ER PR Positive Vulval Leiomyoma with Myxoid Change Mimicking Bartholin’s Cyst- A Rare Presentation
Mithila Bisht1, Ranjan Agrawal2, Menka Verma3, Parbodh Kumar4
1 Assistant Professor, Department of Pathology, Rohilkhand Medical College and Hospital, Bareilly, Uttar Pradesh, India.
2 Professor, Department of Pathology, Rohilkhand Medical College and Hospital, Bareilly, Uttar Pradesh, India.
3 Senior Resident, Department of Obstetrics and Gynaecology, Dr. Bsa Medical College and Hospital, New Delhi, India.
4 Professor and Head, Department of Pathology, Rohilkhand Medical College and Hospital, Bareilly, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mithila Bisht, Assistant Professor, Department of Pathology, Rohilkhand Medical College and Hospital, Bareilly-243006, Uttar Pradesh, India.
E-mail: dr.mithila@gmail.com
Vulval leiomyomas are rare entities which are seen in the reproductive age group. They are most commonly misdiagnosed as Bartholin’s cyst or Bartholin’s abscess when presenting with features of inflammation. Excisional biopsy is the treatment of choice. Besides this, Estrogen Receptor (ER) and Progesterone Receptor (PR) positivity implicates the usefulness of adjuvant hormonal therapy. We present a case of 38-year-old female who presented with a vulval swelling. She was misdiagnosed clinically as Bartholin’s cyst. Marsupialization of the cyst was done and tissue was sent for histopathology. Microscopy confirmed the diagnosis of vulval leiomyoma with myxoid changes. Additionally, immunohistochemical stains were was also applied, which showed positivity for Vimentin, Desmin, ER and PR and negativity for Pan Cytokeratin (CK), S100. ER and PR positivity is a rare finding in case of leiomyoma with myxoid changes.
Diagnosis, Extrauterine, Fibroid, Immunohistochemistry, Vulval mass
Case Report
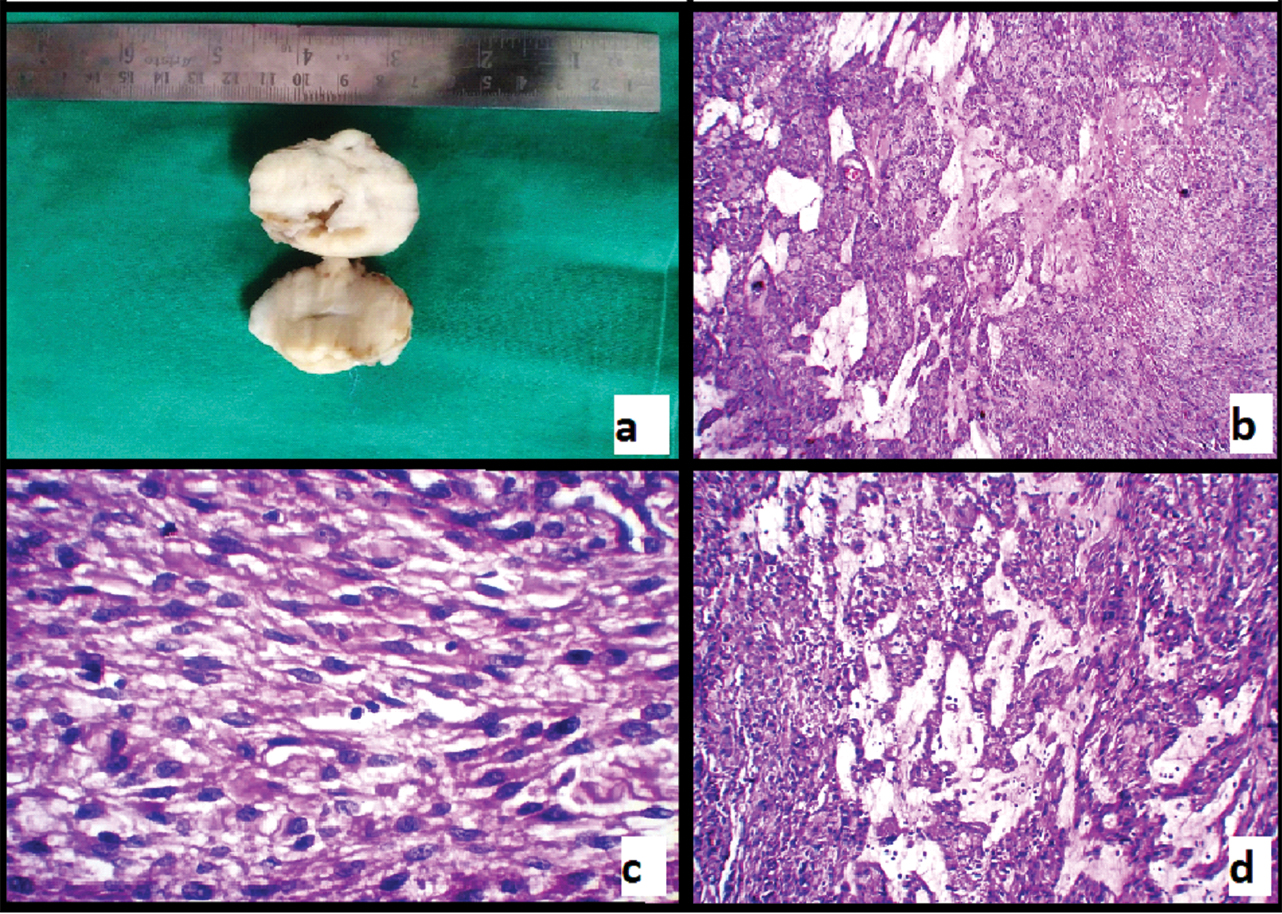
A 38-year-old female reported to the Gynaecology OPD with complaints of burning micturition and a mass in the vulval region for 10 years. She was diagnosed as Bartholin’s cyst and planned for surgery. The patient refused surgery due to some family commitments. She returned later with complaints of increasing discomfort during sitting due to the vulval mass and dribbling of urine since