Effects of 60° Semi-recumbent Position on Preventing Ventilator-associated Pneumonia: A Single-blind Prospective Randomised Clinical Trial
Hadi Hassankhani1, Sharzad Akbarzadeh2, Sima Lakdizaji3, Atabak Najafi4, Ebrahim Aliafsari Mamaghani5
1 Associate Professor, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, East Azarbaijan, Iran.
2 Student, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Tabriz University of Medical Science, Tabriz, East Azarbaijan, Iran.
3 Lecturer, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, East Azarbaijan, Iran.
4 Associate Professor, Department of Anaesthesia, Tehran University of Medical Sciences, Tehran, Iran.
5 PhD Student, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, East Azarbaijan, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hadi Hassankhani, Associate Professor, Department of Medical Surgical Nursing, School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, East Azarbaijan, Iran.
E-mail: hassankhanih@tbzmed.ac.ir
Introduction
Head-of-Bed Elevation (HOBE) is now considered as a main modifiable factor for decreasing Ventilator-Associated Pneumonia (VAP) especially in the area of intensive care nursing. Despite numerous studies on the beneficial effects of different HOBE, there is little scientific evidence examining the effect of a 60° HOBE position.
Aim
The present study aimed to examine the effect of 60° HOBE on preventing VAP and respiratory parameters in mechanically ventilated patients.
Materials and Methods
In a single-blind prospective randomised clinical trial, 25 patients were recruited in the multidisciplinary surgical intensive care unit over a period of a year (June 2011 to April 2012), and randomly assigned to the intervention group maintaining position of 60° (n=14) and the control group in the routine position of 45° (n=11). VAP and respiratory parameters (tidal volume, pulmonary compliance, pulmonary resistance, and respiratory rate) were investigated from first to the seventh day of intubation.
Results
HOBE at 60° resulted in significantly lower pulmonary infiltration on chest X-ray (p=0.009), lower axillary temperature (p=0.001), as well as higher tidal volume (p<0.001) and higher pulmonary compliance (p=0.038) compared with the control group. The overall prevalence of VAP was 20% in the intervention group and 73% in the control group (p=0.016). In this regard, HOBE from 45° to 60° reduced the risk of VAP more than three times.
Conclusion
HOBE at 60° results in a significant decrease in the occurrence of VAP and also improvement in some mechanical respiratory parameters including tidal volume and pulmonary compliance.
Head of bed elevation, Mechanical ventilation, Ventilator acquired pneumonia
Introduction
Many countries have paid more attention to nosocomial infection in recent years and most health care organizations have focussed their efforts on their prevention [1]. Pneumonia is the most frequent nosocomial infection in mechanically ventilated patients with high mortality and morbidity in Intensive Care Units (ICUs). The overall prevalence of VAP has been estimated 24% to 76% and the risk for VAP has been recently considered as a quality of care indicator in hospitals [2,3,4].
Aspiration of gastric contents is one of the most common complications in patients receiving mechanical ventilation [5]. Aspiration is the most common cause of bacterial pneumonia infection that results in mortality rate of 40% to 50% due to a wide range of serious complications and progression to Acute Respiratory Distress Syndrome (ARDS) [6,7]. Also, studies have shown that the duration of hospital stay is prolonged and hospital costs are increased in patients with severe pneumonia [8-9]. Epidemiological studies have also shown that the prevalence of VAP can increase from 10-68% in mechanically ventilated patients who are fed in the supine position [11,12]. Supine position is considered as a major risk factor for mortality in mechanically ventilated patients [13,14], while the fowler position (placing the patient in a semi-upright sitting position of 45°) has led to a significant decrease in the prevalence of VAP [15]. Positioning can be used to prevent complications [16]. Recommendations of the Centers for Disease Control and prevention (CDC) are based on HOBE to 45° and even higher than 45° for preventing VAP [17,18]. Additionally, it seems that the only modifiable factor for decreasing VAP especially in the area of nursing is HOBE. Despite numerous studies on beneficial effects of 30° - 45° HOBEs, It remains uncertain which degrees of semi-recumbent position are optimal and there is little scientific evidence investigating the effects of HOBE to 60° [19,20].
As aspiration events (especially micro-aspirations) are a major risk factor for VAP, placing mechanically ventilated patients into the semi-recumbent position with HOBE to 60° is hypothesised to be more effective in prevention of VAP compared to 45° HOBE. The present study aimed to investigate the effect of elevating HOBE to 60° on preventing VAP and respiratory parameters in mechanically ventilated patients.
