Manifestation of Primary Syphilis in Two Extragenital Regions
João Paulo De Carli1, Silas Antonio Juvencio De Freitas Filho2, Luiz Renato Paranhos3, Gisele Rovani4, Mateus Ericson Flores5
1 Professor, Department of Stomatology and Prosthodontics, University of Passo Fundo, Passo Fundo, Rio Grande Do Sul, Brazil.
2 PhD Student, Department of Surgery, Stomatology, Pathology and Radiology, University of São Paulo, Bauru, São Paulo, Brazil.
3 Professor, Department of Dentistry, Federal University of Sergipe, Lagarto, Sergipe, Brazil.
4 Professor, Department of Stomatology and Prosthodontics, University of Passo Fundo, Passo Fundo, Rio Grande Do Sul, Brazil.
5 Professor, Department of Stomatology and Prosthodontics, University of Passo Fundo, Passo Fundo, Rio Grande Do Sul, Brazils.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Luiz Renato Paranhos, Professor, Department of Dentistry, Federal University of Sergipe, Avenida Governador Marcelo Déda, 13, Centro, 49400-000 Lagarto, Sergipe, Brazil.
E-mail: paranhos.lrp@gmail.com
Biopsy, Diagnosis, Face, Infection
A 52-year-old male patient, heterosexual, was referred to the Department of Stomatology at Passo Fundo University, Brazil, complaining of an ulcer in the upper lip.
According to the patient, the lesion appeared spontaneously in the upper lip and evolved during 14 days. Simultaneously, a second ulcer on the nose also appeared. No history of facial trauma was reported. The patient stated that