Management of Chronic Blink Related Microtrauma in Stevens-Johnson Syndrome with Oral Mucous Membrane Graft Transplantation: A Novel Approach
Rahul Nandkishor Laturiya1, Syed Mohiuddin Ahmed2, Priyanka Mallikarjun Tapsale3, Vishnukant Vankatrao Ghonsikar4, Ahtesham Qurishi Ahmed5
1 Professor, Department of Oral and Maxillofacial Surgery, Maharashtra Institute of Dental Science and Research Center, Latur, Maharashtra, India.
2 Professor and Head, Department of Oral and Maxillofacial Surgery, Maharashtra Institute of Dental Science and Research Center, Latur, Maharashtra, India.
3 Postgraduate Student, Department of Oral and Maxillofacial Surgery, Maharashtra Institute of Dental Science and Research Center, Latur, Maharashtra, India.
4 Director, Department of Ophthalmology, Shankar Natralay, Nanded, Maharashtra, India.
5 Reader, Department of Oral and Maxillofacial Surgery, Maharashtra Institute of Dental Science and Research Center, Latur, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Priyanka Mallikarjun Tapsale, Postgraduate Student, Department of Oral and Maxillofacial Surgery, Room No-5, M.I.D.S.R. Dental College and Hospital, Ambejogai Road, Vishwanathpuram, Latur-413512, Maharashtra, India.
E-mail: dr.priyanka8041@gmail.com
A 26-year-old male was referred with sequel of Stevens-Johnson Syndrome (SJS) in form of bilateral severe keratinisation of lid margin and Symbhlepharon involving in particular forniceal region. At the time of presentation his visual acuity was 20/120. Indirect ophthalmoscopic examination revealed normal optic nerve head with attached retina. Superficial dissection was done between palpebral and bulbar conjunctiva so as to release symblepharon and further ocular surface reconstruction was carried out with labial Mucous Membrane Graft [MMG]. His best corrected final visual acuity was 20/40 with well accepted graft indicating that this technique definitely improves visual acuity and alleviates patient discomfort by improving ocular surface milieu and hence, possibly further avoids deterioration of ocular surface in SJS.
Cicatricial entropion, Limbal stem cell, Ocular surface reconstruction, Symbhlepharon
Case Report
A 26-year-old male construction worker came with history of bilateral ocular dryness, redness and irritation since four months. He had history of fever with chills and sore throat two months back for which he was treated by a general practitioner with amoxicillin and combiflam following after which he developed reddish spots all over body which rapidly converted in erythematous papules on trunk and limbs with mucosal involvement, predominantly bilateral ophthalmic conjunctival involvement. He was diagnosed by a dermatologist as a case of SJS for which he was hospitalised in Intensive Care Unit (ICU) and discharged after 15 days of hospital stay. His skin lesions healed completely over a period of six weeks but the dryness and redness in eyes persisted for which he visited ophthalmology department at M.I.D.S.R. Dental College and Hospital, Latur [Table/Fig-1].
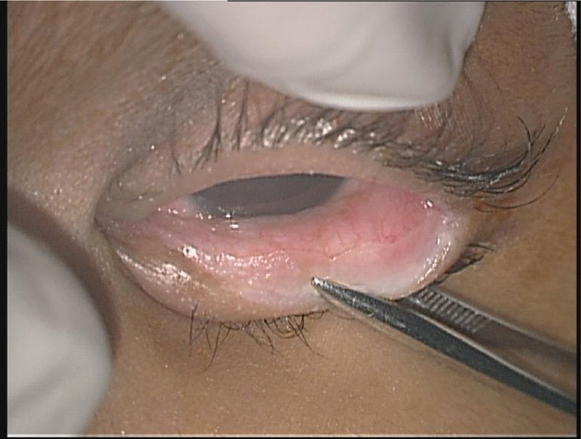
Clinical photograph at the time of consultation depicting SJS with symbhlepharon, early keratinisation and acute inflammation of both lower tarsal conjunctiva.

