Primary Paraganglioma of the Thyroid Gland- A Rare Case Report
Manjot Gill1, Arnav Kr Roychoudhury2, Shaffy Thukral3, Anshul Gupta4, Nidhi Bansal5
1 Resident, Department of Pathology, Adesh Institute of Medical Science and Research, Bathinda, Punjab, India.
2 Assistant Professor, Department of Pathology, Adesh Institute of Medical Science and Research, Bathinda, Punjab, India.
3 Assistant Professor, Department of Pathology, Adesh Institute of Medical Science and Research, Bathinda, Punjab, India.
4 Assistant Professor, Department of Pathology, Adesh Institute of Medical Science and Research, Bathinda, Punjab, India.
5 Assistant Professor, Department of Immunohematology and Blood Transfusion, Guru Gobind Singh Medical College, Faridkot, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arnav KR Roychoudhury, Assistant Professor, Department of Pathology, Adesh Institute of Medical Sciences and Research, Barnala Road, NH 7, Bathinda-151101, Punjab, India.
E-mail: drarnav2007@gmail.com
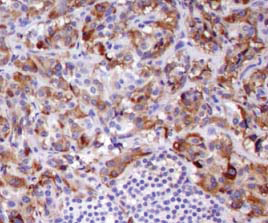
Paragangliomas are uncommon neoplasms that can arise in adrenal as well as in extra-adrenal paraganglia of the Autonomic Nervous System (ANS). Thyroid paraganglioma is a rare tumour that can be frequently mistaken for other thyroid neoplasms. Increased awareness is essential for avoiding diagnostic pitfalls regarding their characteristic features. We describe here a case of primary paraganglioma of thyroid gland. The neoplastic cells were strongly and diffusely immunoreactive with chromogranin. It showed a delicate S-100 protein positive supporting sustentacular framework. Level of calcitonin was also checked and found to be negative. We also reviewed the literature to summarize the characteristics of this distinctive lesion of thyroid gland. Though, a very rare paraganglioma, it should be included in the differential diagnosis of hypervascular thyroidal neoplasms. The gold standard of diagnosis relies on the histopathogical findings along with adjunctive immunohistochemical studies.
Chromogranin, Immunohistochemistry, Neuroendocrine
Case Report
We present a case of 40-year-old female who came with a neck swelling since three years. Haematological and biochemical investigations were within normal limits. Physical examination revealed a well circumscribed, firm solitary thyroid nodule in the right lobe of thyroid measuring 4 cm × 3 cm. The patient presented after three years because of the compressive symptoms and inability to breathe properly. There was no history of any thyroid problems in the past. There were no signs of hyper or hypothyroidism. Thyroid profile was done and was within normal limits. Fine Needle Aspiration Cytology (FNAC) was done two years back but the reports were unavailable.
Ultrasonography showed solitary heterogenous nodule measuring 4 cm × 3 cm with hypoechoic halo and intranodular vascular flow. Thyroid function tests were in normal range. Provisional diagnosis of neuroendocrine carcinoma and medullary carcinoma was kept in mind. Right hemithyroidectomy was done and the specimen was sent to the histopathology section in 10% formalin solution.
Gross examination revealed a globular soft tissue mass grey brown in colour measuring 4.5 cm in diameter. Cut section showed brownish fluid and multiple haemorrhagic areas [Table/Fig-1].
Gross showing well circumscribed nodule with areas of hemorrhage.

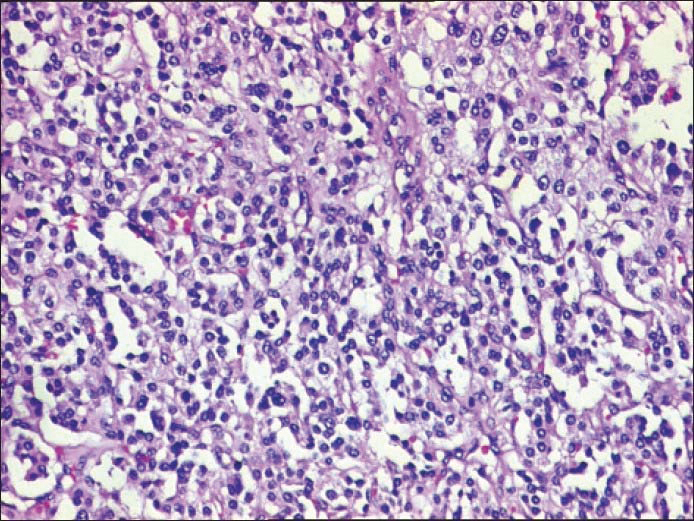
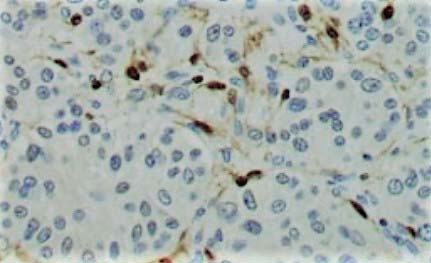
Histopathological examination showed tumor consisting of nests and sheets of tumour cells separated by fibrous septae (Zellballen pattern). These cells had round to oval nuclei, vesicular nuclear chromatin, inconspicuous nucleoli and moderate amount of eosinophilic granular cytoplasm. No significant pleomorphism and mitosis was identified. Pink eosinophilic amorphous material was also present [Table/Fig-2,3]. Histopathological diagnosis of primary paraganglioma of thyroid was given along with the differential diagnosis of medullary carcinoma of thyroid. Calcitonin, S-100, chromogranin and synaptophysin were advised to rule out all the differential diagnosis. S-100 and chromogranin [Table/Fig-4,5] were positive while calcitonin was negative and hence, the diagnosis of paraganglioma was given. Total thyroidectomy was done without any radical neck dissection. The patient could not be followed up further.