Materials and Methods
Study population: In a single-blind prospective randomised clinical trial (IRCT201106146801N1), 25 patients were recruited in the multidisciplinary surgical intensive care unit of Sina hospital in Tehran over a period of one year June 2011 to June 2012. Power calculation based on the results of a similar previous study suggests that a study of 14 patients in each group would be required to detect a 26% reduction in VAP with a power of 0.8 [21].
All patients with Endotracheal Tube (ETT) under mechanical ventilation who met inclusion criteria were eligible for enrollment into the study were randomly allocated to intervention (HOBE of 60°) and control (HOBE of 45°) groups by using computer allocate random numbers. The study was conducted under the approval of the Tabriz University of Medical Sciences ethics committee (code NO: 5.4.1160). The written consent of all subjects was obtained from their next of kin before randomization. Inclusion criteria were patients of both sexes who were mechanically ventilated for ≥7 days who were under mechanical ventilation (MODE = SIMV, VT = 6-8 mL/kg, PEEP=2.5-7.5 cmH2O, FiO2=<50%, RR=6-12/minute). Only patients, who maintained haemodynamic stability during the assessment period, were eligible for administration of the protocol. The exclusion criteria included any clinical or laboratory evidence of active infection on admission to ICU, ARDS, head and neck trauma and any contraindication for supine positioning.
The research nurse in the ICU unit conducted data collection in the morning shift and in the evening and night shift consigned to his colleagues however HOBE at 60° was ordered by intensivist. The staff collecting laboratory data in ICU were blinded to group assignment of subjects. In the assessment period before intervention, we recorded the following parameters in all patients: demographic characteristics including gender, age, body weight, underlying disorders, the aetiology of hospitalisation, the type of surgery, history of surgery, previous oral medications, history of gastrointestinal disorders, drug sensitivity, endotracheal tube size, and the day of intubation. The limitations of sample size are due to prolong length of the study intervention and exclusion of nine patients because of pulmonary positive culture.
Study interventions: Bed position (HOBE 45° or 60°) was attached to the patients’ bedside for awareness of the nurses compliance with the protocol. All of the patients underwent oral and endotracheal suctioning routine care to remove secretions. The endotracheal secretions were removed before the patient position change with suctioning less than 20 seconds and pressure of 60-80 mmHg. The ETT cuff was monitored every shift to maintain pressure of 20 to 30 cm H2O at all times in both groups. Also, all patients had an ETT with a dorsal lumen above the ETT cuff to allow continuous suctioning of tracheal suctions accumulating in the subglottic area (TYCO Health Care Group LP, NO: 1-800-635-5267, made in Mexico). The 60° elevated position was maintained continuously, 24 hours a day for seven days needed for study. All patient’s position was changed every two hours and The changing of position would take about 15 minutes. The patient who got out of 60° HOBE position over six hours for a day was excluded from the study. Back and under pressure areas massage carried out for preventing bedsores. Chest and limb physiotherapy was performed daily by a trained physiotherapist. A battery of investigations was performed [{Acute Physiology and Chronic Health Evaluation II (APACHEII), a severity-of-disease classification system in ICU setting}, GCS, culture of tracheal tube and blood as main indicator and chest X-ray, Axillary temperature, tidal volume, pulmonary compliance] initially and at the end of the seven day intervention period. Pulmonary compliance and resistance were measured by the ventilator monitoring (Bennett 840).
The amount and method of patient feeding was either parenteral or enteral and depended on the order and decisions of the intensivist. Enteral feeding was given intermittently by the nurse via a nasogastric tube (16-French SUPA medical Devices NO: 19699-45411, Tehran-IRAN) with a target maximum of 1500 to 2000 mL per 24 hours. When residual measurements were more than 200 mL, at every 3 hours, enteral feeding was stopped and all decisions of enteral feeding were left to the intensivist order. All patients had a central venous catheter route for infusion therapy. Pain was managed equally in both groups and all patients were prescribed pain medication as required, according to the intensive care specialist. The pharmacological and non-pharmacological methods for the prevention of pneumonia were the same for all patients. For the pharmacological prevention of stress ulcers, all patients had a nasogastric tube in place and received Ranitidine 50 mg/TDS or Pantoprazole 40 mg/BD. All patients received a low-molecular-weight heparin for prophylaxis of Deep Vein Thrombosis (DVT) and mouth washed with chlorhexidine. Non-pharmacological methods such as implementing comprehensive oral care, continuous sub glottal suctioning, hand washing, and preventing stomach overload for all patients were the same.
