Given the high incidence of thyroid diseases and the spread of other treatments, there is still a need for thyroid surgery at the end of the treatment of some patients. Thyroid is in close proximity to trachea, oesophagus, carotid, internal jugular vein and the laryngeal nerves and high blood supply of thyroid from several sources always aware the doctors of the fundamental point that thyroid surgery is highly sensitive and precise dissection requires a delicate haemostasis [1]. Although, there is a consensus in reliable sources and articles on insertion of drain after thyroid surgery in rare cases, such as retrosternal thyroid and cervical lymphatic dissection, the lack of use of drain in uncomplicated thyroid surgery is controversial [2]. Many surgeons routinely use open or closed drains in all thyroid surgeries and in some old reference books, the use of drain is also recommended [3]. However, in some studies, it has been indicated that the use of drain should be reduced as much as possible. It has also been reported that the use of drain after uncomplicated thyroid surgery is not useful [4-6].
Some literatures showed that the morbidity between the two groups with and without drain did not differ [7,8]. Furthermore, it was found that the incidence of wound complications is not related to the lack of use of drains [9]. On the other hand, some surgeons believe that insertion of drain after thyroid surgery increases the incidence of wound infection and therefore, its use in thyroid and parathyroid surgery should be optional [10] because in the case of using drain: 1) The need for careful haemostasis will not be met, 2) The possibility of drain displacement and problems caused by it is high, 3) It creates a dead tissue space, which interferes in wound healing, 4) The secretion of interstitial fluid can be stimulated, leading to increase in the drainage secretion, 5) The patient’s post-operative hospitalisation is long, 6) It damages the patients psychologically and they are not pleased with drain use, 7) Additional financial cost will be imposed on patients, 8) Scar of drain exit site is also unpleasant.
Considering the controversy between different studies and also surgeons experiences in the field of insertion or non-insertion of drain after thyroidectomy, we aimed to investigate the advantages and disadvantages of inserting drains in thyroid surgeries.
Materials and Methods
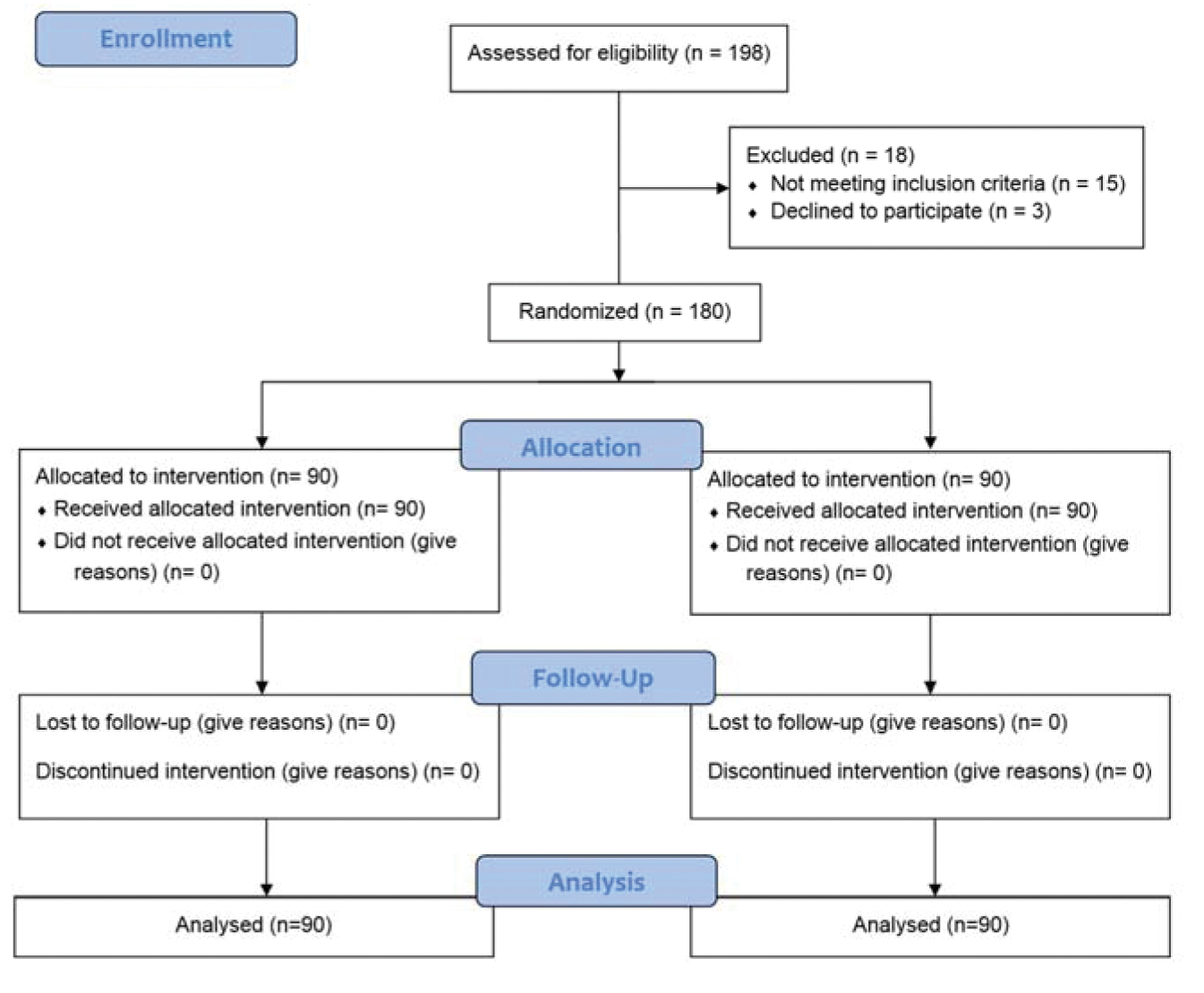