three months. Marsupialisation of the Bartholin’s cyst was planned. The excised mass was sent for histopathological examination. An encapsulated soft tissue piece measuring (4 cm × 3.5 cm × 3 cm) was received. The outer surface was smooth and regular. Cut surface was grey white and glistening, and showed a noticeable whorling pattern [Table/Fig-1a]. Haematoxylin and eosin stained sections showed bundles of proliferating smooth muscle fibres arranged as interlacing fascicles and whorls [Table/Fig-1a,d]. Areas of myxomatous degeneration were also present [Table/Fig-1d]. No features of atypia were noted.
a) Gross appearance of tumour showing cut section; b) Low power view showing the cellular and myxoid areas (H&E; 10X); c) High power view showing spindle shaped smooth muscle cells (H&E; 40X); d) Low power view showing myxoid degeneration (H&E; 10X).
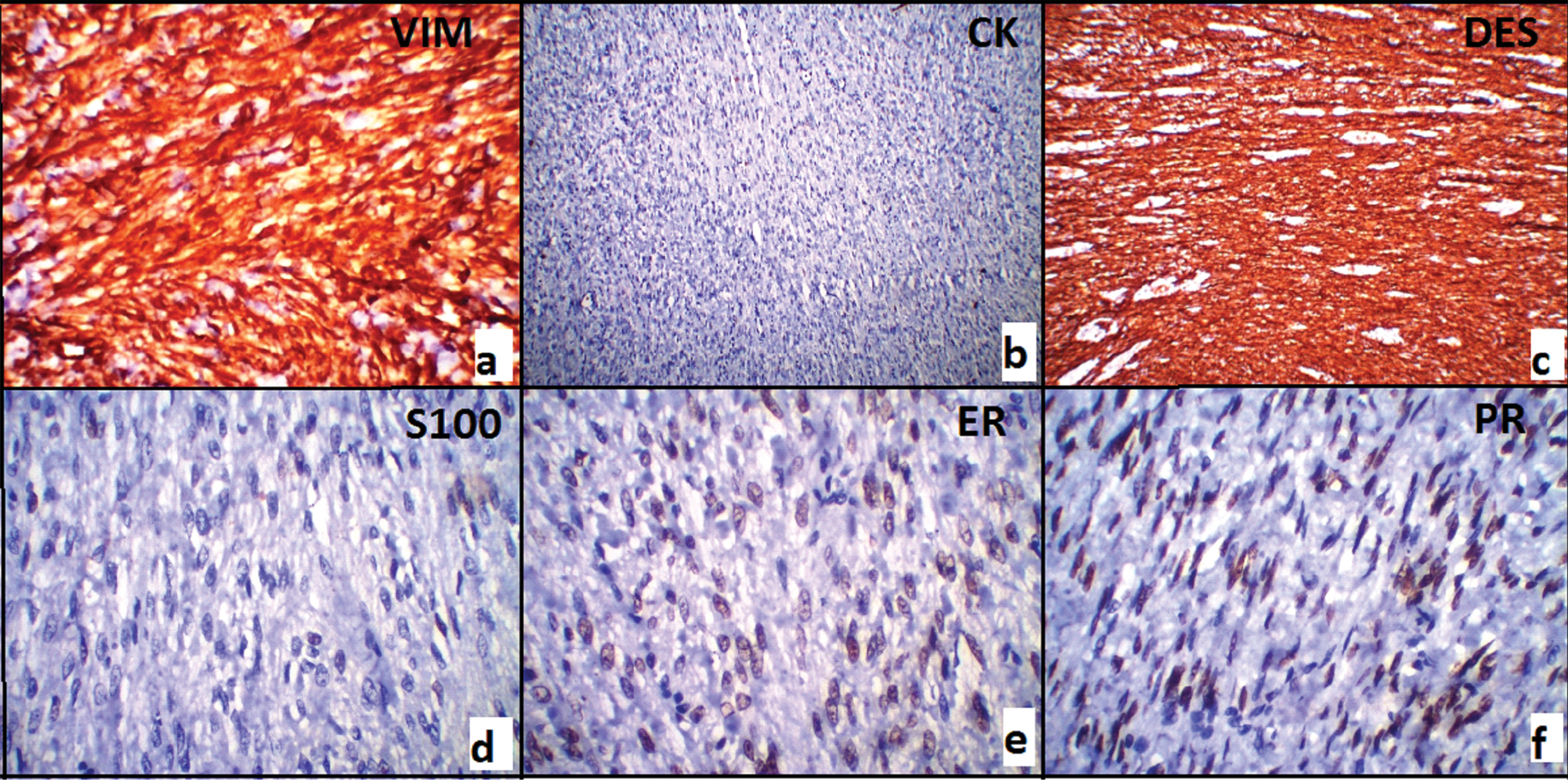
The sections were further subjected to immunohistochemical studies [Table/Fig-2a,f]. A panel of immunohistochemical markers was applied viz., vimentin, cytokeratin, desmin, S100 and hormone receptor status markers i.e., ER and PR were also studied. Vimentin and desmin showed strong cytoplasmic positivity confirming the morphological diagnosis of vulval leiomyoma. Pan CK and S100 were negative in the tumour cells. Based on the Allred scoring [1], ER and PR came out to be positive in the nuclei of the spindle shaped tumour cells. Based on the light microscopic and immunohistochemical findings, a final diagnosis of vulval leiomyoma with myxoid changes was given. On follow up till one year duration, the patient recovered progressively with gradual alleviation of her symptoms. After one year, the patient lost to follow up.
a) Vimentin positivity (40X); b) Cytokeratin negativity (10X); c) Desmin positivity (40X); d) S100 negativity (40X); e) ER positivity (40X); f) PR positivity (40X).
Discussion
Leiomyomas are a very common occurrence in uterine wall but their occurrence in the vulva is rare [2]. Extrauterine leiomyomas are rare and can affect the urinary bladder, labia majora, labia minora, ovaries and urethra [3]. Leiomyoma is a rare entity in vulva, where it is misinterpreted clinically as Bartholin’s cyst most of the times. These benign smooth