Diagnosis of VAP: We applied the modified Clinical Pulmonary Infection Score (CPIS) to diagnose VAP (total score > 6 suggested VAP- [Table/Fig-1]) [22]. VAP was diagnosed with use of standard clinical and microbiological criteria in the first 24 hours as well as the seventh day of intubation. Sputum was aspirated by sterile endotracheal suction technique and collected in a sterile container by nurse for all cultures. White Blood Cell (WBC) count and gram stain were performed at the first and seventh day of admission. The clinical diagnostic criteria for infection included fever (temperature >38.2°C), leukopenia (WBC count <4000/mm3) or leukocytosis (WBC count >12000/mm3), and purulent tracheal secretions.
Clinical Pulmonary Infection Score (CPIS).
| Component | Point |
|---|
| Temperature oC |
| 36.0 ~ 38.4 | 0 |
| 38.5 ~ 38.9 | 1 |
| ≤36.0 or ≥39.0 | 2 |
| Blood leukocytes mm-3 |
| 4000 ~ 11000 | 0 |
| <4000 or >11000 | 1 |
| Tracheal secretions |
| Few | 0 |
| Moderate | 1 |
| Large | 2 |
| Purulent | +2 |
| Oxygenation Pa.O2/FI.O2 ratio (mmHg) |
| >240 or ARDS | |
| ≤240 and no ARDS | |
| Chest radiograph |
| No infiltrate | 0 |
| Patchy or diffuse infiltrate | 1 |
| Localised infiltrate | 2 |
Total points for CPIS varied from 1–10 points. Pa,O2: arterial oxygen tension; FI,O2: inspiratory oxygen fraction; ARDS: acute respiratory disease syndrome.
Statistical Analysis
