From scepticism to optimistic acceptance; from development of suitable instruments to publication of supporting literature, OPCABG is widely practiced now, depending on the learning curve of the surgeon [1,2]. A combination of surgical manoeuvres help in preventing conduction and hemodynamic deterioration which might occur during the graft positioning on the beating heart. These include the trendelenburg position, fluid administration and use of vasopressors and inotropes if necessary. Inotropes are administered to increase myocardial contractility whereas, vasopressors agents are administered to increase the vascular tone [3]. Advances in perioperative care have been identified and linked to improvements in the outcome of CABG [4].
Off-pump coronary artery bypass graft eliminates the alternative physiology of cardiopulmonary bypass. However, marked hypotension is seen to occur intraoperatively in some patients with bad left ventricle. Preference of inotropes not only depends on the patients but also on the anaesthetist and their experience. There is dearth of data regarding the use of inotrope in patients undergoing OPCABG. This study was done with an attempt to look into the intraoperative and immediate post-operative use of inotropes in a multispecialty hospital of South India.
Materials and Methods
This was a prospective observational study done in the adult cardiac surgery unit of Apollo Hospitals, Greams Road, Chennai, Tamil Nadu, India, during 1st August 2011 to 31st October 2011. Ethics Committee approval was obtained. Convenience sampling was done and all the patients undergoing OPCABG during this period were included in the study after obtaining informed consent. Patients not willing to participate were excluded from the study. Patients receiving any inotropes post-operatively up to 12 hours after skin closure including any agents initiated pre-operatively or intraoperatively were studied in detail. Inotropic support was defined as the use of dopamine ≥5 microgram/kilogram/minute, any dose of Adrenaline, Noradrenaline, Dobutamine, Isoprenaline, Vasopressin or Milrinone.
Statistical Analysis
The data was collected in a structured performa validated for content and entered in the excel sheet. Analysis was done using SPSS version 16.0. Descriptive data was expressed using percentages and frequencies. Chi-square was done to assess the association of age, gender, serum creatinine, ejection fraction, graft number, graft type with use of the inotropes at a significance level of p-value <0.05.
Results
A total of 180 patients undergoing OPCABG were included in the study. The age ranged from 31 to 86 years with a mean age of 59±10.18 years. Majority of patients, 80 (44.4%) fell in the age group 61-75 years closely followed by those in 46-60 years 79 (43.9%) while 14 (7.8%) and seven (3.9%) were in age groups 31-45 years and 76-90 years respectively. There were 161 males and 19 females. [Table/Fig 1] highlights the pre-operative profile of the patients included in the study. During surgery 129 (71.7%) received three grafts, 20 (11.1%) received two, 18 (10%) received four, nine (5%) received only a single graft and 4 (2.2%) received up to five grafts.
| Variables | N=180 (%) | Males (n=161) | Females (n=19) |
|---|
| Comorbidities Diabetes | 103 (57.2) | 89 | 14 |
| Hypertension | 105 (58.3) | 88 | 17 |
| Previous Myocardial Infarction (MI) | 30 (16.7) | 25 | 5 |
| Asthma | 2 (1.1) | 1 | 1 |
| Hypothyroidism | 6 (3.3) | 5 | 1 |
| Smoking | 46 (25.6) | 46 | 0 |