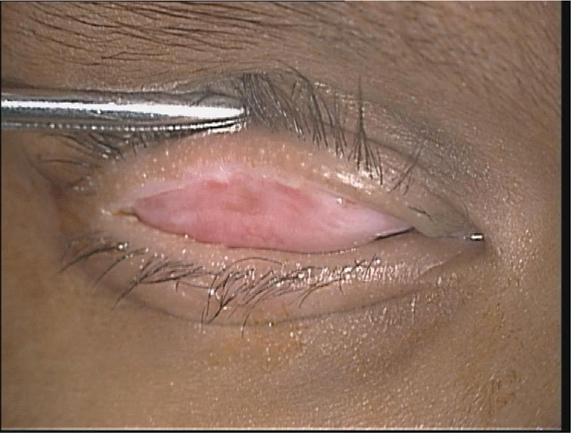
His ocular examination revealed visual acuity of 20/120 in both eyes with severe keratinisation of lid margin. The bulbar and tarsal conjunctival surface was adhered to each other especially in the forniceal region. There was chronic ocular surface inflammation with redness, watering, photophobia and corneal erosion due to chronic blink related microtrauma. Rest of ocular examination was normal. Indirect ophthalmoscopic examination revealed normal optic nerve head with attached retina. He had a preoperative Schirmer’s test value of zero. Diagnosis of post SJS sequel with keratinisation of lid margin and conjunctiva was made [Table/Fig-2,3]. He was advised MMG with minor salivary gland transplantation under general anaesthesia. His complete blood count, serum electrolytes, renal function test and liver function test were normal. His Hepatitis B Virus Surface Antigen (HbsAg) and Human Immunodeficiency Virus (HIV) test were negative. After physician’s evaluation and anaesthetic fitness, patient was taken up for surgery.