muscle tumours may arise from the erector pili muscle, the erectile tissue or at the insertions of the round ligaments and are usually well circumscribed [4]. Uterine leiomyomas are seen in about 30% of >35 years age group females while vulval leiomyomas most commonly affect women in their 5th or 6th decade [5,6]. Vulval leiomyomas are rare and closely mimic bartholin’s cyst clinically. Till date only about 160 cases of vulval leiomyomas have been reported in the literature [7].
Leiomyomas arising from uterine smooth muscle cells are termed fibroids and are of very common occurrence. They represent the most common gynaecologic and uterine neoplasms. Approximately, 20%–30% of women older than 35 years have uterine leiomyomas that are manifested clinically [7]. Besides the sites mentioned above, other rare sites for extrauterine leiomyoma are sinonasal cavities, orbits, kidneys, and skin [5,8,9].
Extrauterine leiomyomas pose a diagnostic challenge especially in vulva where they mimic bartholin’s cyst clinically. Smooth Muscle Tumours (SMTs) of vulva are rare entity. Its incidence varies from 0.07% to 0.42% [10]. The leiomyomas of uterus arise from the myometrial smooth muscle cells, but the leiomyomas of vulva are said to arise the network of muscle fibers that lie in the deep dermis or from the smooth muscle of the blood vessel wall, erectile tissue or round ligament remnant within the labium majus [1,2,10].
The diagnosis requires microscopic examination, where proliferation of benign smooth muscle cells is seen. Features that define risk of recurrence are a gross diameter of 5 cm or greater, an infiltrative margin, a mitotic count of five or more per 10 high power fields and grade two to three atypia [11]. None of these features was present in our case.
Immunohistochemically, ER and PR are expressed in 73.7% and 85% of SMTs of vulva, respectively. However, smooth muscle tumours of vulva with myxoid change are generally associated with absence of ER and PR expression. Such observations suggest that myxoid changes possibly suppress the ER/PR expression in vulval SMTs [12]. It is noteworthy that, our case showed myxoid changes but, immunohistochemistry revealed nuclear immunoreactivity for ER and PR in the smooth muscle cells.