Results were presented as mean±Standard Deviation (SD) for quantitative variables and were summarized by frequency (percentage) for categorical variables. Continuous variables were compared using t-test or non-parametric Mann-Whitney U test whenever the data did not appear to have normal distribution or when the assumption of equal variances was violated across the two study groups. Categorical variables were, on the other hand, compared using chi-square test or Fisher’s-exact test when more than 20% of cells with expected count of less than five were observed. Statistical software SPSS version 19.0 for Windows (SPSS Inc., Chicago, IL) was used for statistical analysis. A p-value of 0.05 or less were considered statistically significant.
Results
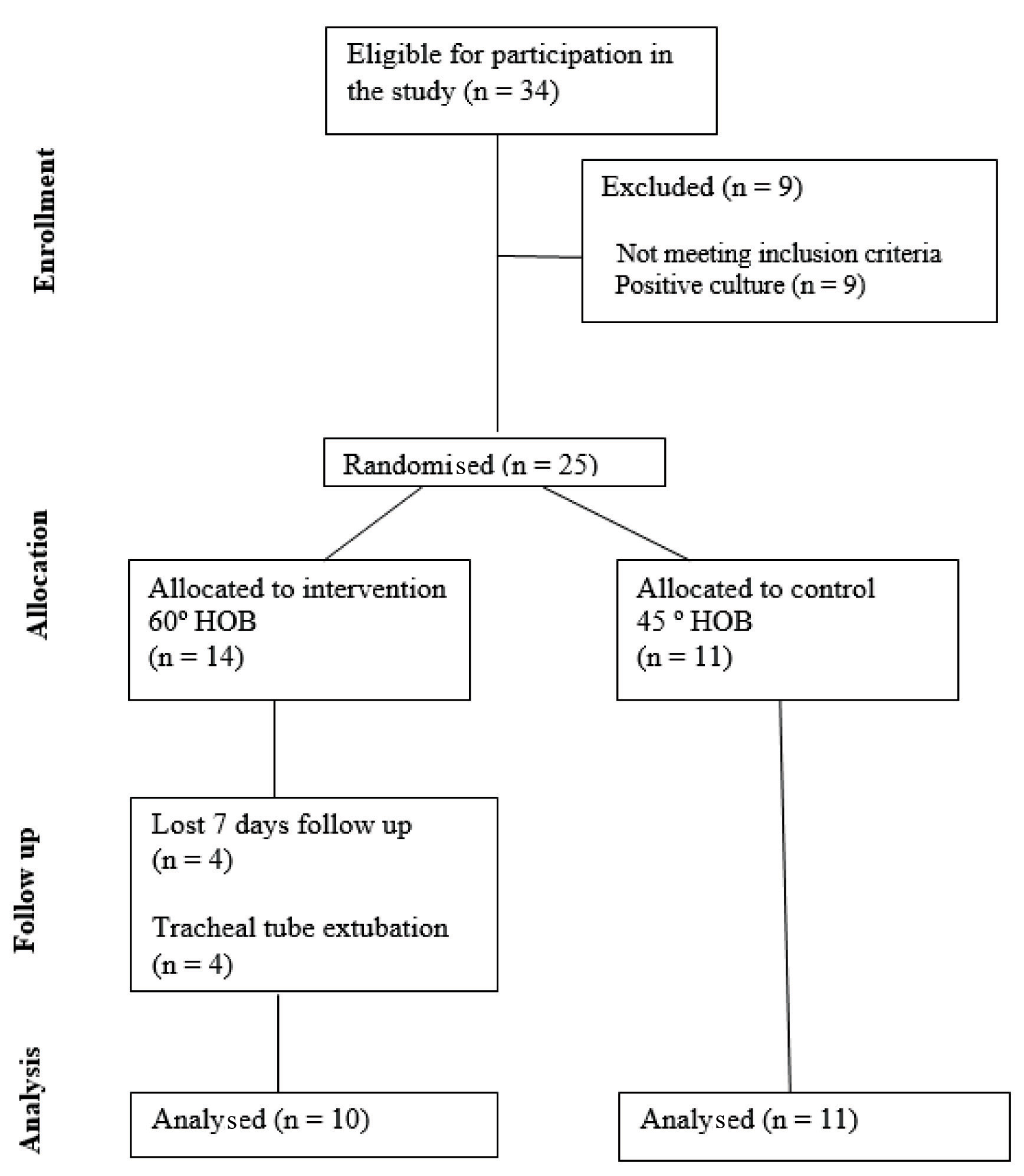
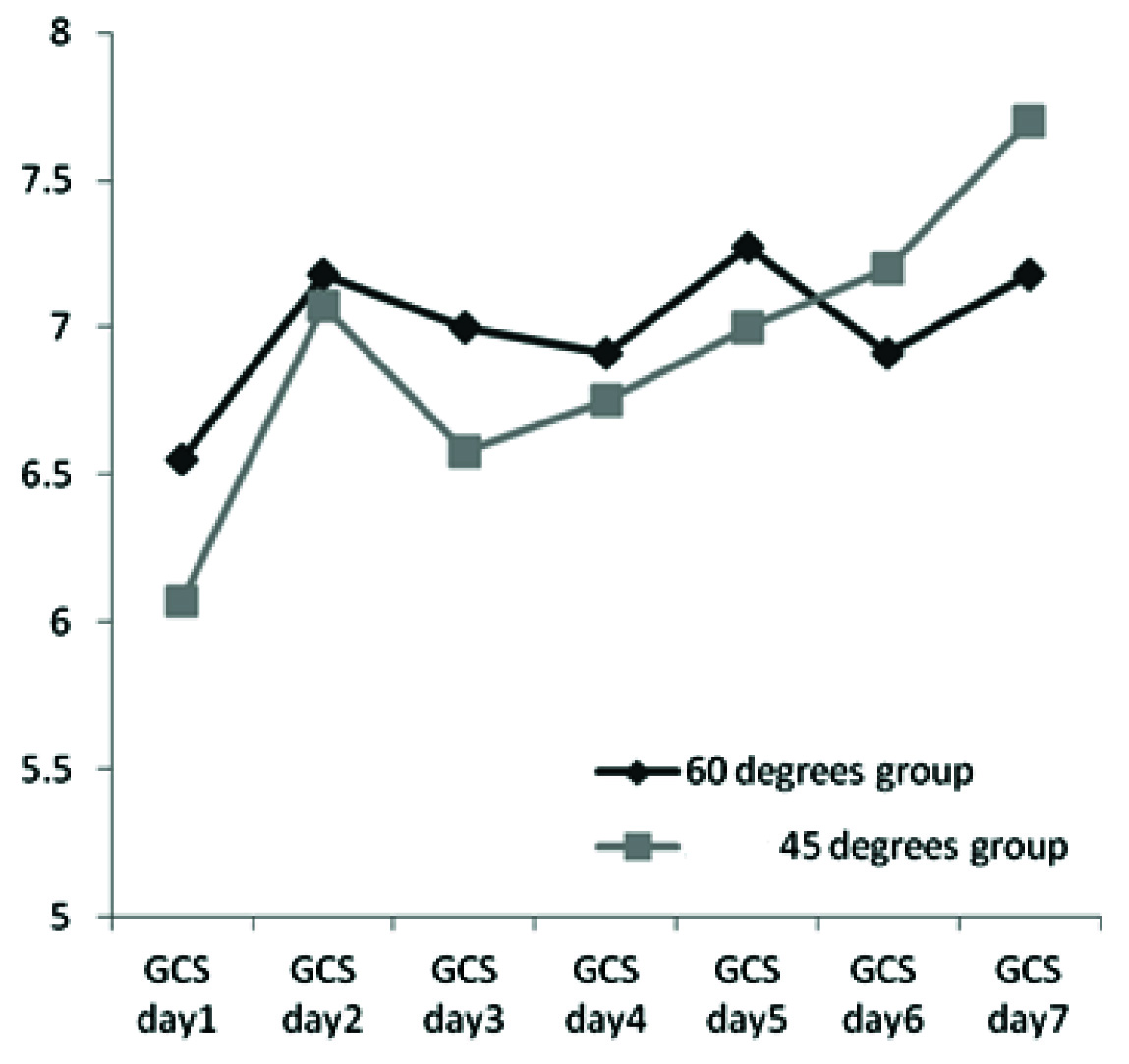
Among all 34 patients who were initially included into the study, nine were excluded because of pulmonary positive culture. Fourteen and 11 patients were included in the intervention and the control group respectively [Table/Fig-2]. There was no significant differences between the two groups with regard to baseline characteristics such as demographics, mean weight, etiology of admission as trauma, size of tracheal and nasogastric tubes, mean Glasgow Coma Score (GCS) WBC count, as well as mean APACHE II score [Table/Fig-3]. The two groups were also similar in terms of respiratory and ventilation-related haemodynamic parameters at baseline [Table/Fig-4]. The assessment of the changes in GCS score within the seven days of the study showed no significantly difference between the intervention and control groups [Table/Fig-5]. Positioning the patients in the 60° head up elevation position resulted