Case Series
Case 1
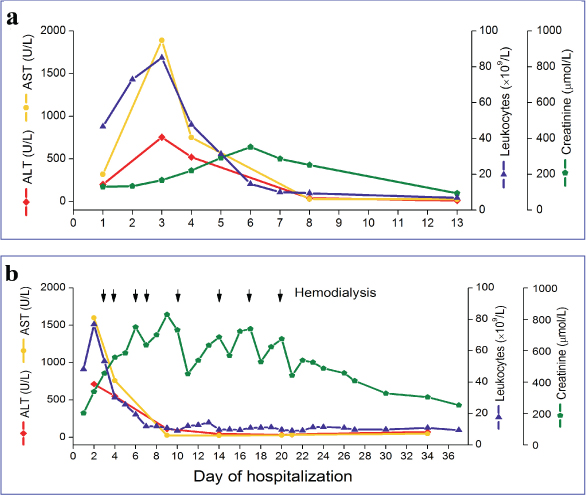
A 32-year-old male, farmer, was admitted with severe leukocytosis and profound thrombocytopenia but with no obvious signs of renal involvement, in whom a haematologic disorder was initially suspected. He reported a four day history of fever up to 39°C when he was admitted in November 2013. On admission, he had a leukocyte count of 46.61×109/L, a platelet count of 12×109/L, and a normal serum creatinine level [Table/Fig-1a]. The initial symptoms, such as high fever, headache, backache, conjunctival congestion, and petechiae, were consistent with those reported in hantavirus-infected patients [1], but serologic tests for hantavirus were negative. Since, a malignant haematologic disease was highly suspected, he underwent bone marrow aspiration but no specific finding was observed. His leukocyte count rapidly increased to 85.13×109/L (neutrophils, 93%) by day three of hospitalisation, with a daily increase of roughly 20×109/L [Table/Fig-1a]. The patient unexpectedly developed liver dysfunction on day three with an Alanine Aminotransferase (ALT) level of 755 U/L, Aspartate Aminotransferase (AST) level of 1890 U/L, albumin level of 26 gm/L. Serologic tests for hepatitis A, B and C were negative, while IgM antibodies to Hantaan virus (HTNV) were positive on day five when tested again. However, his serum creatinine, slowly increased from day three and peaked at day six with a level of 352.6 μmol/L, followed by full spontaneous recovery of kidney function. Upon supportive therapy, the counts of leukocytes and platelets, as well as the levels of liver enzymes, gradually recovered to baseline by day eight. The patient recovered and was discharged on day 13 of hospitalisation.
Haematological and biochemical changes over time in case 1 and case 2. On the day of haemodialysis, only data prior to the haemodialysis treatment were included.
Case 2
A 42-year-old male, farmer with severe shock and a five day history of fever, was found to have a leukocyte count of 48.18×109/L, a platelet count of 23×109/L, and serum creatinine level of 201.9 μmol/L [Table/Fig-1b]. His leukocyte counts rapidly increased to 76.81×109/L (neutrophils, 91%) within two days after admission. Concurrently, the patient developed proteinuria, haematuria, oliguria and AKI, the typical signs of renal involvement [2], together with acute liver dysfunction (urine output of 270 mL/day, serum creatinine level of 338.7 μmol/L, ALT level of 713 U/L, AST level of 1600 U/L, and albumin level of 27 gm/L). Upon supportive therapy, his leukocyte and platelet counts, as well as liver enzyme levels, decreased swiftly and returned to normal eventually within roughly two weeks. Despite eight sessions of haemodialysis, the levels of serum creatinine, continued to rise progressively to 829.7 μmol/L by day nine of hospitalisation. The patient was discharged on day 37 after admission, with a serum creatinine level of 252.7 μmol/L; and all other laboratory results returned to baseline. HTNV infection was confirmed serologically on day 11.