| Alcoholism | 27 (15) | 27 | 0 |
| Elevated serum creatinine* | 108 (60) | 98 | 10 |
| Moderately reduced EF** | 59 (32.8) | 49 | 10 |
| Abnormal Preoperative ECG*** | 133 (73.9) | 119 | 14 |
| Haemoglobin<12g% | 26 (14.44) | 21 | 5 |
*Serum creatinine ≥1.1 mg% in females and ≥1.3 mg% in males
**Moderately reduced Ejection fraction=30-49%
***Abnormal ECG=Includes changes of anterior wall MI, Inferior wall MI, Broad QRS, Right Bundle Branch Block
Perioperative Inotrope Use
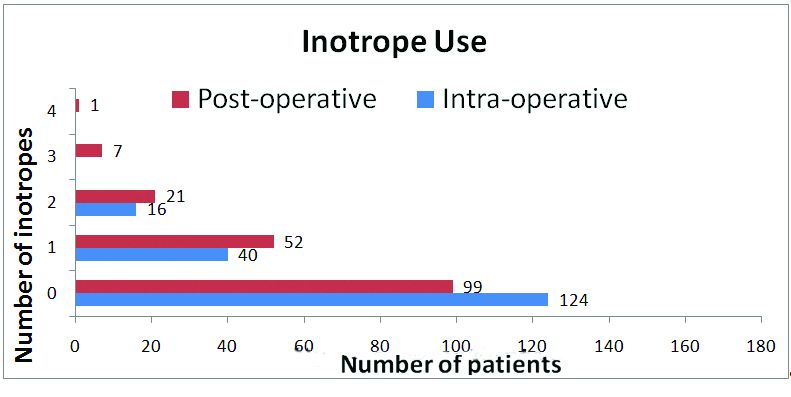
Out of the 180 patients studied 56 (31.1%) received inotropes intraoperatively and 81 (45%) received inotropes immediate post-operatively. The number of inotropes used is shown in [Table/Fig-2]. About 16 (8.89%) patients intraoperatively and 29 (16.11%) post-operatively received more than one inotropic support. Dopamine was used in a dilution of 200 mg/50 mL, Dobutamine 250 mg/50 mL, Noradrenaline 4 mg/50 mL, Adrenaline 2 mg/50 mL, Isoprenaline 1 mg/250 mL, Milrinone 25 mg/100 mL and Vasopressin 20 units/50 mL. As shown in [Table/Fig-3] the most commonly used inotrope was noradrenaline both intraoperatively and post-operatively. All the patients who received inotropes intraoperatively received noradrenaline. As shown in [Table/Fig-4], age of the patient, smoking status, moderately reduced ejection fraction (30-49%), left main coronary disease as well as use of two or more grafts was significantly related to intraoperative inotrope use. Variables influencing postoperative inotrope use were moderately reduced ejection fraction, left main coronary artery disease and use of two or more grafts as shown in [Table/Fig-5].
Number of inotropes used intra and post-operatively.
Intraoperative and immediate post-operative inotrope use.
| Intraoperative | N=180 (%) | Post-operative | N=180 (%) |
|---|
| Inotropes not received | 124 (68.9) | Inotropes not received | 99 (55) |
| Inotropes received* | 56 (31.1) | Inotropes received* | 81 (45) |
| Noradrenaline | 56 (31.1) | Noradrenaline | 69 (38.3) |
| Adrenaline | 16 (8.89) | Adrenaline | 21 (11.7) |
| | Dopamine | 16 (8.9) |
| | Dobutamine | 4 (2.2) |
| | Isoprenaline | 4 (2.2) |
| | Vasopressin | 1 (0.005) |
| | Milrinone | 1 (0.005) |
* Out of the 56 patients who received inotropes intraoperatively 16 patients received more than one inotrope and out of the 81 patients who received inotropic support post-operatively 29 patients received more than one inotropic support
Factors determining intraoperative inotrope use.
| Inotrope Use | Intraoperative (n=56) | Chi-squarevalue | Odds Ratio (95% CI, p-value) |
|---|
| Gender |
| M:F | 49:7 | 0.33 | 0.75 (0.28-2.02, 0.57) |
| Age group (years) |
| 31-45 | 7 | 2.52 | 0.42 (0.14-1.30, 0.11) |
| 46-60 | 18 | 4.55 | 2.04 (1.05-3.96, 0.03)* |
| 61-75 | 26 | 0.13 | 0.89 (0.47-1.68, 0.72) |
| 76-90 | 5 | 5.52 | 0.17 (0.03-0.89, 0.02)* |
| Diabetes | 27 | 2.7 | 0.59 (0.31-1.11, 0.10) |
| Hypertension | 30 | 0.76 | 0.75 (0.40-1.42, 0.38) |
| Hypercholesterolemia | 9 | 0.17 | 1.20 (0.50-2.90, 0.68) |
| Smoking | 20 | 4.4 | 2.09 (1.04-4.20, 0.04)* |
| Alcoholism | 12 | 2.64 | 1.98 (0.86-4.57, 0.11) |
| Elevated creatinine | 30 | 1.4 | 1.09 (0.58-2.06, 0.27) |
| Moderately reduced ejection fraction | 27 | 8.79 | 2.68 (1.38-5.18, 0.003)* |
| Left coronary artery disease | 47 | 4.86 | 1.30 (0.03-0.49, 0.001)* |
| Number of grafts ≥2 | 56 | 4.28 | 1.93 (0.88-0.97, 0.04)* |
| Haemoglobin <12 gm% | 4 | 3.5 | 0.36 (0.12-1.10, 0.06) |
*Significant
Factors determining post-operative inotrope use.