in significantly lower pulmonary infiltration in chest X-ray, lower axillary temperature, as well as higher patient’s tidal volume and pulmonary compliance compared with the control group [Table/Fig-6]. The overall prevalence of VAP was 20% in the intervention group and 73% in the control group with a significant difference. In this regard, HOBE from 45° to 60° reduced the risk of VAP more than three times. Also, the diagnosis of VAP using the CPIS score in two groups showed no difference at baseline (p=0.53), whereas this score was significantly lower in the groups at day 7 (p=0.001).
Flow of participants through the study.
Baseline (day 1) characteristics of the study participant.
| Characteristics | Interventionalgroup (n=14) | Control group(n=11) | p-value |
|---|
| Gender, N (%) | Women | 12 (85.7) | 7 (63.6) | 0.19 |
| Men | 2 (14.3) | 4 (36.4) |
| Age (year), M±SD | 38.12±15.02 | 39.35±13.36 | 0.20 |
| Weight (kg), M±SD | 74.47±12.55 | 75.05±9.60 | 0.34 |
| Etiology of admission as trauma, N (%) | 10 (71.4) | 10 (90.9) | 0.23 |
| Size of tracheal tube (mm) M±SD | 7.82±0.25 | 7.68±0.34 | 0.25 |
| Size of nasogastric tube (mm) M±SD | 15.64±0.81 | 15.86±0.53 | 0.42 |
| Baseline GCS score M±SD | 6.07±2.23 | 6.55±1.37 | 0.54 |
| WBC count (× 102/mm3) M±SD | 7.41±2.54 | 6.93±2.48 | 0.64 |
| APACHE Π score** M±SD | 18.57±3.61 | 15.64±3.56 | 0.54 |
*p-value ≤ 0.05 is significant
**APACHEΠ: Acute Physiology and Chronic Health Evaluation
Baseline (day 1) respiratory and ventilation-related haemodynamic parameters of the study participant.