he worked as a farmer, constantly exposed to sunlight. Clinically, both ulcers presented with indurated borders. They measured 1.2 cm (center of the upper lip) and 5 mm (tip of the nose) [Table/Fig-1a]. In addition, the surrounding mucosa of the lip ulcer was normal, but the skin around the nose ulcer was erythematous. There was no increase in local temperature and the patient reported no pain on palpation. Intraorally, no lesions were observed. Cervical lymph nodes were not altered. The clinical hypothesis included actinic cheilitis, squamous cell carcinoma and bacterial or fungal infections.
a) Ulcer at the apex of the nose with surrounding erythematous skin and in the upper lip without changes around; b) Incisional biopsy of the upper lip.
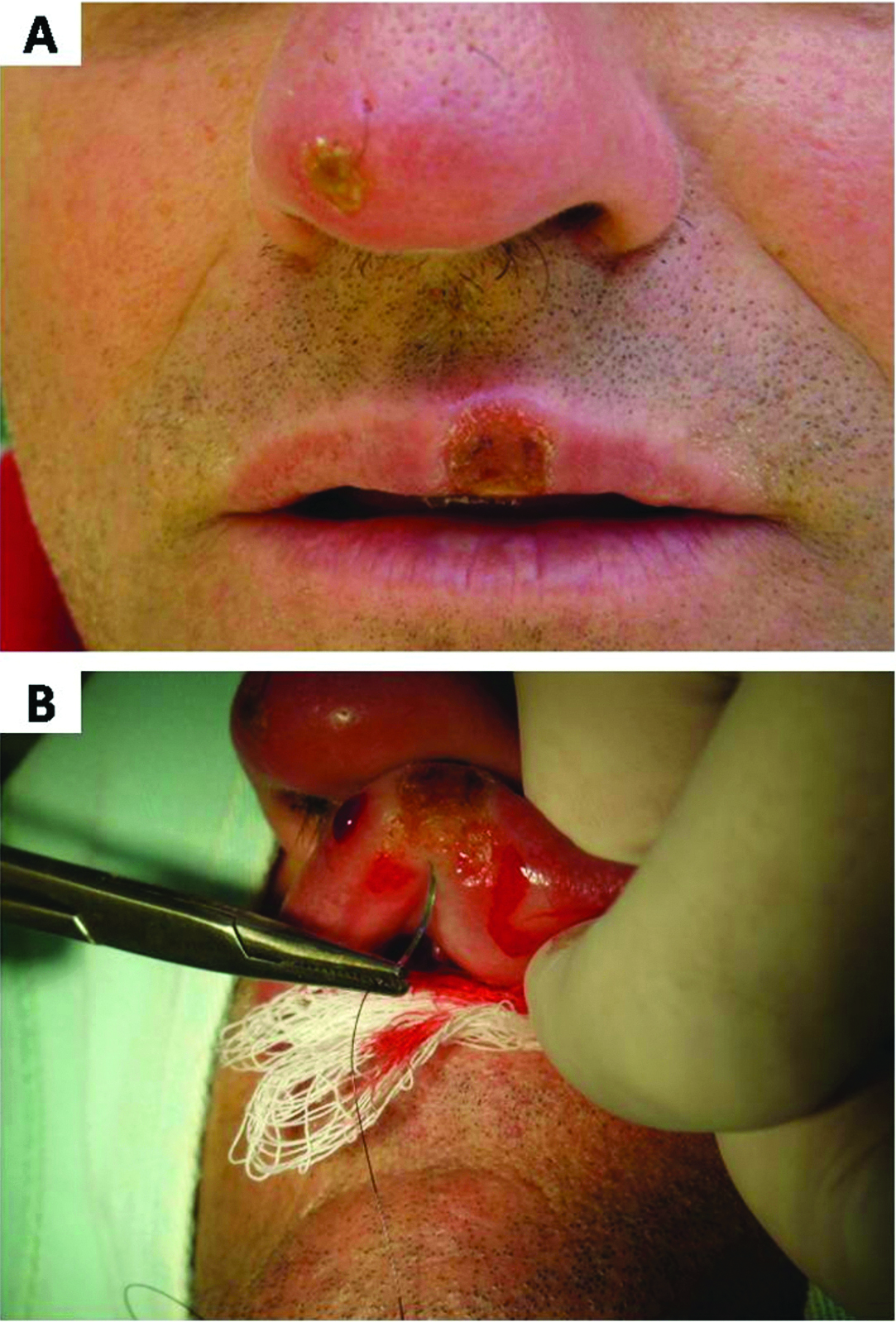
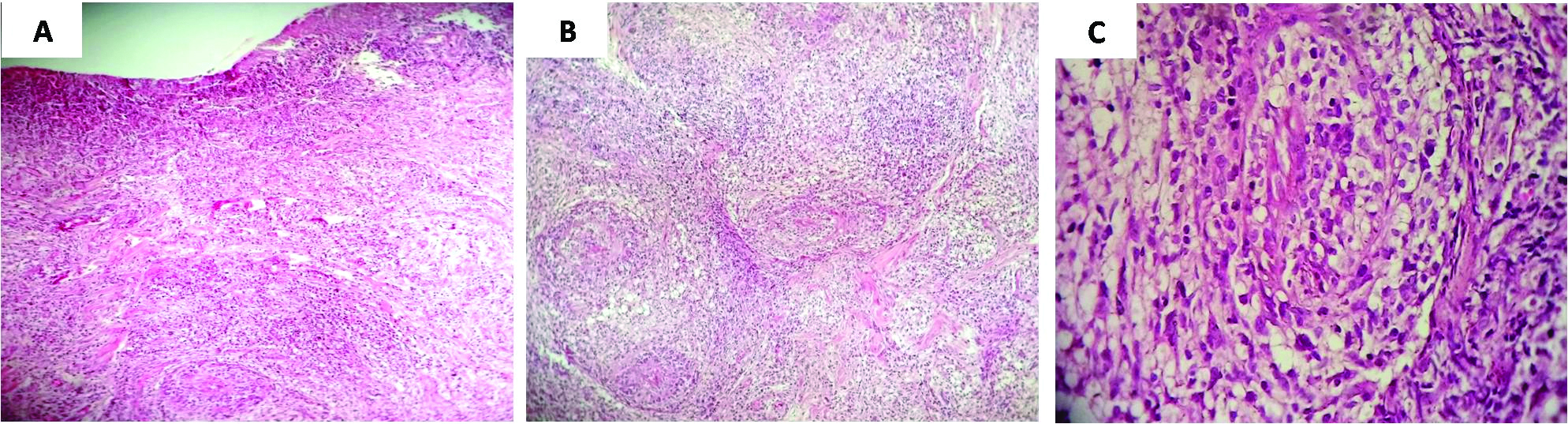
Incisional biopsy was performed [Table/Fig-1b]. The histopathological analysis revealed a non-specific ulceration covered by serofibrinous exudates, intense subjacent mononuclear inflammatory infiltrate and granulomatous formation [Table/Fig-2]. Venereal Disease Research Laboratory (VDRL) test was requested and resulted positive for syphilis with a titer of 1:64. The patient was treated with a single dose of Benzathine penicilin G (2.4 million units) administered intramuscularly. Within a follow up of 18 months, the titer decreased to 1:4 and clinically the appearance of the lip and nose were normal after treatment [Table/Fig-3].