Study population and data collection: Between the years January 2013 to March 2015, a prospective randomised clinical trial was performed on patients referred to Shahid Beheshti and Ayatollah Rohani hospitals in Babol, north of Iran, diagnosed with thyroid cancer, multinodular goiter and thyroid nodules that were candidates for total or subtotal surgery of thyroidectomy or lobectomy. The following subjects were excluded from the study: 1) Patients with coagulation disorders or underlying disease (diabetes and cardiovascular diseases) or retrosternal thyroid, 2) Patients who needed modified dissection or radical neck dissection during surgery. The patients were assigned into two groups with or without drain by random allocation, using computer generated numbers. The Consolidated Standards for Reporting Trials (CONSORT) flowchart of the participants is shown in [Table/Fig-1].
Drain type was closed and it was removed when drainage was less than 30 ml within 24 hours. Data were collected through interviews, checklist and examination. The study variables, including age, gender, Body Mass Index (BMI), smoking history, family history of thyroid diseases, type of surgery, duration of surgery, and length of hospital stay, were collected from all participants. Post-thyroidectomy complications, such as hematoma, seroma, infection, transient hypocalcaemia and recurrent laryngeal nerve paralysis, were investigated by examinations. On the first, third and 30th day after the surgery, the surgical site was visited in terms of bleeding, hematoma (swelling, neck pain and/or airway obstruction symptoms), seroma (leakage of clear fluid, swelling, redness and/or warmth) and wound infection (redness, inflammation, heat, pain, fever and/or infectious secretions).
Ethical issues: This article was registered in Iranian Registry of Clinical Trials (IRCT2016030319255N4). The informed consent was obtained from all individuals.
Statistical Analysis
The collected data were analysed using SPSS version 16.0. Chi-square and t-test tests were used to compare between the qualitative and quantitative variables and the two groups with and without drain. We initially evaluated the differences of the factors, including age, gender, BMI, smoking history, family history of thyroid diseases and type of surgery, between the two groups. These potential variables have been reported to be associated with risk of thyroid surgery complications, such as bleeding or hematoma [11-13]. A p-value <0.05 was considered as statistically significant.
Results
One hundred eighty patients were recruited in this study and randomly divided into two groups: group I consisted of 90 subjects without drains, and group II consisted of 90 subjects with drains. Thirty seven patients (20.6%) were males and others were females with a ratio of 1:4. The mean age was 41.44±13.65, ranged from 20 to 75 years. The mean duration of surgery was 139.58±39.71 minutes and the mean duration of hospitalisation was 2.27±0.74 days in all patients. Between the two groups, there were no significant differences in terms of age, sex, BMI, family history and smoking history and duration of surgery [Table/Fig-2].