| Characteristics | InterventionalGroup M±SD | Control Group M±SD | p-value |
|---|
| Axillary temperature (°C) | 37.17±0.44 | 37.26±0.36 | 0.58 |
| Arterial oxygen saturation (%) | 99.00±1.57 | 98.36±1.75 | 0.35 |
| Arterial oxygen pressure (mmHg) | 196.86±80.25 | 176.73±48.50 | 0.47 |
| Arterial CO2 pressure (mmHg) | 30.86±6.82 | 35.05±5.25 | 0.11 |
| Ventilator oxygen capacity (%) | 56.79±12.34 | 54.09±10.91 | 0.57 |
| Ventilator respiratory rate (/minute) | 12.14±2.54 | 12.18±1.08 | 0.96 |
| Positive end expiratory pressure (mmHg) | 5.00±0.12 | 5.36±1.21 | 0.28 |
| Ventilator tidal volume (mL) | 545.00±48.44 | 498.73±171.59 | 0.34 |
| Patient’s tidal volume (mL) | 555.29±104.87 | 545.82±72.70 | 0.80 |
| Pulmonary compliance (L) | 72.36±3.15 | 69.38±9.79 | 0.29 |
| Pulmonary resistance (cmH2O/L/s) | 10.59±4.85 | 11.47±3.13 | 0.61 |
| CPIS | 0.93±0.55 | 1.35±0.86 | 0.53 |
*p-value ≤ 0.05 is significant
Trend of the changes in GCS in two study groups (p=0.729).
Outcomes of the study participant on the seventh day of intubation.
| Respiratory outcome | InterventionalGroup | Control Group | p-value | Relative Risk |
|---|
| Pulmonary infiltration in CXR | 3 (30.0) | 9 (81.8) | 0.009* | 3.10 |
| Axillary temperature (°C) | 37.28±0.90 | 38.63±0.70 | 0.001* | 3.85 |
| WBC count (× 102/mm3) | 9.39±3.45 | 12.00±6.20 | 0.225 | 1.17 |
| Prevalence of pneumonia | 2 (20.0) | 8 (72.7) | 0.016* | 3.64 |
| Arterial oxygen pressure (mmHg) | 48.90±99.88 | 35.73±51.37 | 0.704 | 1.42 |
| Patient’s tidal volume (mL) | 678.76±76.33 | 549.03±50.24 | <0.001* | 4.86 |
| Pulmonary compliance (L) | 79.05±39.15 | 52.50±8.07 | 0.038 | 2.23 |
| Pulmonary resistance (cm H2O/L/s) | 10.60±4.49 | 11.94±2.28 | 0.889 | 1.11 |
| CPIS | 3.20±2.86 | 7.64±2.42 | 0.001* | 3.72 |
*p-value ≤0.05 is significant
Discussion
Our study demonstrated that HOBE to 60° was associated with significant decreases in the incidence of VAP as well as a meaningful improvement in tidal volume and higher pulmonary compliance in comparison with the control group positioned in 45° elevation. To the best of our knowledge and based on reviewing the literature, this is the first prospective randomised controlled study investigating the effects of HOBE to 60° on pulmonary outcomes and preventing occurrence of VAP in ICU admitted patients.
In accordance with our findings, 45° HOBE improved end-expiratory lung volumes in mechanically ventilated subjects in sooner study [23] and decreased aspiration in the study of Schallom M et al., [24]. Our findings suggest that the recommended semi-upright or upright positions may be beneficial in some mechanically ventilated patients. In fact, HOBE in critically ill patients hospitalized in ICU wards, not only led to a considerable decrease in the appearance of VAP, but also significantly improved some vital pulmonary indices that can be potentially result in favourable long-term outcomes in these patients. Although, beneficial effects of the 60° HOBE has not been previously described, several trials addressed clinically suspected VAP following lower degrees of elevation. The baseline risks for clinically suspected VAP across trials ranged from 15% to 34% [22,25].
The pooled relative risk derived from the trials also showed a benefit in favor of the 45° HOBE. In a study by Torres A et al., the supine position and length of time the patient is kept in this position were shown to be potential risk factors for VAP that can be prevented by HOBE for patients [26]. The baseline mechanisms related to improvement of pulmonary indices with HOBE to higher levels have been widely investigated. It has been revealed that the obtained results can reflect an improved circulation profile with higher systemic venous return, higher cardiac output and, as a consequence, improved oxygen delivery; while adversely, lower degrees of elevation can be associated with lung de-recruitment and hypoxemia [27,28]. Positioning patients in the semirecumbent (60°) position is also associated with significant changes in intra-abdominal pressure [29-31].
This study provides a new insight into a link between the beneficial effects of the 60° HOBE positioning compared with 45° on pneumonia prevention. In fact, this new positioning can effectively improve the host response against bacterial infection and also prevent transmission of gastrointestinal pathogens to respiratory systems. In this context, involvement of the innate host immunity to protect the respiratory system against pathogenesis is also suggested [32].
