Aneurysmal Bone Cyst of C2 Cervical Spine Presenting as an Asymptomatic Posterior Neck Swelling
Pradosh Kumar Sarangi1, Jayashree Mohanty2, Sasmita Parida3, Basanta Manjari Swain4, Sunil Kumar5
1 Resident, Department of Radiodiagnosis, Shri Ramachandra Bhanj Medical College and Hospital, Cuttack, Odisha, India.
2 Professor and Head, Department of Radiodiagnosis, Shri Ramachandra Bhanj Medical College and Hospital, Cuttack, Odisha, India.
3 Associate Professor, Department of Radiodiagnosis, Shri Ramachandra Bhanj Medical College and Hospital, Cuttack, Odisha, India.
4 Associate Professor, Department of Radiodiagnosis, Shri Ramachandra Bhanj Medical College and Hospital, Cuttack, Odisha, India.
5 Resident, Department of Oral pathology and Microbiology, Shri Ramachandra Bhanj Medical College and Hospital, Cuttack, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pradosh Kumar Sarangi, Resident, Department of Radiodiagnosis, Shri Ramachandra Bhanj Medical College and Hospital, Cuttack-753007, Odisha, India.
E-mail: lipu90sarangi@gmail.com
Aneurysmal Bone Cysts (ABC) are benign tumour-like expansile lytic lesions commonly affecting metaphysis of long bones. They are relatively rare in vertebral column accounting for about 12 to 30% of all ABC cases, predominantly involving posterior elements. ABC of cervical spine account for only 2% cases. They commonly present as back pain, palpable mass, spinal deformity, rarely pathological fracture and neurological deficit (paraplegia, cord compression, and cauda equina syndrome). Surgical treatment of ABC of cervical spine in paediatric patients is challenging because of proximity of lesions to neurovascular structures and the potential remaining