Clinical photograph at the time of procedure depicting SJS with keratinisation of left lower tarsal conjunctiva.
Clinical photograph at the time of procedure depicting SJS with keratinisation of right upper tarsal conjunctiva.
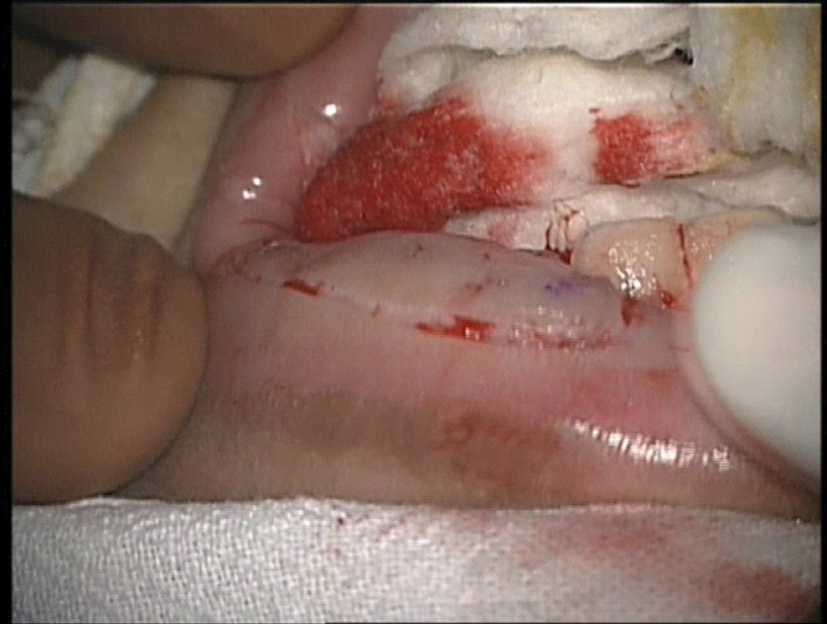
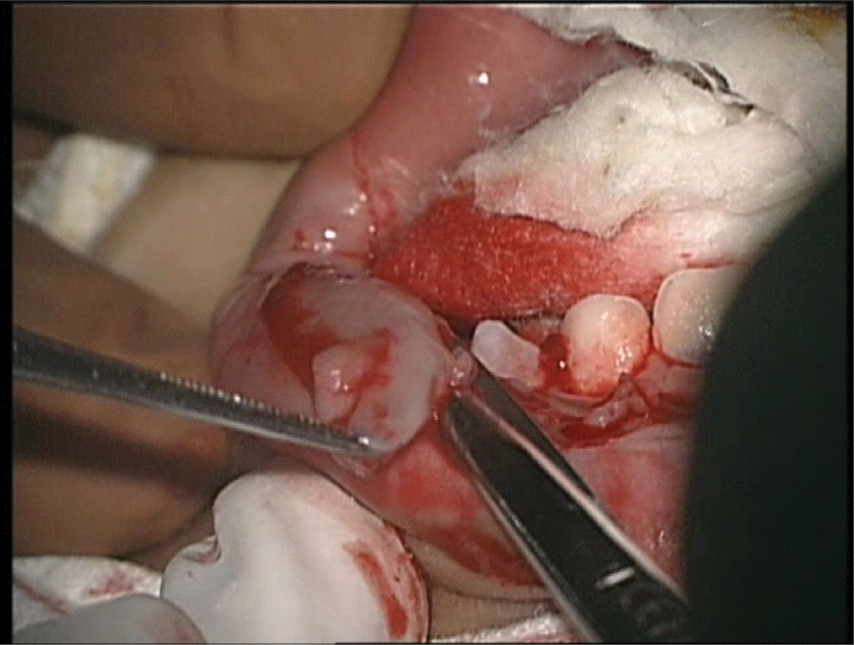
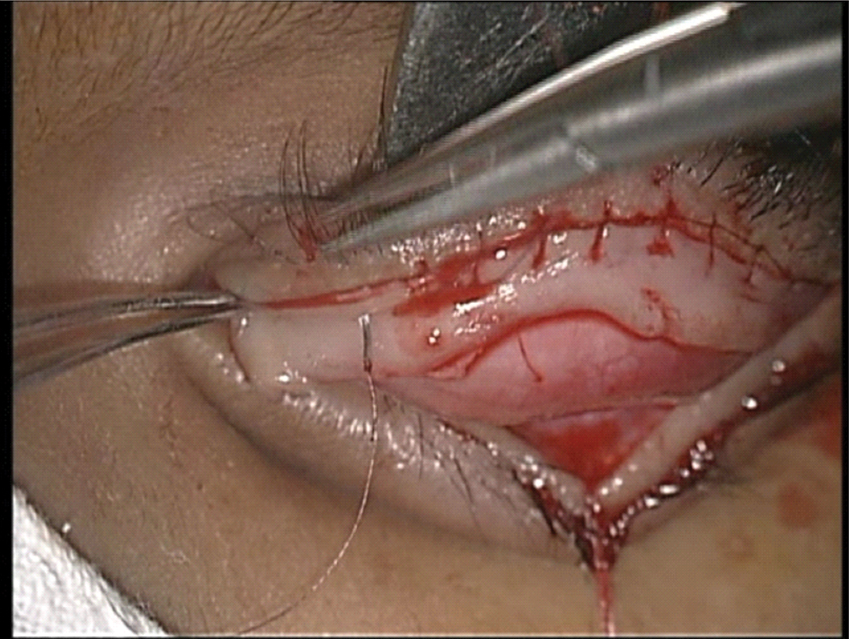
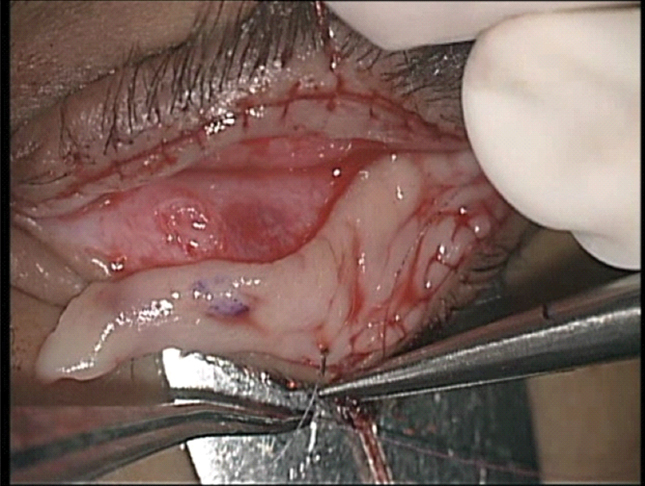
Patient was taken under general anaesthesia with cuffed endotracheal tube. Approximately 2-3 ml of lignocaine with adrenaline (1:80,000) was injected along upper and lower lid skin creases. A cotton suture was placed through upper eyelid margin centrally and eyelid everted over desmarres lid retractor. Incision along inner lid margin was taken with No. 15. Scalpel blade for excision of keratinised conjunctiva [Table/Fig-4,5]. Careful superficial dissection was done between palpebral and bulbar conjunctiva so as to release symblepharon. There were few areas of corneal peripheral neovascularization suggestive of localised deficiency of limbal stem cell.
