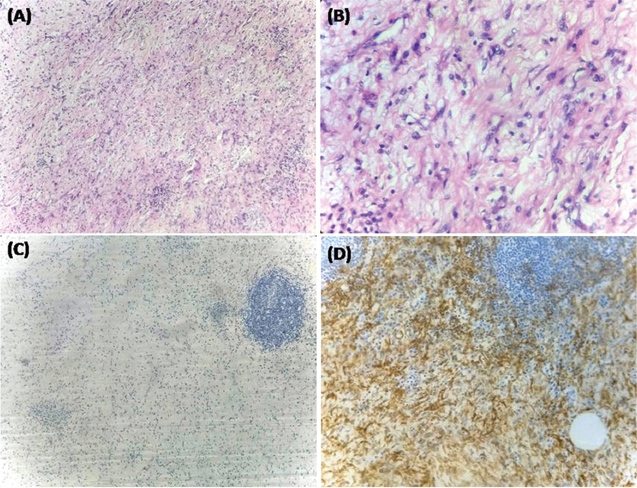
Histological examination of sections stained with Haematoxylin and Eosin (H&E) showed a well-circumscribed neoplasm composed of haphazardly arranged plump spindle to stellate cells with moderate amphophilic cytoplasm, oval vesicular nucleus with no atypia [Table/Fig-2a,b]. Mitosis was scant. There was moderate inflammatory infiltrate of plasma cells and lymphocytes with lymphoid follicle formation. Plenty of small thin walled blood vessels were present with a background of myxoid stroma. There was no necrosis. Possible diagnoses were IMT, Gastrointestinal Stromal Tumour (GIST), Solitary Fibrous Tumour (SFT) and Peripheral Nerve Sheath Tumour (PNST). On immunohistochemical examination, the spindle cells were positive for Smooth Muscle Antibody (SMA) [Table/Fig-2c]; negative for CD117, DOG-1, S100 which ruled out the possibility of GIST and PNST. CD34 was negative on spindle cells which ruled out the possibility of SFT. ALK was negative [Table/Fig-2d]. Proliferation index was very low (Ki-67 less than 1%). Correlating the histological picture and immunohistochemical findings, diagnosis of IMT was given. After four months of follow up, there was no evidence of tumour recurrence.
a) section showing fascicles and haphazardly arranged spindle cells with moderate inflammatory infiltrate in a myxoid background (H&E, 4X); b) cells are plump to spindle with moderate amphophilic cytoplasm and no atypia (H&E, 40X); c) tumour cells are ALK negative (4X); d) SMA is positive in tumour cells (10X).
Case II
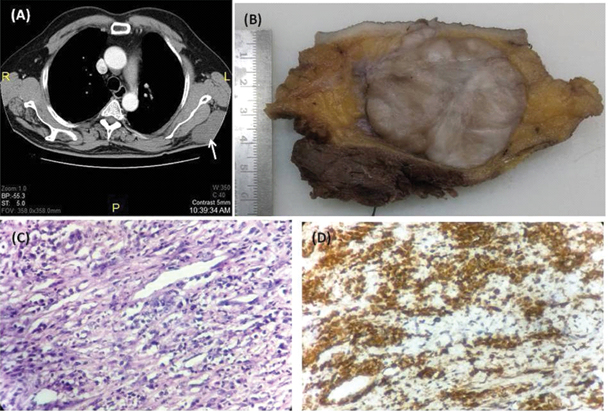
A 59-year-old male presented with swelling in left scapular region for the past four months, which was gradually increasing in size. He had a history of excision of tumour in the same site 10 months back. Physical examination showed an ill-defined firm mass of around 8 cm beneath the previous surgical scar. A CT imaging showed minimally enhancing lobulated mass in subcutaneous plane near left scapula without bone or muscle involvement [Table/Fig-3a]. Wide excision was done and specimen was submitted to the Pathology department. Macroscopically, a firm lesion of size 6.5x5x5 cm was seen located in the subcutaneous fat. Cut section was grey white, firm with vague lobulations [Table/Fig-3b]. Microscopic examination showed short compact bundles of plump spindle cells showing minimal atypia with areas of sclerosis. There was moderate infiltrate of plasma cells and lymphocytes [Table/Fig-3c]. Mitosis was scant and there was no necrosis. The tumour cells were positive for SMA [Table/Fig-3d]. ALK was negative. Histopathology slides of previous excision were reviewed in our department. Correlating with it, a diagnosis of recurrent IMT was made. Patient is on regular follow up. Adjuvant radiotherapy was not considered as in the second surgery a complete tumour resection was done. Three months of follow up period was uneventful.
