Biomedical waste is any waste which is generated during the diagnosis, treatment or immunisation of human beings or animals or in research activities pertaining there to or in the production or testing of biologicals [1]. Keeping pace with the increasing population, last decade has also seen the surge in the number of hospitals and with that has increased the burden of BMW.
As per WHO report, hospital waste generated is either general waste (80%) or infectious/toxic waste (20%) [2]. The general waste is treated like a municipal waste, whereas the infectious waste requires proper handling so as to avoid any spread of infections.
As per Ministry of Environment and Forests (MoEF) estimates, almost 4,05,702 kg waste is generated daily, of this 28% is left untreated and this acts as a health hazard by entering the system again [3]. The improper disposal of BMW not only predisposes the hospital staff and patients to risk of infections but also poses a risk to environment. A study by Patel DA et al., found that the hepatitis outbreak in Gujarat, 2009 was due to poor management of BMW [4].
BMW disposal and treatment requires special precaution with scientifically sound method of disposal. To streamline the process and to avoid the BMW related health hazard, MoEF, Government of India (GoI) notified the BMW (Management and Handling) Rules 1998 under the Environment Protection Act 1971. Since, the earlier rule was liberal and ambiguous on certain fronts, a new rule was introduced in 2011 which was more elaborate and stringent which were further amended and new rules were notified on 28th March 2016 [5].
BMW management is dependent on activities ranging from collection, segregation, transportation, operation, treatment, and final disposal of waste [1]. The potential of BMW to spread pathogens mandates the proper disposal of waste as per the aforesaid rules. There are multiple studies which have evaluated the status of BMW management in few hospitals, but there is paucity of studies depicting the status of BMW management at country level.
The present study was planned to document existing infrastructure and practices related to BMW management across the districts at country level using DLHS-4 data. The concept of DLHS was conceived to have a comprehensive picture of health profile of districts annually. However, keeping in view the large sample size, it was consciously decided by the GoI to confine the survey to poor performing states; AHS states. Thus, the study analysis is also categorised into two groups; AHS and non-AHS.
Materials and Methods
DLHS-4, fourth in series conducted in 2012-2013, was preceded by three rounds in the past, DLHS-1 in 1998-1999, DLHS-2 in 2002-2003, DLHS-3 in 2008-2009. In DLHS-4, the facility survey was also conducted to collect information regarding the availability of human resources, physical infrastructure, equipment, essential drugs, and Maternal and Child Health (MCH) services during one month preceding the survey. The DLHS- 4 was conducted in 30 states and Union Territories (UTs), of which nine states were part of AHS and 21 states were non-AHS states. The data was released in December, 2015 in public domain.
Computer Assisted Personal Interview (CAPI) was used for data collection. For this, interviewers were provided with mini laptops with bilingual questionnaire (English and local language). The data collection was done using pretested structured questionnaires. Separate questionnaires were used for each level of facility-Sub Health Centre (SHC), Primary health centre (PHC), Community Health Centre (CHC), and DH.
Ethics statement: The proposal of DLHS was assessed and approved by Indian Institute of Population Studies (IIPS), Mumbai, India, Ethical Committee in association with Ministry of Health and Family Welfare (MOHFW), India. The entire dataset is available for download upon requesting Director, IIPS.
Study population: In each district, Primary Sampling Unit (PSU) was selected based on Probability Proportional to Size (PPS) systematic random sampling. The SHC catering to selected PSU (rural area) was selected. The PHC catering to the SHC was selected whereas all the CHC and DH in a district were selected for the survey.
Respondent: The information was sought from health facilities either by directly asking the concerned officials, physical inspection or by recording from relevant registers. For a SHC, ANM or health worker was the respondent. The Medical Officer acted as a respondent in case of PHC. For CHC and DH, Medical Superintendents (MS) and Administrative Officers (AO) was the respondent.
Measures: The study considered BMW disposal infrastructure and practices related variables for which information was sought in facility based DLHS-4.