| Inotrope Use | Post-operative(n=81) | Chi-squarevalue | Odds Ratio (95% CI, p-value) |
|---|
| Gender |
| M:F | 72:9 | 0.07 | 1.14 (0.44-2.99, 0.79) |
| Age group (years) |
| 31-45 | 7 | 0.15 | 0.80 (0.27-2.40, 0.69) |
| 46-60 | 33 | 0.59 | 1.26 (0.69-2.29, 0.44) |
| 61-75 | 37 | 0.09 | 0.91 (0.51-1.65, 0.76) |
| 76-90 | 4 | 0.43 | 0.60 (0.13-2.77, 0.51) |
| Diabetes | 45 | 0.17 | 0.88 (0.48-1.60, 0.68) |
| Hypertension | 44 | 0.98 | 0.74 (0.41-1.24, 0.32) |
| Hypercholesterolemia | 14 | 0.96 | 1.51 (0.66-3.49, 0.33) |
| Smoking | 24 | 1.28 | 1.47 (0.75-2.89, 0.26) |
| Alcoholism | 13 | 0.13 | 1.16 (0.51-2.63, 0.72) |
| Elevated creatinine | 37 | 0.06 | 0.93 (0.52-1.68, 0.81) |
| Moderately reduced ejection fraction | 45 | 9.09 | 2.64 (1.39-5.01, 0.003)* |
| Left coronary artery disease | 72 | 4.67 | 2.50 (0.07-0.97, 0.03)* |
| Number of grafts ≥2 | 80 | 4.36 | 7.03 (1.86-5.46, 0.04)* |
| Haemoglobin <12g% | 8 | 2.48 | 0.49 (0.20-1.20, 0.11) |
| Packed red cell transfusion | 51 | 0.01 | 0.97 (0.53-1.79, 0.93) |
| Arrhythmias | 14 | 0.04 | 1.08 (0.49-2.38, 0.84) |
*Significant
Discussion
Off-pump CABG is safe, cost-effective and reproducible surgical technique which has revolutionized the access of coronary techniques to the developing and the under developed countries [1]. It has stood the trials of criticism for suboptimal anastomoses in the Beating Heart Against Cardioplegic Arrest Studies (BHACAS 1 and 2) and was found to have positive outcome in terms of reduced chest infections, inotrope requirements, arrhythmias, total drainage of the chest tubes, requirement of transfusions, intubation, intensive care and hospital stay [5]. Evidence points out that in the elderly, OPCABG has decreased the occurrence of low output syndrome. In the obese, OPCABG is associated with significant benefit for in hospital mortality, arrhythmias as well as inotrope use [6,7]. McKinlay KH et al., opined that the combined CABG and valve surgery requires more inotrope support than CABG alone [8].
The appropriate use of vasoactive drugs facilitates the clinical recovery by enhancing the cardiac output and vascular tone. Pharmacological support is necessary during and after weaning from cardiopulmonary bypass with low cardiac output syndrome [9]. The peri-operative inotrope use in OPCABG is a less explored, less researched area. This is an attempt, to look into, the pattern of inotropes used as well as the factors determining inotrope use in patients undergoing all OPCABG during the study period.