Uterine leiomyoma arises from ER/PR expressing myometrial cells. So, the hormone receptors, ER and PR are expressed in uterine leiomyoma. On the other hand, smooth muscle tumours of vulva are considered to have originated from smooth muscle cells of the erectile tissue or the blood vessels. Studies have also hypothesised their origin from the smooth muscles of dartos or from the round ligament or the errector pili muscle [3]. All these structures lack intrinsic ER/PR expression. Hodgins MB et al., carried out a study in London (UK) to map the sites for sex steroid action in the human vulva. They studied the ER/PR expression in vulval tissue wherein they found out that in the epidermal and fibroblastic cells, ER staining is significantly low in labia minora, labia majora and suprapubic skin as compared to vagina. Also, except for their presence in few sweat glands, ER receptor expression was virtually absent in skin appendages, blood vessels, and lymphatics [13]. They also observed in their study that, PR immunostaining was not seen in vulva. Still, more studies need to be done to understand the pattern and importance of ER and PR receptor status in vulval leiomyomas.
Conclusion
Extrauterine leiomyomas are of a rare occurrence. In vulva, leiomyomas arise from the smooth muscle cells within erectile tissue, blood vessel walls or round ligament remnants in the labia majora. Vulval leiomyomas, of the labia are most commonly clinically mistaken for bartholin’s cyst and pose a diagnostic challenge therefore, they must be kept in the differential diagnosis of vulval masses. Histopathology and immunohistochemistry aid in the definitive diagnosis. More studies need to be done to decipher the role of ER PR receptor status in vulval leiomyomas.
[1]. Qureshi A, Pervez S, Allred scoring for ER reporting and its impact in clearly distinguishing ER negative from ER positive breast cancersJ Pak Med Assoc 2011 60(5):350-53. [Google Scholar]
[2]. Amudha P, Kalarani E, Karthika Devi A, Swathi M, Vulval leiomyoma: a rare clinical entityInt J Reprod Contracept Obstet Gynecol 2016 5(4):1254-56. [Google Scholar]
[3]. Szklarukj Tamm EP, Choi H, Varavithya V, MR imaging of common and uncommon large pelvic massesRadiographics 2003 23(2):403-24. [Google Scholar]
[4]. Kaufman RH, Gardner HL, Tumours of the vulva and vagina. Benign mesodermal tumoursClin Obstet Gynecol 1965 8(4):953-81. [Google Scholar]
[5]. Fasih N, Prasad Shanbhogue A, Macdonald DB, Fraser-Hill MA, Papadatos D, Kielar AZ, Leiomyomas beyond the Uterus: Unusual Locations, Rare ManifestationsRadioGraphics 2008 28(7):1931-48. [Google Scholar]
[6]. Guardiola MT, Dobin SM, Dal Cin P, Donner LR, Pericentric inversion (12) (p12q13-14) as the sole chromosomal abnormality in a leiomyoma of the vulvaCancer Genet Cytogenet 2010 199(1):21-23. [Google Scholar]
[7]. Kurdi S, Arafat A, Almegbel M, Aladham M, Leiomyoma of the Vulva: A Diagnostic Challenge Case ReportCase Reports in Obstetrics and Gynecology 2016 2016:01-03. [Google Scholar]
[8]. Buttram VC Jr, Reiter RC, Uterine leiomyomata: etiology, symptomatology, and managementFertil Steril 1981 36(4):433-45. [Google Scholar]
[9]. Agrawal R, Kumar M, Agrawal L, Agrawal KK, A Huge Primary Ovarian Leiomyoma with Degenerative Changes-An UnusualJ Clin Diagn Res 2013 7(6):1152-54. [Google Scholar]
[10]. Kajiwara H, Yasuda M, Yahata G, Yamauchi I, Satoh S, Hirasawa T, Myxoid leiomyoma of the vulvaTokai J Exp Clin Med 2002 27:57-64. [Google Scholar]
[11]. Nielsen GP, Rosenberg AE, Koerner FC, Young RH, Scully RE, Smooth-muscle tumours of the vulva: A clinicopathological study of 25 cases and review of the literatureAm J Surg Pathol 1996 20:779-93. [Google Scholar]
[12]. Khandeparkar S, Deshmukh S, Bhayekar P, A rare case of lipoleiomyoma of the vulva: Cytological and immunohistopathological studyJ Midlife Health 2013 4(4):238-40. [Google Scholar]
[13]. Hodgins MB, Spike RC, Mackie RM, MacLean AB, An immunohistochemical study of androgen, oestrogen and progesterone receptors in the vulva and vaginaBr J Obstet Gynaecol 1998 105(2):216-22. [Google Scholar]