Incision along inner lid margin.
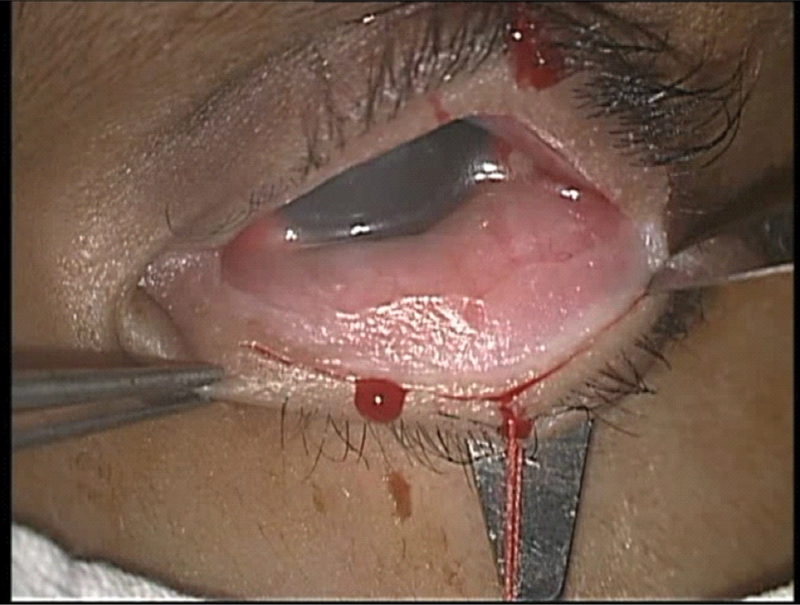
Excision of keratinised conjunctiva.