a) minimally enhancing subcutaneous lobulated mass (marked using arrow) adjacent to left scapula with no evidence of involvement of scapula or chest wall muscles; b) well-circumscribed grey white firm lobulated mass seen located in the subcutaneous fat; c) Spindle cells having amphophilic cytoplasm with plenty of plasma cells and thin walled blood vessels (H&E, 40X); d) The tumour cells were positive for SMA (40X).
Case III
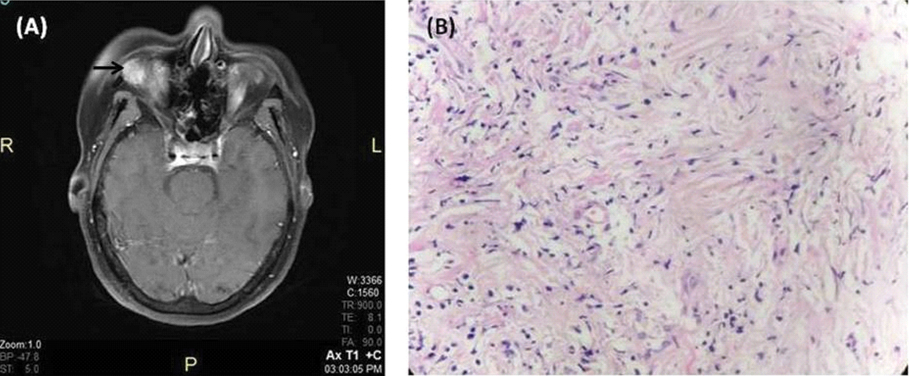
A 66-year-old female patient with no comorbidities presented with a swelling around right eye, which was noticed two year back. Swelling was gradually increasing in size, which narrowed her vision. She also complained of double vision for past two months. Clinical examination showed fullness of right periorbital tissue. Magnetic Resonance Imaging (MRI) image showed homogenously enhancing intraorbital lesion [Table/Fig-4a]. She underwent wide excision of the same. Specimen was received in Pathology department as multiple pieces aggregate measuring 2 cm. Histological examination, showed plump spindle cells arranged as short bundles and in vague storiform pattern with extensive areas of sclerosis [Table/Fig-4b]. There was focal mild infiltrate of plasma cells and eosinophils. There was no organism or granuloma. SMA was positive in the spindle cells and ALK was negative. A final diagnosis of IMT was made. Patient was followed up for five months. Her vision improved after surgery and there was no evidence of tumour recurrence.
a) homogenously enhancing right intraorbital lesion (marked using arrow) seen in the post contrast T1 weighted sequence; b) spindle cells with storiform pattern with sclerosis and sparse inflammatory cells (H&E,10X).
Discussion
Inflammatory myofibroblastic tumour is an uncommon mesenchymal tumour usually affecting children and young adults but can affect any age group [1]. It encompasses a spectrum of lesions having myofibroblastic and fibroblastic proliferation with variable amount of inflammatory cells mainly plasma cells, lymphocytes, with or without histiocytes and eosinophils [2]. It was first detected in lung and was reported in 1939 by Bunn [3]. Due to its uncertain aetiology and neoplastic potential, it had various names, including inflammatory pseudotumour, plasma cell granuloma, omental mesenteric myxoid hamartoma and inflammatory fibrosarcoma [4]. Although, 73% of cases occur in mesentery, omentum, retroperitonium, pelvis and abdominal soft tissue [5], it can occur at any site including liver, head and neck.
Clinical manifestations depend on the site of involvement. About one-third of the patients present with clinical syndrome of fever, malaise, weight loss, microcytic hypochromic anaemia, elevated erythrocyte sedimentation ratio, polyclonal hyperglobulinemia and elevated C-reactive proteins, possibly cytokine mediated [5]. These features usually disappear with excision of the tumour but may reappear on recurrence. Imaging characteristics are variable and non-specific, with most appearing as a lobulated heterogeneous solid mass. Macroscopically, IMT is a circumscribed nodular or multinodular mass with whorled, fleshy or myxoid cut surface. The size can be upto 20 cm [5].