Dopamine at intermediate dose of 5-10 microgram/kilogram/minute increases the cardiac contractility and chronotropy. Dobutamine despite its mild chronotropic effect increases the myocardial oxygen consumption. Noradrenaline is a powerful vasoconstrictor with minimal chronotropic effect and less potent direct inotropic property [10]. Epinephrine increases the cardiac output and heart rate, mean arterial blood pressure and blood flow to the coronaries [3]. Isoprenaline has powerful chronotropic and inotropic actions. Vasopressin causes dose dependent increase in systemic vascular resistance and accentuates the vascular sensitivity to norepinephrine. Milrinone is a potent inotrope as well as vasodilator and improves the diastolic relaxation [10]. In off-pump patients, Milrinone improve the haemodynamic indexes that deteriorate during surgery [11].
In this centre the commonly used inotropes were dopamine, Adrenaline, Noradrenaline, Dobutamine, Isoprenaline, Milrinone and Vasopressin; the most common being noradrenaline both intraoperatively as well as in the immediate post-operative period. Of the 56 (31.1%) patients who received inotropes intraoperatively, 40 (22.2%) received only a single inotrope. Post-operatively 81 (44.8%) patients received inotropes, of which 52 (28.8%) received a single inotrope and 29 (16.1%) received more than one. This is in contrast to a study by Kaushish R et al., where 90.5% undergoing OPCABG had inotropic support intraoperatively of which 67.1% received a single and 23.4% received more than one inotrope [12]. During the immediate postoperative period, inotropes are more used as a standard protocol in cardiopulmonary bypass to facilitate recovery [4]. Several studies have demonstrated the reduction in inotrope use with OPCABG [5,7].
From various studies, it was observed that, advancing age, reduced ejection fraction, cardiac index ≤2.5 L/min/m2, left ventricular end diastolic pressure ≥20 mmHg, females, cardiomegaly, history of congestive cardiac failure, pre-operative atrial fibrillation, arrhythmias, severe mitral regurgitation, emergency operation, recent myocardial infusion, peripheral vascular disease, chronic kidney disease (Stage three to five), on pump surgeries, prolonged duration of bypass, left main coronary artery disease and three vessel coronary artery disease are found to be the risk factors associated with need for inotropes [13-16].
In line with other studies [14-16], the present study points out that advancing age of the patient is associated with pre-operative inotrope use. We did not find any significant association between particular gender which is consistent with Ahmed I et al., and in contrast to Rao V et al., [14,16]. Smoking status (OR=2.09) was found to be a predictor of intraoperative inotrope use which could be indirectly linked to the presence of peripheral vascular disease. Hernandez AF et al., points out that presence of peripheral vascular disease increased the inotrope use with OR being 1.28 [13]. In line with other studies, we found that moderately reduced ejection fraction significantly increased the intraoperative (OR=2.68) and post-operative inotrope use (OR=2.64). Ahmed I et al., states that left ventricular ejection fraction <40% is an independent predictor of inotrope use [14]. Rao V et al., pointed out that left ventricular ejection fraction less than 20% was a risk factor for increased use of inotropic support [16]. Left coronary disease and use of two or more grafts were the other variables that indirectly predicted the inotrope use both intraoperatively as well as post-operatively. This can be attributed to the fact that left side disease and presence of more than two grafts both indirectly mean more cardiac compromise necessitating the use of inotropes. Hernandez AF et al., as well as Rao V et al., states that three vessel coronary artery disease and left main coronary artery disease were predictors of inotrope use [13,16].
Literature points out that on pump CABG alone or with valve surgeries in itself increases the demand for inotropic support [8,13,15]. Kaushish R et al., states that the use of multiple drugs in the immediate post-operative period was lower in the OPCABG (23.4%) as compared to conventional CABG (39%) patients [12].
Limitation
Our study, inevitably, has limitations as it is a single institution study. Initiation of inotropes are at the discretion of the anaesthesiologist or intensivist which might have caused selection bias.
Conclusion
Moderately reduced ejection fraction, left main coronary artery disease and presence of more than two grafts predict the inotrope requirement intra and post-operatively. We believe that this study would add on to literature on off pump CABG. Further studies need to be conducted with more sample and longer duration comparing the inotrope use in off pump and on pump CABG surgeries.
*Serum creatinine ≥1.1 mg% in females and ≥1.3 mg% in males
**Moderately reduced Ejection fraction=30-49%
***Abnormal ECG=Includes changes of anterior wall MI, Inferior wall MI, Broad QRS, Right Bundle Branch Block