It has been hypothesised that HOBE to higher degrees may change lung distension leading in turn to the release of smaller amount of some cytokines such as interleukin-8 (IL-8), thereby protecting the host from the detrimental effects of an inflammatory response [33,34].
Limitation
However, the main study limitation was the small sample size that study with large number is recommended.
Conclusion
Altogether, our findings suggest that 60° HOBE can be proposed as an efficient way to decrease VAP occurrence and improve gas exchange in mechanically ventilated ICU patients. This positioning can allow better distribution of lung inflation along the craniocaudal axis through improvement in respiratory system compliance, together with tidal volume. The major strength of the study was the statistically and clinically significant findings.
Total points for CPIS varied from 1–10 points. Pa,O2: arterial oxygen tension; FI,O2: inspiratory oxygen fraction; ARDS: acute respiratory disease syndrome.
*p-value ≤ 0.05 is significant
**APACHEΠ: Acute Physiology and Chronic Health Evaluation
*p-value ≤ 0.05 is significant
*p-value ≤0.05 is significant
[1]. Cunha BA, Pneumonia Essentials 2010 2010 Oct 22 Jones & Bartlett Publishers [Google Scholar]
[2]. Kunac A, Sifri ZC, Mohr AM, Horng H, Lavery RF, Livingston DH, Bacteremia and ventilator-associated pneumonia: a marker for contemporaneous extra-pulmonic infectionSurg Infect (Larchmt) 2014 15(2):77-83. [Google Scholar]
[3]. American Thoracic Society, Infectious Diseases Society of AmericaGuidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumoniaAm J Respir Crit Care Med 2005 171(4):388 [Google Scholar]
[4]. Ewig S, Welte T, Torres A, Is healthcare-associated pneumonia a distinct entity needing specific therapy?Curr Opin Infect Dis 2012 25(2):166-75. [Google Scholar]
[5]. Davis KA, Ventilator-associated pneumonia: A reviewJ Intensive Care Med 2006 21(4):211-26. [Google Scholar]
[6]. Koenig SM, Truwit JD, Ventilator-associated pneumonia: diagnosis, treatment, and preventionClin Microbiol Rev 2006 19(4):637-57. [Google Scholar]
[7]. Rello J, Ollendorf DA, Oster G, Vera-Llonch M, Bellm L, Redman R, Epidemiology and outcomes of ventilator-associated pneumonia in a large US databaseChest 2002 122(6):2115-21. [Google Scholar]
[8]. Palmer LB, Ventilator-associated infectionCurr Opin Pulm Med 2009 15(3):230-35. [Google Scholar]
[9]. Safdar N, Dezfulian C, Collard HR, Saint S, Clinical and economic consequences of ventilator-associated pneumonia: A systematic reviewCrit Care Med 2005 33(10):2184-93. [Google Scholar]
[10]. Lipovich CJ. Analysis of ventilator associated pneumonia patients’ hospital and intensive care charges, length of stay and mortality (doctoral dissertation, the Ohio State University), 2013 [Google Scholar]
[11]. Cunha BA, Ventilator-associated pneumonia: monotherapy is optimal if chosen wiselyCrit Care 2006 10(2):141 [Google Scholar]
[12]. Wip C, Napolitano L, Bundles to prevent ventilator-associated pneumonia: how valuable are they?Curr Opin Infect Dis 2009 22(2):159-66. [Google Scholar]
[13]. Göcze I, Strenge F, Zeman F, Creutzenberg M, Graf BM, Schlitt HJ, The effects of the semirecumbent position on hemodynamic status in patients on invasive mechanical ventilation: prospective randomized multivariable analysisCrit Care 2013 17(2):R80 [Google Scholar]
[14]. Macht M, Robinson JC, Graham BB, Updated Approach for the Assessment of Ventilator Associated PneumoniaCrit Care Med 2013 41(11):01-03. [Google Scholar]
[15]. Thakuria B, Singh P, Agrawal S, Asthana V, Profile of infective microorganisms causing ventilator-associated pneumonia: A clinical study from resource limited intensive care unitJ Anaesthesiol Clin Pharmacol 2013 29(3):361 [Google Scholar]
[16]. Craven RF, Hirnle CJ, Jensen S, Fundamentals of nursing: Human health and function 2013 7th edPhiladelphia, PAWolters Kluwer Health/Lippincott Williams & Wilkins [Google Scholar]