Case 3
A 50-year-old male, farmer with a seven-day history of fever and upper respiratory symptoms. He was in severe shock with undetectable blood pressure and required immediate tracheotomy and mechanical ventilation. Laboratory studies revealed the following values: leukocytes-32.51×109/L; platelets-6×109/L; serum creatinine-141.2 μmol/L; ALT-30 U/L; AST-100 U/L; albumin-15 gm/L. Urinalysis revealed proteinuria, but no haematuria. Despite fluid resuscitation, and vasopressor and antiviral therapy, organ functions and laboratory results further deteriorated. Following the consistent increase of leukocyte counts from 32.51×109/L to 74.69×109/L within two days, the levels of ALT and AST increased from 30 U/L and 100 U/L to 308 U/L and 1435 U/L, respectively. On the third day of hospitalisation, he continued to have high fever and severe shock, and developed oliguria. His consciousness deteriorated, and continuous renal replacement therapy was started. His leukocyte counts rapidly reduced to 23.66×109/L, and his serum creatinine remained no more than 269.1 μmol/L. However, he died of severe shock at the end of the day. HTNV infection was confirmed serologically on day two of hospitalisation.
Discussion
Haemorrhagic fever with renal syndrome caused by hantaviruses including HTNV, Seoul, Puumala and Dobrava-Belgrade virus, is characterised by fever, haemorrhage and AKI. However, most of the symptoms and signs of HFRS, such as oliguria, anuria and AKI, do not appear until the later stages of illness. Although, leukocytosis (leukocytes >10×109/L), along with thrombocytopenia, is an early, common laboratory finding in patients with hantavirus infection [3], leukemoid reaction was seldom described in HFRS as well as in hantavirus pulmonary syndrome [4].
Acute hepatitis is common in patients with dengue haemorrhagic fever, and a level of AST or ALT ≥1000 U/L was used as a criterion for severe dengue [5,6]. Unlikely, liver involvement is much rare in hantavirus infections, which has been described in several cases caused by Puumala and Dobrava-Belgrade virus infection [7,8].
Leukemoid reaction associated with hepatitis has only been reported in alcoholic hepatitis with high mortality [9,10]. Here, we reported a tetrad of fever, leukemoid reaction, profound thrombocytopenia, and acute liver dysfunction as an early presentation of HFRS in three patients with acute HTNV infection who had mild to severe AKI subsequently. There were more HFRS cases reported from the region during the same time. The physicians suspected the HTNV infection because of the early presentations and the fact that the patients lived in a region highly endemic for hantavirus and was admitted during the epidemic season of HFRS. However, the infection was confirmed subsequently, there is no specific vaccine or therapy for hantavirus so far.
Extreme leukocytosis combined with thrombocytopenia and fever often points to the consideration of haematologic disorder. However, besides leukaemia, a leukemoid reaction (leukocytes >50×109/L), which describes extremely elevated blood leukocyte counts secondary to infection, inflammation or neoplasm [11,12], should be considered in patients with an extreme leukocytosis [13].
The three cases admitted to hospital at a median of five days (range, 4-7 days) after onset of fever. A leukemoid reaction was presented on the first or second day of hospital admission, and lasted for a median of two days (range, two to three days). In addition to leukemoid reaction, all patients had profound thrombocytopenia (nadir platelet count <20×109/L), and severe acute hepatitis defined by ALT and/or AST >400 U/L (ten times the upper limit of normality). HTNV infection was confirmed serologically in all patients, and serologic tests for hepatitis B and C were negative. Among these patients, all had severe shock with undetectable blood pressure, one underwent tracheotomy and mechanical ventilation, two had severe AKI defined as stage three AKI by receipt of acute dialysis or increased serum creatinine ≥354 μmol/L according to AKI Network, two patients underwent continuous renal replacement therapy and/or intermittent haemodialysis, and one died early at the hypotensive stage.
Thrombocytopenia, fever, and impaired renal function are characteristic features of HFRS. However, clinical presentations and blood cell counts may point to other disorders, such as a haematologic disease, particularly when the impairment of renal function is not obvious [14]. In Case 1, the early presentations, such as extreme leukocytosis, profound thrombocytopenia, the serologic negativity for hantavirus, normal serum creatinine levels, as well as the absence of oliguria, proteinuria or haematuria and the typical signs of renal involvement [2], initially resulted in the diagnosis of HFRS being overlooked, although the patient lived in a region highly endemic for hantavirus and was admitted during the epidemic season of HFRS. Additional tests, such as bone marrow aspiration, were therefore performed. In Case 2 and 3, because typical symptoms of renal involvement occurred early, despite profound thrombocytopenia and extreme leukocytosis, further invasive tests were not performed. Our findings emphasize the need for increasing awareness of hantavirus testing in patients with fever and haematological manifestations, particularly in areas endemic for the infection.