Patients characteristics.
| Variable | Group Ia (n=90) | Group IIb (n=90) | p-value |
|---|
| Age (Mean±SD) | 41.50±13.65 | 41.38±13.73 | 0.71 |
| Gender |
| Male | 18 (20%) | 19 (21.2%) | >0.999 |
| Female | 72 (80%) | 71 (78.8%) |
| BMI* (Mean±SD) | 24.39±2.22 | 25.03±2.64 | 0.44 |
| Family history of thyroid |
| Yes | 18 (20%) | 24 (26.7%) | 0.29 |
| No | 72 (80%) | 66 (73.3%) |
| Smoking history |
| Yes | 5 (5.6%) | 4 (4.4%) | 0.73 |
| No | 85 (94.4%) | 86 (95.6%) |
| Type of surgery |
| Malignant mass | 30 (33.3%) | 30 (33.3%) | 0.99 |
| Benign mass | 30 (33.3%) | 30 (33.3%) |
| Right lobectomy | 15 (16.7%) | 14 (15.6%) |
| Left lobectomy | 15 (16.7%) | 16 (17.8%) |
| Mean duration of surgery (Min) | 131.94±38.85 | 147.22±39.31 | 0.009 |
a Group I consisted of subjects without drains
b Group II consisted of subjects with drains
* Body mass index
Hematoma, seroma, infection and laryngeal recurrent nerve damage were not seen in any of the patients in both groups. The [Table/Fig-3] shows surgical site of a patient after total thyroidectomy, with no complications. [Table/Fig-3]. Transient hypocalcaemia was seen in 35 patients (19.4%), only on the first day after surgery, which was higher in group II 19 (21.1%) than in other group 16 (17.7%), but the difference was not statistically significant [Table/Fig-4]. Also, there was a significant difference in occurrence of transient hypocalcaemia between the total thyroidectomy group 32 (26.6%) (benign cases=15, malignant cases=17) and lobectomy group three (0.05%) (p<0.0001). The duration of hospitalisation of patients was 2.18±0.80 and 2.36±0.67 days in the groups without and with drain, respectively, but this difference was not significant (p=1).
The surgical site of total thyroidectomy for papillary thyroid carcinoma (one day after surgery). No complications are seen in the patient without drain.

Comparison of post-operative variables between the groups with and without drain.
| Variable | Group Ia (n=90) | Group IIb (n=90) | p-value |
|---|
| Mean duration of hospitalisation (Days) | 2.18±0.80 | 2.36±0.67 | 0.11 |
| Hematoma (n) |
| First day | 0 (0%) | 0 (0%) | 1 |
| Third day | 0 (0%) | 0 (0%) |
| 30th day | 0 (0%) | 0 (0%) |
| Seroma |
| First day | 0 (0%) | 0 (0%) | 1 |
| Third day | 0 (0%) | 0 (0%) |
| 30th day | 0 (0%) | 0 (0%) |
| Infection |
| First day | 0 (0%) | 0 (0%) | 1 |
| Third day | 0 (0%) | 0 (0%) |
| 30th day | 0 (0%) | 0 (0%) |
| Transient hypocalcaemia |
| First day | 16 (17.7%) | 19 (21.1%) | 1 |
| Third day | 0 (0%) | 0 (0%) |
| 30th day | 0 (0%) | 0 (0%) |
| Recurrent laryngeal nerve paralysis |
| First day | 0 (0%) | 0 (0%) | 1 |
| Third day | 0 (0%) | 0 (0%) |
| 30th day | 0 (0%) | 0 (0%) |
Discussion
The high incidence of thyroid diseases and the development of medical treatments, thyroid surgery is still one of the common operations and occurs for different reasons. Since, ancient times, different techniques have been used. It is tried to do thyroid surgery more accurately and with more subtlety. Various references and articles on uncomplicated thyroid surgeries, have not proved the benefits of inserting drain and they sometimes considered it harmful. Limited data suggested that drains may be benefit for selective surgeries [14,15]. The surgeons often use drains after thyroid surgery to prevent any clot formation at the site of surgery [3]. Use of drain is mostly based on a tradition than scientific evidences [16]. The main role of drain is prevention of postoperative complications and the evacuation of hematoma or any lymphatic discharge or bleeding after surgery [17]. However, it has been shown that the use of drain can be associated with an increased risk of infection [18,19]. In addition, in recent decade, surgical techniques for benign thyroid diseases has been greatly improved and the rate of mortality and post-operative complications have been dropped. Besides, the drainage in uncomplicated cases is very few and there is no need to do so. Therefore, the use of drain seems not to be necessary after thyroid surgeries, especially in uncomplicated cases.