growth of the spine. Here, we report a case of ABC of C2 vertebra with isolated posterior arch involvement who presented with a palpable posterior nuchal swelling and skin discoloration without any neurological deficit or difficulty in neck movement. Biopsy led to the definite diagnosis of ABC.
Back pain, Fluid-fluid level, Palpable mass, Tumour
Case Report
An eight-year-old girl presented with a history of palpable swelling at the nape of neck for two years. There was no history of trauma to that region. The lesion was slowly growing over a period of two years to the present size of 4×2 cm. Her general examination was unremarkable. On local examination, she had a 4×2 cm bony, immobile swelling in the midline posterior neck without local warmth or tenderness. There was discolouration of overlying skin [Table/Fig-1]. There was no restriction of neck movements or any neurological deficits. No conclusive clinical diagnosis could be made at this point except bony nature of the lesion.
Swelling at the posterior neck region, overlying skin appears discoloured.

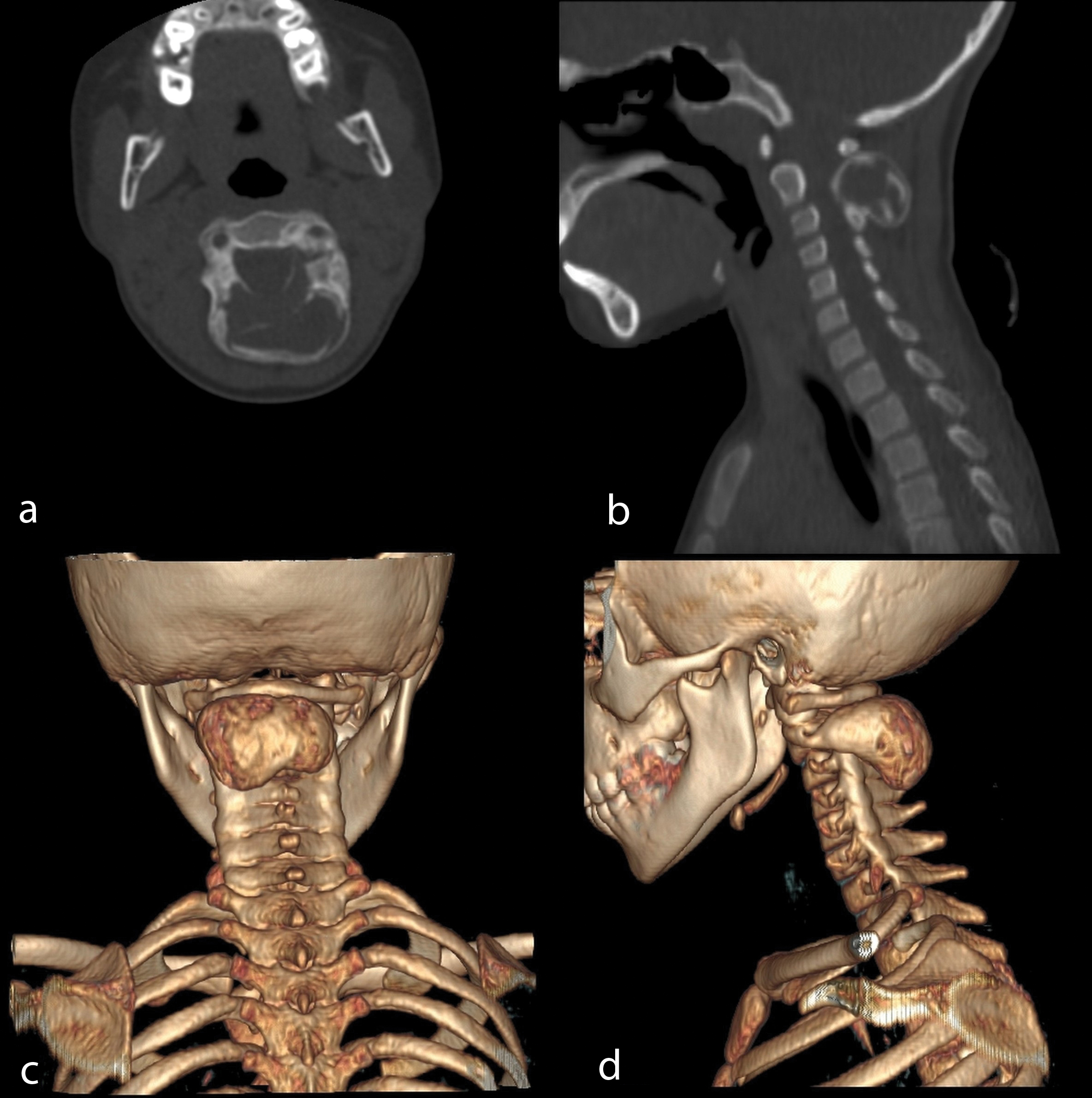
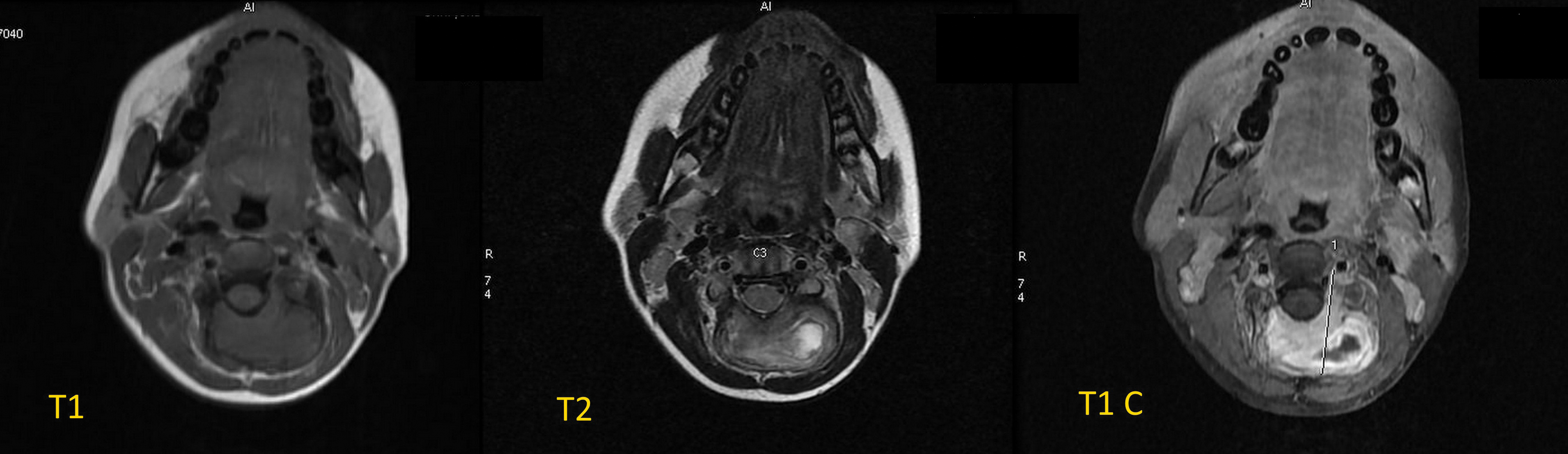
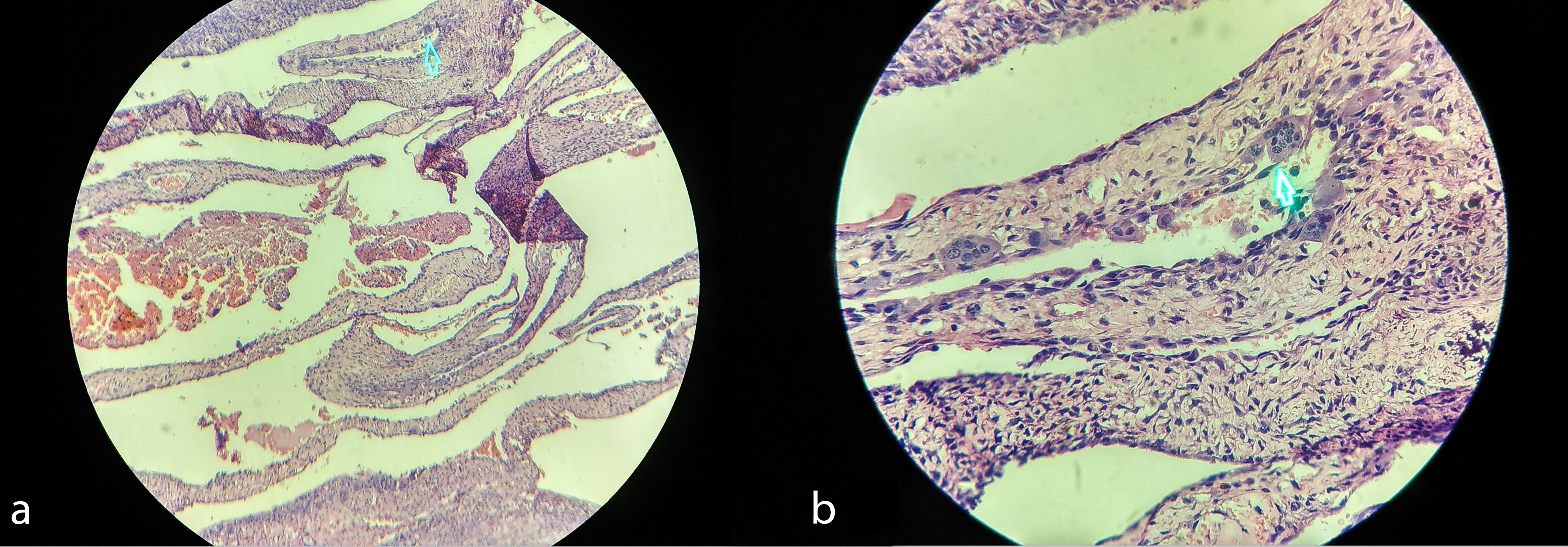
Lateral radiograph of cervical spine demonstrated a sharply defined, expansile osteolytic lesions (characteristic ballooning appearance) with thin sclerotic margins involving posterior element of C2 vertebra without any matrix mineralisation [Table/Fig-2]. Computed tomography (CT) was done to know the extent of lesion [Table/Fig-3a,b]. It showed a multiloculated expansile lytic lesion of size (4×2×2.5) cm involving C2 posterior element without any soft tissue component or fluid-fluid level. There was no