In the present report, we described clinical evidence for HTNV infection leading to a co-occurrence of leukemoid reaction, profound thrombocytopenia, and acute liver dysfunction, along with high fever and severe shock, which were all recovered on discharge except in Case 3 who died at the early hypotensive stage. A similar scenario was also found in a case of Dobrava-Belgrade hantavirus infection complicated by pan hypopituitarism who had severe leukocytosis, profound thrombocytopenia, and acute liver dysfunction in the early stages [8].
Conclusion
The three cases here showed that leukemoid reaction may occur in parallel to profound thrombocytopenia and liver dysfunction in the early stage of HFRS. When considering a haematologic disorder in patients with fever, thrombocytopenia and leukocytosis, consider hantavirus testing to rule out an infectious process.
[1]. Du H, Wang PZ, Li J, Bai L, Li H, Yu HT, Clinical characteristics and outcomes in critical patients with haemorrhagic fever with renal syndromeBMC Infect Dis 2014 14:191 [Google Scholar]
[2]. Vaheri A, Strandin T, Hepojoki J, Sironen T, Henttonen H, Makela S, Uncovering the mysteries of hantavirus infectionsNat Rev Microbiol 2013 11(8):539-50. [Google Scholar]
[3]. Wang M, Wang J, Wang T, Li J, Hui L, Ha X, Thrombocytopenia as a predictor of severe acute kidney injury in patients with Hantaan virus infectionsPLoS One 2013 8(1):e53236 [Google Scholar]
[4]. Duchin JS, Koster FT, Peters CJ, Simpson GL, Tempest B, Zaki SR, Hantavirus pulmonary syndrome: a clinical description of 17 patients with a newly recognized disease. The Hantavirus Study GroupN Engl J Med 1994 330(14):949-55. [Google Scholar]
[5]. Parkash O, Almas A, Jafri SM, Hamid S, Akhtar J, Alishah H, Severity of acute hepatitis and its outcome in patients with dengue fever in a tertiary care hospital Karachi, Pakistan (South Asia)BMC Gastroenterol 2010 10:43 [Google Scholar]
[6]. Lee LK, Gan VC, Lee VJ, Tan AS, Leo YS, Lye DC, Clinical relevance and discriminatory value of elevated liver aminotransferase levels for dengue severityPLoS Negl Trop Dis 2012 6(6):e1676 [Google Scholar]
[7]. Eckerle I, Jakob E, Hofmann J, Schmidt-Bacher A, Ettinger J, Schnitzler P, Atypical severe Puumala hantavirus infection and virus sequence analysis of the patient and regional reservoir hostZoonoses Public Health 2012 59(Suppl 2):110-15. [Google Scholar]
[8]. Sarigüzel N, Hofmann J, Canpolat AT, Türk A, Ettinger J, Atmaca D, Dobrava hantavirus infection complicated by panhypopituitarism, Istanbul, Turkey, 2010Emerg Infect Dis 2012 18(7):1180-83. [Google Scholar]
[9]. Morales AM, Hashimoto LA, Mokhtee D, Alcoholic hepatitis with leukemoid reaction after surgeryJ Gastrointest Surg 2006 10(1):83-85. [Google Scholar]
[10]. Arguelles-Grande C, Leon F, Matilla J, Dominguez J, Montero J, Steroidal management and serum cytokine profile of a case of alcoholic hepatitis with leukemoid reactionScand J Gastroenterol 2002 37(9):1111-13. [Google Scholar]
[11]. Sakka V, Tsiodras S, Giamarellos-Bourboulis EJ, Giamarellou H, An update on the etiology and diagnostic evaluation of a leukemoid reactionEur J Intern Med 2006 17(6):394-98. [Google Scholar]
[12]. Granger JM, Kontoyiannis DP, Etiology and outcome of extreme leukocytosis in 758 nonhaematologic cancer patients: a retrospective, single-institution studyCancer 2009 115(17):3919-23. [Google Scholar]
[13]. Halkes CJ, Dijstelbloem HM, Eelkman Rooda SJ, Kramer MH, Extreme leucocytosis: not always leukaemiaNeth J Med 2007 65(7):248-51. [Google Scholar]
[14]. Denecke B, Bigalke B, Haap M, Overkamp D, Lehnert H, Haas CS, Hantavirus infection: a neglected diagnosis in thrombocytopenia and fever?Mayo Clin Proc 2010 85(11):1016-20. [Google Scholar]