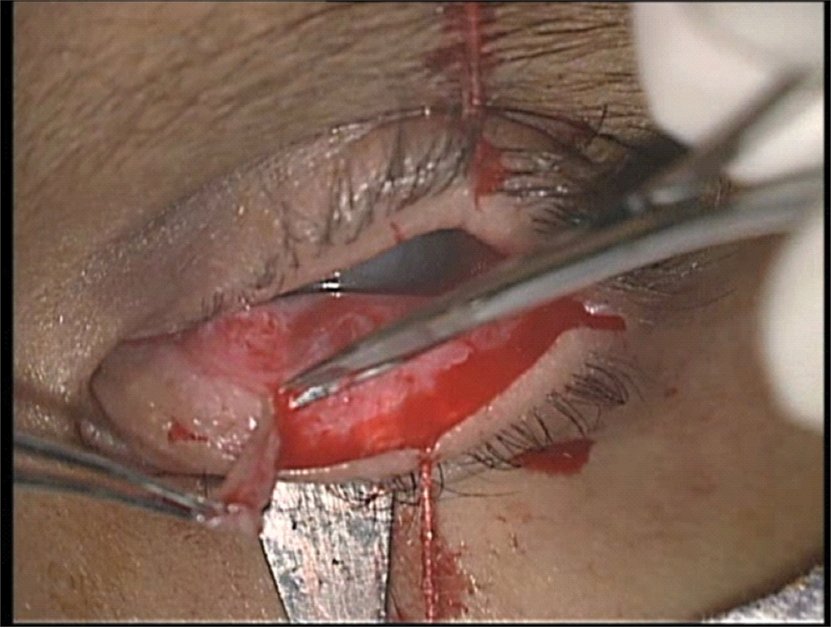
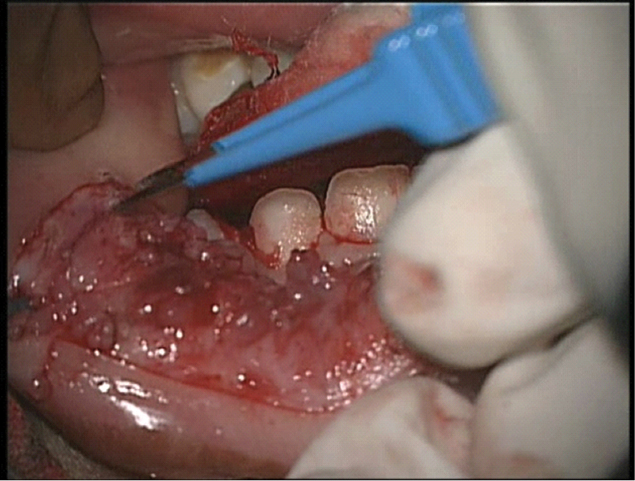
Size of the defect was measured with the help of vernier calliper in both horizontal and vertical direction. The horizontal length would approximate to the length of lid margin and vertical length from lid margin to the apex of conjunctival raw area. A template out of sterile paper was made in elliptical shape roughly corresponding to this size. This was followed by injecting lower lip mucosa with lignocaine with adrenaline (1:80,000). The template was transferred on mucosa and it was marked by sterile gentian violet avoiding vermillion border of lip and frenulum. Marked mucosal area was incised with No. 15 blade and graft was removed by careful dissection with westcott scissor and lim’s forceps [Table/Fig-6,7]. The donor site was compressed with adrenaline soaked swab and bipolar cautery was used for bleeding vessels [Table/Fig-8] and donor site was kept raw to heal by secondary intention.
Incision of Marked mucosal area with No. 15 blade.
Careful dissection of MMG with westcott scissor.
Bipolar cautery for bleeding vessels.