Mode of disposal of infectious/non-infectious BMW: For this information was obtained by asking the respondent about the method of disposal of waste. For this, options were – deep burial pit, bury in a pit, thrown in common public disposal pit, thrown outside hospital compound, thrown inside hospital compound, incinerator, and outsourced.
Segregation and treatment before disposal: For this, question asked in the survey was “Is biomedical waste segregated and treated before disposal”. The question for the same was only present for PHCs and CHCs in DLHS questionnaire.
Availability of various instruments and infrastructure related to BMW disposal: The respondents were asked about the availability of colour coded bags and the same were observed also.
Colour coded waste bags: For this, information was sought by asking question “Are colour coded waste bags available for segregated waste?”
Sharps: For this, investigators has observed and recorded if any sharps were found in the facility.
For questions having multiple responses, all the responses mentioned by the respondents were recorded.
Statistical Analysis
Stata 12.0 was used for analysis of data available. The proportions and 95% Confidence Intervals (CI) were presented wherever appropriate.
Results
The facility level DLHS-4 data on BMW was analysed at SHC, PHC, CHC, and DH; total observations made were 11322, 4487, 2779, and 547 respectively.
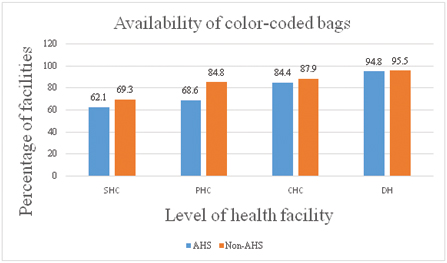
Availability of Colour-coded Bags
In AHS states, the colour-coded bags for segregation of BMW was present in 62.1% (7019) of SHC, 68.6% (3078) PHC, 84.4% (2345) CHC, and 94.8% (516) DH. Whereas in non-AHS states, the situation was relatively better with 69.3% (487) SHC, 84.8% (3436) PHC, 87.9% (1785) CHC, and 95.5% (935) DH having colour coded bags in place [Table/Fig-1].
Distribution of availability of colour-coded bags across the health facilities in AHS and non-AHS districts.
Different dustbins for BMW: Only the availability of colour-coded bags does not ensure the proper disposal as it further depends upon availability of different dustbins and also the practices of the waste handler in the health facilities. The information for this was not available for SHC and DH. In AHS states, 74.6% (3344) of PHCs and 89.8% (2497) of CHCs were using different dustbins for throwing the BMW. While in Non-AHS states, 91.6% (3712) PHCs and 93.9% (1908) CHCs were using different coloured dustbins [Table/Fig-2].
Distribution of healthy practices of biomedical waste disposal across health facilities.
| Level of health facility | PHC | CHC |
|---|
| Region | AHS | Non-AHS | AHS | Non-AHS |
| Use of different dustbins | 3344 (74.6) | 3712 (91.6) | 2497 (89.8) | 1908 (93.94) |
| Segregation and treatment | 3401 (75.8) | 3593 (88.6) | 2318 (83.5 | 1871 (92.2) |
Segregation and treatment of BMW before disposal: The required data for this was not available for SHC and DH. In AHS states, 75.8% (3401) PHCs and 83.5% (2318) CHCs were segregating and treating the waste before disposal. While in non- AHS states, 88.6% (3593) of PHC and 92.2% (1871) of CHC were performing the practice of segregation [Table/Fig-2].
Disposal of Infectious Waste
Recommended methods of disposal
Use of incinerator: Incinerator, a waste treatment method which results in significant reduction of waste-volume and weight, is a high temperature and dry oxidation process which reduces organic and combustible waste to inorganic incombustible matter. The situation is grave all over India across the facilities in both AHS and non-AHS states, as evident by the non-availability of the incinerator. In AHS states, incinerator was present only in 2.2% (249) SHCs, 2.5% (112) PHC, 3.0% (84) CHC and 7% (38) DH. In non-AHS states, the situation was almost similar with availability of incinerator in 6.6% (462) SHCs, 9.5% (384) PHCs, 8.1% (165) CHCs and 11.2% (108) DH [Table/Fig-3].