evidence of spinal canal narrowing. Three Dimensional CT with Volume Rendering Technique (VRT) nicely depicted the origin of lesion from C2 posterior element. The lesion extended caudally up to C4 spinous process [Table/Fig-3c,d]. Magnetic Resonance Imaging (MRI) of the cervical spine revealed T1 isointense and T2 intermediate signal intensity lobulated expansile mass lesion with T2 hyperintense components involving spinous process and lamina of C2 vertebra. There was no spinal cord involvement. Normal flow void noted in bilateral vertebral arteries. On Gadolinium contrast study, the lesion showed heterogenous enhancing components. However, no fluid-fluid level was noted in T2W image [Table/Fig-4]. Based on patient age, radiograph, CT and MRI images, a presumptive differential diagnosis of ABC, giant cell tumour, and osteoblastoma was made. Patient was advised for complete surgical removal of the tumour by en bloc excision through posterior approach and surgical stabilisation. However, her parents were not willing for the surgery and surgery was deferred. Hence, it was decided to undertake percutaneous CT-guided needle biopsy targeting cyst wall and internal septa for definite tissue diagnosis. Microscopy revealed multiple sinusoidal spaces without endothelial lining engorged with red blood cells suggestive of ABC. Scattered areas of multinucleated osteoclast like giant cells, foci of calcification and ossification in the background of proliferating fibrocellular stroma were also noted [Table/Fig-5]. She was advised for regular follow up in neurosurgery OPD and report urgently in case of imminent neurological compromise. The patient is in good health after one year of follow up.