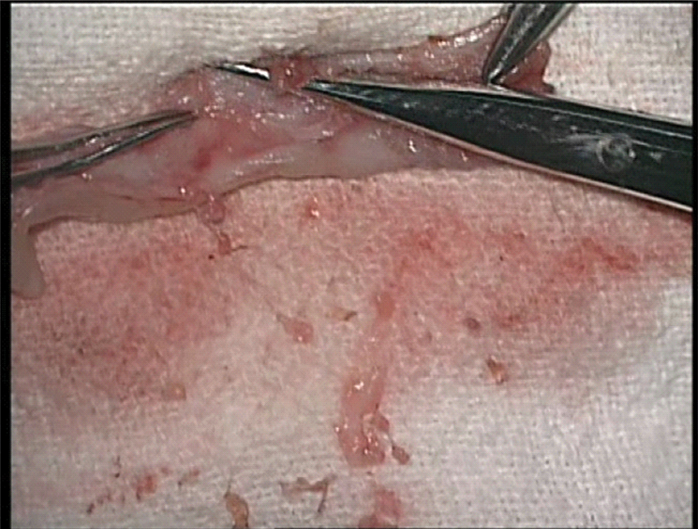
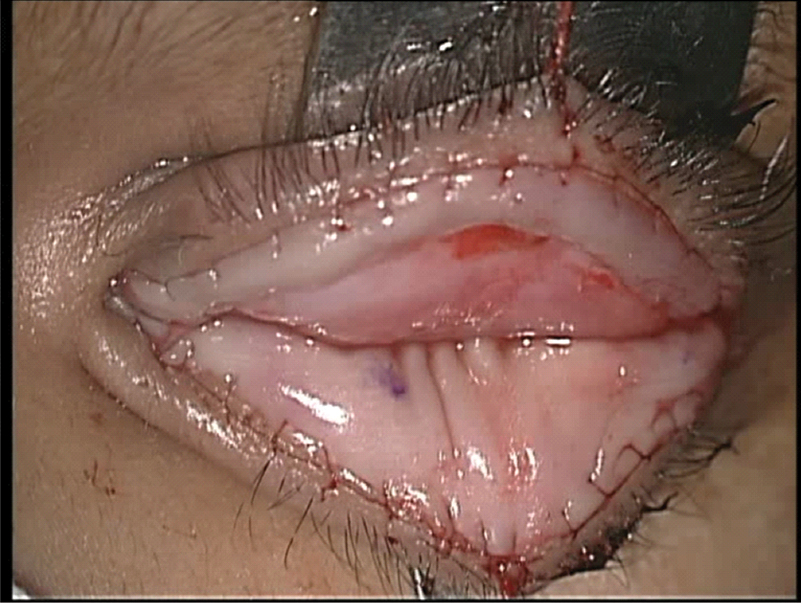
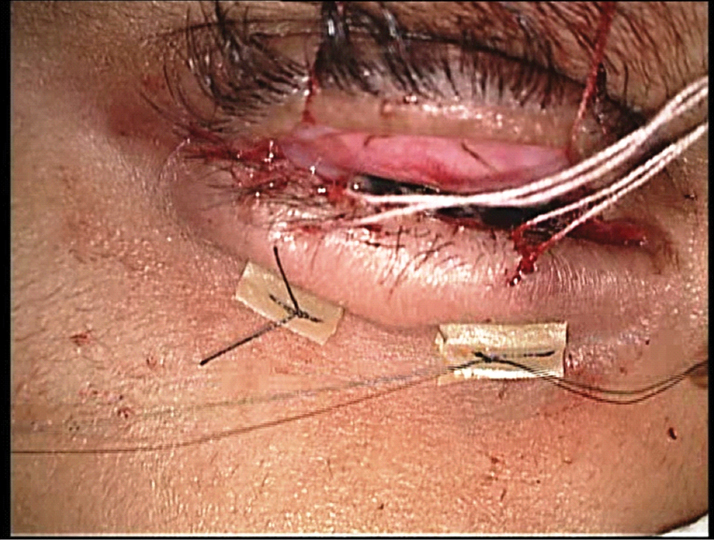
Underlying fatty tissue was removed after harvesting graft. [Table/Fig-9]. The graft was placed over raw surface of upper eye lid. The graft was sutured with 8-0 vicryl suture from lid margin [Table/Fig-10,11]. Only minor salivary glands that were pre-existing in graft were transplanted. Separate transplantation of minor salivary gland in fornix was not done in our technique. The free end of the graft was maintained in the position with the help of 5-0 silk suture passing through the graft and skin over pegs in a form of fornix deepening sutures [Table/Fig-12,13]. Topical eye drops containing dexamethasone 0.1% and moxifloxacin 0.5% were instilled and a compression dressing was applied.
Excision of excess fat from graft.
Suturing of graft with 8-0 vicryl suture to upper lid margin.
Suturing of graft with 8-0 vicryl suture to lower lid margin.
Final appearance of MMG covering entire raw area.
Graft maintained over pegs in a form of fornix deepening sutures.