Distribution of recommended and non-recommended method of disposal of infectious waste.
| Level of health facility | SHC | PHC | CHC | DH |
|---|
| Region | AHS | Non-AHS | AHS | Non-AHS | AHS | Non-AHS | AHS | Non-AHS |
| Recommended method of disposal |
| Incinerator | 249 (2.2) | 462 (6.6) | 112 (2.5) | 384 (9.5) | 84 (3.0) | 165 (8.1) | 38 (7.0) | 108 (11.2) |
| Deep Burial | 2083 (18.4) | 2231 (31.7) | 2197 (49.0) | 2591 (63.9) | 1715 (61.7) | 1057 (52.1) | 210 (38.5) | 275 (28.3) |
| Bury in a pit | 3472 (30.7) | 2333 (33.1) | 1692 (37.7) | 1533 (37.8) | 785 (28.2) | 541 (26.6) | 89 (16.4) | 155 (16.1) |
| Outsourcing | 3705 (32.8) | 1341 (19.1) | 739 (16.5) | 666 (16.4) | 704 (25.3) | 830 (40.9) | 326 (59.9) | 697 (71.2) |
| Non-Recommended method |
| Thrown in common public disposal pit | 161 (1.4) | 154 (2.2) | 45 (1.0) | 68 (1.7) | 24 (0.9) | 56 (2.8) | 9 (1.7) | 30 (3.1) |
| Thrown inside hospital compound | 146 (1.3) | 140 (2.0) | 129 (2.9) | 65 (1.6) | 64 (2.3) | 40 (2.0) | 12 (2.2) | 19 (2.0) |
| Thrown outside hospital compound | 275 (2.4) | 179 (2.5) | 122 (2.7) | 57 (1.4) | 42 (1.5) | 40 (2.0) | 9 (1.7) | 26 (2.7) |
Deep burial of infectious waste: In AHS states, deep burial of infectious waste was done in only 18.4% (2083) of SHC, 49.0% (2197) of PHC, 61.7% (1715) CHC and 38.5% (210) DH. In non-AHS states, 31.7% (2231) SHC, 63.9% (2591) PHC, 52.1% (1057) of CHC and 28.3% (275) of DH were using the method of deep burial as a method of disposal of infectious waste [Table/Fig-3].
Bury in pits: In AHS States, 30.7% (3472) of SHC, 37.7% (1692) of PHCs, 28.2% (785) of CHCs and 16.4% (89) of DH were using the modality of burial in pits as a method of disposal of infectious BMW. In non-AHS states, infectious BMW was disposed by burying in pits in 33.1% (2333) of SHCs, 37.8% (1533) PHCs, 26.6% (541) CHCs and 16.1% (155) DH [Table/Fig-3].
Outsourcing of the BMW disposal: Outsourcing the disposal of the BMW was done in 32.8% (3705) of SHCs, 16.5% (739) of PHCs, 25.3% (704) of CHCs and 59.9% (326) DH in AHS states and 19.1% (1341) of SHCs, 16.4% (666) of PHCs, 40.9% (830) of CHCs and 71.2 % (697) of DH in non-AHS states [Table/Fig-3].
Non-recommended methods of disposal
It was observed that both AHS and non-AHS states were practising the hazardous methods of disposing the infectious biomedical waste either by throwing it in common disposal pit or by disposing it inside or outside the premises. In both AHS and non-AHS states, quite a large number of facilities were throwing their waste either inside or outside the facility in open [Table/Fig-3].
Disposal of non-infectious BMW
Recommended methods: The recommended methods for non-infectious waste disposal are either through throwing it in public disposal pit or deep burial or burial pit.
In AHS states, the SHCs (34.8 %) and PHCs (43.2 %) were disposing their non-infectious biomedical waste by burying it in pit whereas the DHs (56.0 %) were mainly relying on outsourced agencies for disposal of their non-infectious BMW, while most of the CHCs (47.7%) are practising the method of deep burial for disposal of their non-infectious BMW. In non-AHS states, PHCs (53.7%) and CHCs (44.8%) were mainly deep burying their non-infectious biomedical waste, while SHCs (35.0%) and DHs (65.0%) as in AHS states were disposing their non-infectious waste through burying in pit and outsourcing respectively [Table/Fig-4].