[17]. Burk RS, Grap MJ, Backrest position in prevention of pressure ulcers and ventilator-associated pneumonia: conflicting recommendationsHeart Lung 2012 41(6):536-45. [Google Scholar]
[18]. Joseph NM, Sistla S, Dutta TK, Badhe AS, Parija SC, Ventilator-associated pneumonia in a tertiary care hospital in India: incidence and risk factorsJ Infect Dev Ctries 2009 3(10):771-77. [Google Scholar]
[19]. Metheny NA, Frantz RA, Head-of-bed elevation in critically ill patients: a reviewCrit Care Nurse 2013 33(3):53-67. [Google Scholar]
[20]. Wang L, Li X, Yang Z, Tang X, Yuan Q, Deng L, Sun X, Semi-recumbent position versus supine position for the prevention of ventilator-associated pneumonia in adults requiring mechanical ventilationCochrane Libr 2016 (1):1-55. [Google Scholar]
[21]. Drakulovic MB, Torres A, Bauer TT, Nicolas JM, Nogué S, Ferrer M, Supine body position as a risk factor for nosocomial pneumonia in mechanically ventilated patients: a randomised trialLancet 1999 354(9193):1851-58. [Google Scholar]
[22]. O’Horo JC, Kashyap R, Herasevich V, Sampathkumar P, The clinical pulmonary infection score and ventilator associated eventsAm J Respir Crit Care Med 2014 189:4563 [Google Scholar]
[23]. Spooner AJ, Corley A, Sharpe NA, Barnett AG, Caruana LR, Hammond NE, Head-of-bed elevation improves end-expiratory lung volumes in mechanically ventilated subjects: a prospective observational studyRespir Care 2014 59(10):1583-89. [Google Scholar]
[24]. Schallom M, Dykeman B, Metheny N, Kirby J, Pierce J, Head-of-bed elevation and early outcomes of gastric reflux, aspiration and pressure ulcers: a feasibility studyAm J Crit Care 2015 24(1):57-66. [Google Scholar]
[25]. Keeley L, Reducing the risk of ventilator-acquired pneumonia through head of bed elevationNurs Crit Care 2007 12(6):287-94. [Google Scholar]
[26]. Torres A, Serra-Batlles J, Ros E, Piera C, de la Bellacasa JP, Cobos A, Pulmonary aspiration of gastric contents in patients receiving mechanical ventilation: the effect of body positionAnn Intern Med 1992 116(7):540-43. [Google Scholar]
[27]. Richard JC, Maggiore SM, Mancebo J, Lemaire F, Jonson B, Brochard L, Effects of vertical positioning on gas exchange and lung volumes in acute respiratory distress syndromeIntensive Care Med 2006 32(10):1623-26. [Google Scholar]
[28]. Robak O, Schellongowski P, Bojic A, Laczika K, Locker GJ, Staudinger T, Short-term effects of combining upright and prone positions in patients with ARDS: a prospective randomized studyCrit Care 2011 15(5):R230 [Google Scholar]
[29]. Ejike JC, Kadry J, Bahjri K, Mathur M, Semi-recumbent position and body mass percentiles: effects on intra-abdominal pressure measurements in critically ill childrenIntensive Care Med 2010 36(2):329-35. [Google Scholar]
[30]. McBeth PB, Zygun DA, Widder S, Cheatham M, Zengerink I, Glowa J, Effect of patient positioning on intra-abdominal pressure monitoringAm J Surg 2007 193(5):644-47. [Google Scholar]
[31]. Yi M, Leng Y, Bai Y, Yao G, Zhu X, The evaluation of the effect of body positioning on intra-abdominal pressure measurement and the effect of intra-abdominal pressure at different body positioning on organ function and prognosis in critically ill patientsJ Crit Care 2012 27(2):222-e1. [Google Scholar]
[32]. Ladoire S, Pauchard LA, Barbar SD, Tissieres P, Croisier-Bertin D, Charles PE, Impact of the prone position in an animal model of unilateral bacterial pneumonia undergoing mechanical ventilationAnesthesiology 2013 118(5):1150-59. [Google Scholar]
[33]. Charles PE, Barbar SD, Toll-like receptors: a link between mechanical ventilation, innate immunity and lung injury?Intensive Care Med 2010 36:909 [Google Scholar]
[34]. Villar J, Cabrera N, Casula M, Flores C, Valladares F, Muros M, Mechanical ventilation modulates Toll-like receptor signaling pathway in a sepsis-induced lung injury modelIntensive Care Med 2010 36(6):1049-57. [Google Scholar]