On histopathologic examination, it can show three basic patterns. First pattern, shows loosely arranged spindle or plump myofibroblasts with plasma cells, lymphocytes, eosinophils and plenty of thin walled blood vessels in a myxoid background simulating a reactive process as in our first case. Second pattern, consists of compact fascicular arrangement of spindle cells with distinctive inflammatory infiltrate and variable amount of collagenised or myxoid areas as in the second case. Third pattern, is characterised by scar like proliferation of collagen with less cellularity and relatively sparse infiltrate of plasma cells and eosinophils as in our third case [5]. Immunohistochemically, IMT shows variable positivity for SMA, Muscle Specific Actin (MSA) and desmin.
Gene fusions involving ALK at chromosome 2p23 have been described in IMTs [6]. The mutation results in ALK protein overexpression in the myofibroblastic component which can be detected by immunohistochemistry. But ALK positivity is detectable only in 50-60% cases [5]. The positivity correlates with the presence of ALK rearrangement. It can be either granular cytoplasmic or nuclear membrane positivity depending on CLTC or RAN Binding Protein 2 (RANBP2) fusion partner respectively. But the ALK rearrangements are uncommon in IMT detected in adults of more than 40 year [5]. Around 25% of extra pulmonary IMT shows recurrence, depending on site and resectibility. Chance of recurrence is higher in abdominopelvic IMTs and also in tumours with size more than 8 cm [5]. Metastasis can occur up to 2% of cases, especially in ALK negative cases and size more than 11 cm [5,6]. ALK positive cases show a favourable outcome in terms of recurrence or metastasis on follow up [5,6]. Since the clinical behaviour of IMTs is similar to that of tumours of uncertain malignant potential, now they are considered as tumours of borderline malignancy [5,7]. In our case series, all the three cases show distinct mode of presentation, site, histopathological findings and behaviour. All were ALK negative tumours, which are found to be more aggressive. The recurrence of the tumour in six months in the second case highlights the significance of strict follow up.
Conclusion
Inflammatory myofibroblastic tumour is a rare solid tumour that can at times present in an elderly person mimicking malignancy. Diagnosis should be based on histological findings, as ALK rearrangements are uncommon in that age group. Clinical and laboratory follow up is essential because of an increased risk for local recurrence and metastasis.
[1]. Cook JR, Dehner LP, Collins MH, Ma Z, Morris SW, Coffin CM, Anaplastic lymphoma kinase (ALK) expression in the inflammatory myofibroblastic tumor: a comparative immunohistochemical studyAm J Surg Pathol 2001 25(11):1364-71. [Google Scholar]
[2]. Palaskar S, Koshti S, Maralingannavar M, Bartake A, Inflammatory myofibroblastic tumorContemporary Clinical Dentistry 2011 2(4):74-77. [Google Scholar]
[3]. Dalton BG, Thomas PG, Sharp NE, Manalang MA, Fisher JE, Moir CR, Inflammatory myofibroblastic tumors in childrenJ Pediatr Surg 2016 51(4):541-44. [Google Scholar]
[4]. Dhouib A, Barrazzone C, Reverdin A, Anooshiravani M, Hanquinet S, Inflammatory myofibroblastic tumor of the lung: a rare cause of atelectasis in childrenPediatr Radiol 2013 43(3):381-84. [Google Scholar]
[5]. Fletcher C DM, Bridge JA, Hogendoorn P, Mertens F, WHO Classification of Tumors of Soft Tissue and Bone (4th Edition) 2013 IARCLyon [Google Scholar]
[6]. Coffin CM, Hornick JL, Fletcher CD, Inflammatory myofibroblastic tumor: Comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive casesAm J Surg Pathol 2007 31(4):509-20. [Google Scholar]
[7]. Koyuncuer A, Inflammatory myofibroblastic tumor of the small-bowel mesentery: a case report of nonspecific clinical presentation and a review of the literatureInt J Surg Case Rep 2014 5(12):1214-17. [Google Scholar]