The patient was instructed to avoid any hot drinks or hot food for a period of one week during which healing at donor site by secondary intention would be satisfactory. The patient was discharged on a broad spectrum oral antibiotic containing amoxicillin 500 mg and potassium clavulanate 125 mg for a week and an oral antiseptic mouth wash. Topical preservative free antibiotic drops containing dexamethasone 0.1% and moxifloxacin 0.5% were instilled into the eye four times a day for seven days. After this period the medication was gradually reduced over the following three weeks. A preservative free topical lubricant containing carboxymethylcellulose 0.5%, four times a day for a month was used. The patient was reviewed twice weekly to ensure that graft is well accepted and there are no corneal problems.
Patient recovery was very satisfactory. His visual acuity after two weeks was 20/60. After one month his final acuity was 20/40. He has been followed up for a year now without any complications or sequel. His postoperative Schirmer’s test value improved to six.
Discussion
Stevens-Johnson Syndrome is known to be caused by sensitivity reaction to various drugs, few vaccines, toxins, various infections, heavy X-ray therapy, radiation, food, malignancy etc. Among all above, sensitivity to drugs is the most important causative factor for SJS [1].
Ophthalmologists and oral and maxillofacial surgeons are mainstay in restoring anatomical structure and functional properties of ocular surface [2].
The chronic phase of SJS can have varied effects on ocular surface like trichiasis, entropion, repeated corneal erosions due to blink related microtrauma, symblepharon, limbal stem cell deficiency, corneal neovascularization and opacification, dry eye which can result in corneal blindness [3,4].
The mainstay of treatment in late stages is surgical definitive correction of cicatrising sequel [5]. Oral mucous membrane grafting with or without minor salivary gland is helpful for correcting such sequel. Minor oral salivary glands exist in large numbers in the labial, buccal and palatal mucosa, and contribute for half the baseline secretion of saliva. They can be transplanted with overlying mucosa as a complex graft to the posterior lamella of the eyelids. Murube-del-Castillo initially described mucous membrane and minor salivary gland transplantation for the treatment of severe cases of dry eye syndrome [6,7]. Soares and França described successful result with mucous membrane and minor salivary gland transplantation procedure in 21 cases of severe dry eye, of which 12 (57.1%) occurred due to SJS [8]. In a similar study done by Sant’ Anna AE et al., 19 patients with severe symblepharon and dry eye secondary to SJS who underwent labial mucous membrane and minor salivary glands transplantation were studied. There was a statistically significant improvement in the best spectacle-corrected visual acuity in eight patients; Schirmer’s test improved significantly in 14 eyes (73.7%) six months following surgery. Corneal transparency improved significantly in 11 (72.2%) eyes and corneal neovascularisation improved significantly in five eyes (29.4%). The symptoms questionnaire revealed improvement in foreign body sensation in 53.6% of the patients, in photophobia in 50.2% and in pain in 54.8% [9].
A mucous membrane graft can be removed free-hand or with the aid of a mucotome. It is generally easier and safer to remove such a graft free hand [10]. The donor sites are the lower lip, upper lip, and the buccal mucosa. The lower lip is preferred. The access is easier and no sutures are required to close the donor site wound which reepithelialises spontaneously over the course of two to three weeks. The buccal mucosa yields more graft material but normally has to be sutured and is not as accessible [11]. Great care must be taken to avoid damage to the parotid duct, whose opening is opposite the upper second molar tooth, when harvesting a buccal graft [12]. In cases with diffuse bilateral involvement of conjunctiva in SJS, possibility of autologous graft from other eye is unlikely. Also cultured stem cells over amniotic membrane graft are highly costly and not readily available hence, MMG becomes obvious choice for reconstruction [13,14]. The various ophthalmic indications are ocular surface reconstruction post Symblepharon release, excision and replacement of keratinised conjunctiva in SJS, Lid reconstruction as posterior lamella [15]. As a spacer for lid retraction, severe eyelid cicatricial entropion, conjunctival replacement following an enucleation, with minor salivary gland in dry eye treatment and with cultivated stem cells for contracted socket.
However, until present, surgical repair has been difficult and outcomes are still uncertain. Despite the huge variety of procedures done, no single procedure has been standardized. In many occasions, it is hard to find healthy conjunctiva with limbal stem cell to be used as a graft. Mucous membrane on the other hand is readily available and is the simplest graft.