Bleeding in the dead space around the trachea with the pressure on the airway can be life-threatening and requires emergency re-exploration [7]. Bleeding usually occurs between two to six hours after surgery [18,20]. The incidence of cervical hematoma after thyroidectomy is variable and occurs in approximately 0.3-5.5% of cases [15,18]. Risk of post-operative bleeding is more in patients with graves and retrosternal goiter [19]. In the study by Herranz J et al., it was suggested that the use of drain in patients with large dead space and retrosternal goiter is useful. Also, they suggest that routine use of drain after thyroid surgery is not effective [21]. Some studies have reported that due to a blood clot stuck in the drain, inserting drain after surgery is ineffective [22].
In some studies, it is noted that inserting drain causes the inflammatory processes and therefore, it is proposed that insertion of drain can increase liquid production [9]. Also, the negative pressure created as a result of drain suction can cause closed lymphatic tearing and thereby increase the fluid production and secretion [15,18]. Due to the improvements in surgical procedures and medications, post-operative life-threatening complications such as bleeding, hematoma and pressure on the airway can be prevented in most patients [7,22], and therefore, the value of using drain after thyroid surgery should be re-evaluated.
In the present study, no complications were observed in the study groups after surgery, such as hematoma, bleeding, seroma and damage to the laryngeal recurrent nerve. Also, Memon ZA et al., reported the results similar to those we presented, recommending that in uncomplicated surgeries, especially in thyroid lobectomy, using post-operative drain can be removed [23]. In study by Kalemera SE et al., only one patient in the group with drain suffered from post-operative infection, so the routine use of drain after thyroid surgery was not recommended [20].
In this study, duration of hospitalisation in the group without drain was less than the other group, but the difference was not significant. In some studies [15,20,23,24], duration of hospitalisation in the group without drain was significantly reported lower than group with drain. Short hospitalisation reduces the risk of nosocomial infections in patients. Since, the majority of patients have a low economic conditions, shorter length of stay in the hospital for them is more economical and saves financial resources. Patients also can return faster to their jobs. Despite the importance of this issue and its confirmation in many studies, almost half of surgeons still use drains after thyroid surgery [5].
Thyroidectomy-related hypocalcaemia is usually a transient finding. Its incidence has been reported between 5-50% in different studies [25,26]. The main point about total thyroidectomy is that patients should be monitored for a long time in terms of hypo-parathyroid injuries caused as a result of the surgery. The incidence of lasting hypocalcaemia as a result of total thyroidectomy is estimated about 2-5% [25]. As mentioned above, transient hypocalcaemia occurred more frequently in total thyroidectomy group than in lobectomy group. It can be concluded that the main factor contributing transient hypocalcaemia after surgery is likely the type of surgery. In patients who undergo total thyroidectomy, the possibility of transient hypocalcaemia is potentially more than patients undergoing lobectomy. Till to date, numerous studies have failed to identify the value of drain after thyroid routine surgery and drain have been considered unnecessary, however, these results may not be accepted directly in the clinical settings. In short, embedding drain is not required in most thyroidectomy cases. Drain can cause discomfort and pain, increase in duration of hospitalisation and infectious complications. It can be useful in patients with substernal goiter or in those receiving anticoagulant drugs.
Limitation
Regarding limitations of the present research, it should be stated that the study sample did not include the patients with retrosternal thyroid and further surveys are suggested on such cases, with larger sample sizes.
Conclusion
Our findings showed that lack of use of drains was not associated with any complications after thyroid surgeries, but also could reduce the patients discomfort. Use of drain may be recommended only in special cases of thyroidectomy surgery, such as substernal goiter, or in high-risk patients, such as cases with coagulation disorders.
a Group I consisted of subjects without drains
b Group II consisted of subjects with drains
* Body mass index