X-ray neck lateral view showing a sharply defined multiloculated expansile lesion with narrow zone of transition involving posterior element of C2 (axis vertebra).

Non-contrast CT axial; a) and sagittal; b) bone window showing a multiloculated expansile lytic lesion involving C2 posterior element without any soft tissue component without any evidence of spinal canal narrowing. 3D CT with volume rendering technique; c,d) nicely depicting the origin of lesion from C2 posterior element. The lesion extends caudally up to C4 spinous process.
Axial MRI showing T1 isointense and T2 intermediate signal intensity lobulated expansile mass lesion with T2 hyperintense components involving spinous process and lamina of C2 vertebra. On contrast study (T1 C), the lesion shows enhancing components. However, No fluid-fluid level was noted.
Photomicrograph of low power (10X) and high power (40X), field showing multiple sinusoidal spaces surrounded by multinucleated giant cells (arrow) in the background of proliferating fibrocellular stroma.
Discussion
Aneurysmal bone cysts are benign expansile tumour-like bone lesions of uncertain aetiology, characterised by numerous blood-filled channels. They usually involve metaphysis long bones, but about 12-30% of cases involve the spine with lumbar spine the most frequent site. Within the spine, lesions affect the posterior elements, extending anteriorly to include the pedicles, the vertebral bodies, and the paraspinal areas [1,2]. ABC of cervical spine accounts for only 2% cases [3]. These are locally aggressive tumours and extensive bony destruction can result in pathological fractures of the vertebrae and neurological complications. ABC was first reported in 1893 by Van Arsdale who termed it as ossifying hematoma [4]. Later in 1942, Jaffe and Lichtenstein coined the term “aneurysmal bone cysts” defining it as a lesion having a “blown-out” radiographic appearance analogous to a saccular aneurysm [5,6].
Aneurysmal bone cysts are commonly seen in children and adolescents with 60% occurring in the patients less than 20 years of age [6]. The 70% cases of ABC are primary without any underlying lesions. Secondary ABC is associated with giant cell tumour, chondroblastoma, osteoblastoma, telangiectatic osteosarcoma [7,8]. The rare solid variant of ABC only differs from classic ABC in that cavernous channels and spaces are absent [8].
Lim JB et al., has shown that most common symptom in ABC of spine is gradually increasing pain in back. Other symptoms are palpable spinal mass, spinal deformity (kyphosis or scoliosis), and neurological deficits [1]. Our case is interesting in the sense that patient had swelling for two years without any symptoms.
The radiological differential diagnosis of an expansile lytic lesion involving the posterior elements of vertebrae, such as spinous processes in children includes simple bone cyst, ABC, osteoblastoma [9,10] and Giant Cell Tumour (GCT) [11]. Radiographs demonstrate sharply defined, expansile osteolytic lesions, with thin sclerotic margins without cortical defect or a soft tissue mass. When there is cortical loss, or extraosseous soft tissue extension, the differential diagnosis of giant cell tumor, aggressive osteoblastoma, and low-grade chondrosarcoma should be considered [7]. CT and MRI can show fluid-fluid levels caused by haemorrhage and internal septations helping in diagnosis of ABC. Though, Fluid-fluid levels are highly suggestive of ABC, these are not specific for ABC [12]. So, definitive diagnosis requires biopsy for histologic confirmation. Fluid-fluid levels can be seen in GCT, chondroblastoma, simple bone cysts and telangiectatic osteosarcomas. These are best seen in T2W MRI sequence. On MRI, ABC appears as a multilobulated lytic lesion with multiple internal septations and fluid levels. The cysts are of a variable signal representing areas of blood of variable age with a surrounding rim of low T1 and T2 signal [10]. Presence of enhancing solid components suggest secondary ABC.
The literature on aneurysmal bone cysts in the cervical spine is limited to isolated case reports, especially in paediatric age groups [2,3,7,13-16]. To our knowledge, there are only handful of case reports on aneurysmal bone cyst of C2 spine [7,14-16]. A largest paediatric case series was published by Novais EN et al., in 2011 who retrospectively reviewed seven children with ABC of cervical spine with mean age of 11.9 years at the time of diagnosis [17]. All of them were symptomatic with presence of neck pain and four of them had neurological symptoms in terms of upper extremity paraesthesia and weakness. One case (eight year, female) showed involvement of posterior element and vertebral body of C2 and laminae of C3 spine with large soft tissue component causing cord compression. The patient presented with neck pain and restricted range motion. She underwent immobilization in halo vest followed by intralesional excision and instrumentation from occiput to C5 with extradural decompression. Our case is unique because of rarity of location in cervical spine and isolated posterior arch involvement without any symptoms.