Histopathological analysis; a) Non-specific ulceration covered by serofibrinous exudates, intense subjacent mononuclear inflammatory infiltrate and granulomatous formation (100x, H&E staining); b,c) Chronic granulomatous inflammation (B: 100x, C: 400x, H&E staining).
The appearance of the upper lip and nose were normal after treatment of 18 months.

Syphilis is a complex infectious disease cause by the Treponema pallidum [1]. Over the last decade, this disease became highly prevalent worldwide, especially in North America, Europe and China [2]. Diagnosing syphilis is a challenging task when oral and multiple extragenital lesions are detected [2]. Skin and mucosal lesions develop after loss of integrity of the epithelium caused by abrasions due to oral sex [3]. The diagnostic hypothesis considered in this case were based on the clinical aspects of the lesions. Knowing the clinical manifestation of syphilis is essential to guarantee optimal diagnosis of dermatologic and oral lesions. Differential diagnosis for perioral lesions must include primary tuberculosis, non-tuberculous mycobacterial infection, cutaneous leishmaniasis, cat-scratch disease and malignant neoplasm [4]. Clinically, three stages may be observed in patients affected with syphilis [1]. Specifically in the first, a single asymptomatic chancre is usually observed within 10 to 90 days after the infection. At this stage, genital lesions are more common than oral and perioral lesions [2]. The biopsy also plays an important role towards the diagnosis [2]. In the present case, the diagnostic hypothesis of syphilis was considered after the histopathological examination. Despite the fact of being non-specific [5], the microscopic aspect of primary syphilis shows ulceration with inflammatory mononuclear cell infiltrate (macrophages, lymphocytes and plasmocytes), as well the proliferation of endothelial cells [6]. Immunohistochemical staining show spirochetes distributed in the epithelial and connective tissues [5]. The combination of clinical aspects and microscopic findings justified the serological test for syphilis [5].
Nontreponemal and treponemal serological tests, such as VDRL and the Fluorescent Treponemal Antibody Absorption (FTA-ABS) respectively, may be used to investigate syphilis [1]. Despite the scarce information collected during the anamnesis, the patient was diagnosed through the combination of physical exam and serological test. It is important to note that other sexual diseases must be investigated after the confirmation of syphilis [3,6].
Anamnesis and physical examination have a significant part in the diagnosis of sexual diseases, including syphilis. Professionals of the Health Sciences potentially involved with these cases must be able for early diagnosing and proper managing extragenital lesions. For that reason, syphilis should be considered as a differential diagnosis for multiple lesions on skin and mucosa.
[1]. Stamm LV, Syphilis: Re-emergence of an old foeMicrob Cell 2016 3(9):363-70. [Google Scholar]
[2]. Watts PJ, Greenberg HL, Khachemoune A, Unusual primary syphilis: Presentation of a likely case with a review of the stages of acquired syphilis, its differential diagnoses, management, and current recommendationsInt J Dermatol 2016 55(7):714-28. [Google Scholar]
[3]. Fukuda H, Takahashi M, Kato K, Oharaseki T, Mukai H, Multiple primary syphilis on the lip, nipple-areola and penis: An immunohistochemical examination of Treponema pallidum localization using an anti-T pallidum antibodyJ Dermatol 2015 42(5):515-17. [Google Scholar]
[4]. Menni S, Acquired primary syphilis on a child’s lipActa Derm Venereol 2007 87(3):284 [Google Scholar]
[5]. Siqueira CS, Saturno JL, de Sousa SC, da Silveira FR, Diagnostic approaches in unsuspected oral lesions of syphilisInt J Oral Maxillofac Surg 2014 43(12):1436-40. [Google Scholar]
[6]. Demir FT, Salaeva K, Altunay IK, Yalcın O, An extraordinary case of syphilis presenting with a labial ulcerSaudi Med J 2016 37(11):1261-64. [Google Scholar]