Distribution of recommended and non-recommended method of disposal of non- infectious waste.
| Level of health facility | SHC | PHC | CHC | DH |
|---|
| Region | AHS | Non-AHS | AHS | Non-AHS | AHS | Non-AHS | AHS | Non-AHS |
| Recommended method of disposal |
| Thrown in common/public disposal pit | 251 (2.2) | 214 (3.0) | 50 (1.1) | 96 (2.4) | 46 (1.7) | 70 (3.4) | 24 (4.4) | 63 (6.6) |
| Outsourcing | 3288 (29.1) | 1284 (18.2) | 711 (15.8) | 664 (16.4) | 664 (23.9) | 802 (39.5) | 304 (56.0) | 630 (65.0) |
| Deep burial pit | 1746 (15.4) | 2104 (29.9) | 1664 (37.14) | 2174 (53.7) | 1324 (47.7) | 910 (44.8) | 154 (28.4) | 270 (27.8) |
| Bury in a pit | 3934 (34.8) | 2462 (35.0) | 1935 (43.2) | 1651 (40.8) | 1061 (38.2) | 597 (29.4) | 118 (21.8) | 163 (16.9) |
| Non-Recommended method |
| Incinerator | 433 (3.8) | 505 (7.2) | 191 (4.3) | 461 (11.4) | 124 (4.5) | 194 (9.6) | 34 (6.3) | 104 (10.8) |
| Thrown outside Health facility compound | 359 (3.2) | 194 (2.8) | 137 (3.1) | 76 (1.9) | 53 (1.9) | 48 (2.4) | 15 (2.8) | 33 (3.4) |
| Thrown inside Health facility compound | 198 (1.8) | 138 (2.0) | 134 (3.0) | 82 (2.0) | 84 (3.0) | 38 (1.9) | 14 (2.6) | 29 (3.0) |
Non-recommended methods: A substantial number of health facilities were not following the recommended methods of disposal of non-infectious biomedical waste [Table/Fig-4].
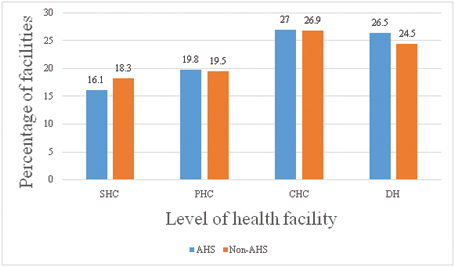
Disposal of waste sharps: In about 27% of CHCs in both AHS and non-AHS states, the discarded sharps were seen in the health facility, followed by about 25% DH and 19% PHCs and about 17% SHCs [Table/Fig-5].
Distribution of any discarded/ used sharps visible in the health facility in AHS and non-AHS districts.
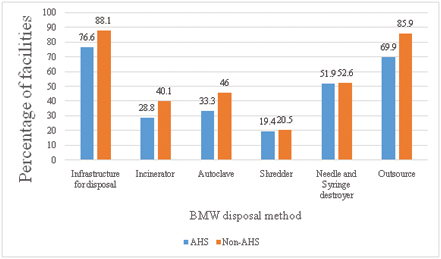
BMW disposal facilities in DH
DHs are the most equipped health facilities. In 76.6% DH in AHS states and 88.1% in non-AHS states, the facility for disposal of BMW was present. In AHS states, incinerators, autoclave, shredder and needle and syringe destroyers was available at only 28.8%, 33.3%, 19.4%, and 51.9% of DH respectively. The situation was almost similar in the non-AHS states [Table/Fig-6].
Availability of BMW disposal related infrastructure in district hospital.
Discussion
The present study was undertaken using DLHS-4 data to document the BMW disposal practices at country level.