Conclusion
The exact etiopathogenesis regarding SJS is still far from known. Mainstay of treatment in late stages is surgical definitive correction of cicatrising sequel. In chronic phase, where ocular surface inflammation is present autologous or allogenic limbo-conjunctival graft containing stem cells are best for transplantation purpose. However, due to bilateral ophthalmic involvement in most of the SJS cases like in our case conjunctival tissue is rarely available. Hence, autologous graft like oral MMG are best because of easy availability and cost-effectiveness over cultivated stem cell graft on amniotic membrane in a limited infrastructure setting. This technique definitely improves visual acuity and alleviates patient discomfort by improving ocular surface environment avoiding blink related microtrauma.
[1]. Bianchine JR, Macareg PV, Lasang LI, Azarnoff DL, Brunk SF, Hvidberg EF, Drugs as Histological factors in SJ SyndromeAm J Med 1968 44(3):390-405. [Google Scholar]
[2]. Beedimoni RS, Rambhimaiah S, Oral chloroquine-induced Stevens - Johnson syndromeIndian J Pharmacol 2004 36(2):101 [Google Scholar]
[3]. Stewart MG, Duncan NO 3rd, Franklin DJ, Friedman EM, Sulek M, Head and neck manifestations of erythema multiforme in childrenOtolaryngol Head Neck Surg 1994 111(3Pt1):236-42. [Google Scholar]
[4]. Tsubota K, Satake Y, Kaido M, Shinozaki N, Shimmura S, Bissen-Miyajima H, Treatment of severe ocular surface disorders with corneal epithelial stem-cell transplantationN Engl J Med 1999 340(22):1697-703. [Google Scholar]
[5]. Shimazaki J, Yang H-Y, Tsubota K, Amniotic membrane transplantation for ocular surface reconstruction in patients with chemical and thermal burnsOphthalmology 1997 Dec 104(12):2068-76. [Google Scholar]
[6]. Murube-del-Castillo J, Transplantation of salivary gland to the lacrimal basinScand J Rheumatol 1986 61:264-67. [Google Scholar]
[7]. Denig R, The indications for immediate transplantation of buccal mucous membrane for eye burnsMed Record 1938 148:395-99. [Google Scholar]
[8]. Soares EJ, França VP, [Transplantation of labial salivary glands for severe dry eye treatment]Arq Bras Oftalmol 2005 68(4):481-89. [Google Scholar]
[9]. Sant’ Anna AE, Hazarbassanov RM, de Freitas D, Gomes JÁ, Minor salivary glands and labial mucous membrane graft in the treatment of severe symblepharon and dry eye in patients with Stevens-Johnson syndromeBr J Ophthalmol 2012 96(2):234-39. [Google Scholar]
[10]. Brian Leatherbarrow: Oculoplastic Surgery Second Edition 2011, Informa Healthcare Ltd [Google Scholar]
[11]. Henderson HW, Collin JR, Mucous Membrane GraftingDev Ophthalmol 2008 41:230-42. [Google Scholar]
[12]. Putterman (1980): Basis oculoplastic surgery in Peyman GA: Principles and practice of ophthalmology, Vol. 3. Philadiphia: WB Saunders Company, 2246-2333 [Google Scholar]
[13]. Shimazaki J, Shinozaki N, Tsubota K, Transplantation of amniotic membrane and limbal autograft for patients with recurrent pterygium associated with symblepharonBr J Ophthalmol 1998 82(3):235-40. [Google Scholar]
[14]. Azuara-Blanco A, Pillai CT, Dua HS, Amniotic membrane transplantation for ocular surface reconstructionBr J Ophthalmol 1999 83(4):399-402. [Google Scholar]
[15]. Bartley GB, Kay PP, Posterior lamellar eyelid reconstruction with a hard palate mucosal graftAm J Ophthalmol 1989 107(6):609-12. [Google Scholar]