Conclusion
Aneurysmal bone cysts of cervical spine is rare. Though, most common presentation is pain, it can however remain completely asymptomatic, especially for lesions with isolated involvement of posterior arch. It can expand to the spinal canal resulting in pathological fractures and neurological deficits due to progressive growth. So, early detection is required to prevent such poor outcome. ABC should be considered in the differential diagnosis of expansile lytic lesions of the spine in young individuals.
[1]. Lim JB, Sharma H, Reid R, Reece AT, Aneurysmal bone cysts of the vertebraeJ Orthop Surg 2012 20(2):201-04. [Google Scholar]
[2]. Mishra SS, Panigrahi S, Das D, Giant aneurysmal bone cyst of cervical spine: Surgical management and circumferential spinal fusion in a 13-year-old girlJ Pediatr Neurosci 2014 9(2):196-99. [Google Scholar]
[3]. Lee JM, Rhim SC, Lee DH, Song JS, Aneurysmal Bone Cysts of the Cervical SpineThe Nerve 2016 2(1):10-12. [Google Scholar]
[4]. Van Arsdale WW, Ossifying haematomaAnn Surg 1893 18(1):817 [Google Scholar]
[5]. Jaffe H, Lichtenstein L, Solitary unicameral bone cyst with emphasis on the roentgen picture, the pathologic appearance and the pathogenesisArch Surg 1942 44(6):1004-25. [Google Scholar]
[6]. Saccomanni B, Aneurysmal bone cyst of spine: A review of literatureArch Orthop Trauma Surg 2008 128(10):1145-47. [Google Scholar]
[7]. Bivins E, Alidina JA, Bancroft LW, Aneurysmal Bone Cyst Involving the C2 VertebraOrthopedics 2015 38(2):78-143. [Google Scholar]
[8]. Boriani S, De Iure F, Campanacci L, Gasbarrini A, Bandiera S, Biagini R, Aneurysmal bone cyst of the mobile spine: Report on 41 casesSpine (Phila Pa 1976) 2001 26(1):27-35. [Google Scholar]
[9]. Lee CC, Wei JD, How SW, Simple bone cyst in cervical vertebral spinous process and laminae: report of a caseJ Formos Med Assoc 2000 99(1):54-58. [Google Scholar]
[10]. Zileli M, Isik HS, Ogut FE, Cagli S, Calli C, Aneurysmal bone cysts of the spineEuropean Spine Journal 2013 22(3):593-601. [Google Scholar]
[11]. Sarangi PK, Pattanayak D, Hui P, Singh M, Mohanty J, Giant Cell Tumor of the Thoracic Spine-A Case ReportInt J Health Sci Res 2016 6(8):415-19. [Google Scholar]
[12]. Liu JK, Brockmeyer DL, Dailey AT, Schmidt MH, Surgical management of aneurysmal bone cysts of the spineNeurosurg Focus 2003 15(5):E4 [Google Scholar]
[13]. Khalil IM, Alaraj AM, Otrock ZK, Chamoun RB, Sabbagh AS, Skaf GS, Aneurysmal bone cyst of the cervical spine in a child: case report and review of the surgical roleSurgical neurology 2006 65(3):298-303. [Google Scholar]
[14]. Levin DA, Hensinger RN, Graziano GP, Aneurysmal bone cyst of the second cervical vertebrae causing multilevel upper cervical instabilityJ Spinal Disord Tech 2006 19(1):73-75. [Google Scholar]
[15]. Naveen MA, Naik V, Keshav GC, Kumar SAS, Pai SB, Aneurysmal Bone Cyst of C2, C3 Cervical Spine: a Rare Case Report and Review of LiteratureJ Spinal Surg 2015 2(2):52-54. [Google Scholar]
[16]. Pennekamp W, Peters S, Schinkel C, Kuhnen C, Nicolas V, Muhr G, Aneurysmal bone cyst of the cervical spine (2008:7b)Eur Radiol 2008 18(10):2356-60. [Google Scholar]
[17]. Novais EN, Rose PS, Yaszemski MJ, Sim FH, Aneurysmal bone cyst of the cervical spine in childrenThe Journal of Bone and Joint Surgery 2011 93(16):1534-43. [Google Scholar]