The first step in BMW is segregation followed by correct use of colour-coded bags and dustbins. With segregation in place, the amount of infectious waste generated is only 12-15%. However, in the absence of segregation all the infectious and non-infectious BMW generated turns infectious; thus, highlighting the importance of segregation. It was observed in this study that all the facilities were not following the practice of segregation. Similar findings of not practising segregation were documented in other studies done in Bengaluru, Lucknow, Karachi, and Kathmandu [6-9]. The contrasting findings of exemplary segregation was observed in a study conducted in 1100-bedded hospital in North Delhi and Lucknow [10,11]. The reasons were the continuous assistance and supervision. Thus for proper segregation, there should be continuous supervision from health facility Incharge.
The non-availability of colour-coded bags in most of the sub centres and PHCs highlights the worrisome situation of poor resources and infrastructure in primary level health facilities. The situation was found relatively better in CHCs and DHs. The previous studies done had reported similar worrisome situation in primary health facilities [12,13].
The next step in BMW management is proper disposal of infectious and non-infectious waste as per the BMWM Rules, 1998. It was observed that recommended methods for disposal of BMW were better in health facilities of non-AHS states than their T counterparts in AHS states. The availability of resources and infrastructure for BMW disposal at sub centres and PHCs were poor than CHCs and DHs. Incinerator was present in only a few facilities. It was also observed that apart from using it for infectious BMW, it was also used for the disposal of non-infectious waste. A study done in Chandigarh and urban Delhi highlighted the similar finding of either the non-availability or non-functionality of incinerator [12,13]. It was observed that in a few facilities the BMW was thrown in open either in the premises of the facility or outside. The similar scenario of improper disposal of BMW was reported from several studies. The study conducted by Sharma S and Chauhan SV, reported that waste was either thrown inside or outside which was further either burnt or disposed along with municipal waste [14]. Similar practice was observed to be followed by facilities in rural setting of Gwalior and Balrampur Hospital [7,15]. The study conducted in Karachi by Rasheed S et al., observed that only 25% hospitals were having proper waste management system [8]. The similar finding of disposing BMW along with municipal waste was observed in study conducted in Kathmandu and Dhaka [9,16]. The mixing of infectious BMW along with municipal waste jeopardises the proper disposal and is a health hazard not only for staff but also for patients and attendants visiting the facility.
It is recommended that sharps waste should be disposed by burying in deep pit. Sharps waste were seen in the vicinity of the facilities in about one-fourth of DHs in both AHS and non-AHS states and this clearly indicates the breach in the management of BMW and is a source of concern.
In contrast to previous studies, a study done by Joseph L et al., in a tertiary care centre in southern India demonstrates that the focussed training, strict supervision, daily surveillance and periodic audit along with regular appraisal significantly improves the awareness among healthcare workers and actual practices of BMW management [17]. However, there was no provision for audit of BMW management and training of the healthcare workers in BMW (Management and Handling) Rules, 1998. The importance of training of the healthcare workers is emphasized in BMW Management Rules, 2016, which states that the onus of training of all healthcare workers and others involved in handling of BMW lies with the occupier and operator of common BMW treatment and disposal facility at the time of induction and thereafter at least annually. However, there is still no provision for audit.
The strength of the study lies in the fact that it is a nationwide survey for highlighting the BMW disposal practices. Improper disposal of BMW is one of the important hazards for healthcare providers, paramedical staff, and those involved in collecting the waste generated. The study will guide the policy makers in directing the efforts towards the gaps found in waste management.
Limitation
The limitation of the study was that the respondents were only asked about the availability of instruments and the functionality status was not assessed.
Conclusion
This study provides the overview of BMW management at the country level. The situation is worrisome across the health facilities. The BMW disposal infrastructure is not in place and proper guidelines are not being followed across the health facilities in both AHS and non-AHS states. The emphasis should be laid upon the provision of various infrastructure and equipment related to waste management. Also, hospital administration should conduct induction and refresher training sessions for the healthcare staffs so as to ensure the proper disposal of BMW.