Tumor cells arranged in organoid pattern with adjacent normal thyroid gland follicles (H&E, 10X).
Tumour cells arranged in organoid pattern (H&E, 40X).
Delicate sustentacular positivity in the supporting tissues around the tumour cell nests (S-100, 40X).
Diffuse granular cytoplasmic positivity (Chromogranin, 40X).
Discussion
The most common site of extra-adrenal paraganglia are the head and neck region, superior mediastinum and retromediastinum [1,2]. Lattes [3] in 1950 proposed a classification of these neoplasms occurring in different sites. The most common sites were within the carotid body itself mainly carotid bifurcation, vagus nerve (ganglion nodosum), aortic arch bodies. These ganglionic structures are part of the parasympathetic nervous system. Since, these tumours resembled the paragangliomas of the sympathetic nervous system and were negative for chromaffin reaction, they were named suggestively as nonchromaffin paragangliomas. Pertinent to the discussion of paragangliomas of unusual locations are the papers by Tobin H and Harris HH [4]. The first reported case of paraganglioma in thyroid was described by Van Miert PJ [5] in 1964.
Paraganglioma is a neuroendocrine tumour that originates from the sympathetic paraganglia of the autonomic nervous system, which in turn is derived from ectodermal cells. Thyroid gland is derived from the cells of endodermal origin. Therefore, at present, the pathogenesis of thyroid paraganglioma remains unclear. Thyroid paraganglioma is generally slow growing and most patients present with an asymptomatic neck mass. Till date only 60 cases of primary paraganglioma of thyroid gland have been reported in the english literature [6-10].
The diagnostic criteria [11] in regard to malignancy in paraganglioma rely on the presence of metastasis, but no histopathological parameters to have been shown to predict clinical behaviour of the tumour. Few tumours may show atypical presentation but malignant transformation has not been described in thyroid yet.
The diagnosis of thyroid paraganglioma may be extremely difficult on a purely morphological basis. None of the reported cases have ever been diagnosed correctly preoperatively. Ultrasonography typically shows a solid hypoechoic nodule in thyroid gland. Computed Tomography (CT) scan shows a thyroid mass of low density usually being benign. Though, Fine Needle Aspiration Biopsy (FNAB) is considered to be highly sensitive and specific in cases of thyroid lesions, thyroid paragangliomas are rarely being diagnosed by FNAB. Immunohistochemistry is essential to show the difference from other types of tumours [9]. On immunohistochemistry, S-100 is highlighted in the sustentacular cells [Table/Fig-4]. Tumour cells show positivity for chromogranin [Table/Fig-5].
Due to architectural similarities, paragangliomas of thyroid gland are often misdiagnosed as other types of thyroid malignancies. Differential diagnosis includes two main entities, namely Medullary carcinoma and Hyalinizing Trabecular Tumour (HTT). Both the tumours (Medullary carcinoma and Paraganglioma) show similar structural patterns of nesting as well as organoid cell clusters. Neuroendocrine differentiation is also shown by both medullary carcinoma as well as paraganglioma thereby, increasing the difficulty in appropriate diagnosis. The differential diagnosis between benign and malignant paraganglioma is difficult and cellular criteria for malignancy have not been defined yet. The criteria for malignancy includes metastasis, necrosis, uniform cytological atypia and vascular invasion [5,7,12]. So, it becomes very essential to distinguish correctly between medullary carcinoma and paraganglioma. Presence of amyloid in the stroma and stained by congo red stain gives the diagnosis in favour of medullary carcinoma with confirmation by positive staining with calcitonin [5]. The other closest differential is HTT [10] of follicular cell origin. As the name suggests, the main feature is the presence of intratrabecular hyalinization in the tumour. By immunohistochemistry, HTT is positive for thyroglobulin and TTF1 with unique membranous expression of Ki-67.
Total thyroidectomy or thyroid lobectomy (if tumour is confined to a single thyroid lobe) are the preferred treatment options and generally can be considered to be curative. Elective neck dissection is not indicated [7,12,13].
The prognosis of primary thyroid paraganglioma appears to be favourable, provided that surgical excision is complete. Benign paragangliomas have a five year survival of 95%, while malignant paragangliomas are estimated to have a five year survival rate in 43.3% cases [14].
Conclusion
A high degree of suspicion, knowledge of the differential diagnoses and careful histomorphological study combined with judicious use of adjuvant immunohistochemistry are the key to an accurate early diagnosis of thyroid paraganglioma.
In conclusion, this case is presented for its rarity, thus highlighting the need to include primary paraganglioma of thyroid in the differential diagnosis of neuroendocrine intrathyroid tumours and hence, merits mention.
[1]. Lack EE, Cubilla AL, Woodruff JM, Paragangliomas of the head and neck region. A pathologic study of tumors from 71 patientsHum Pathol 1979 10(2):191-218. [Google Scholar]
[2]. Barnes L, Tse LLY, Hunt JL, Tumour of the paraganglionic system: introduction, In: Barnes L, Eveson JW, Reichart P, Sidransky D, edsWorld Health Organization classification of tumours: pathology and genetics of head and neck tumours 2005 9LyonIARC Press:362-63. [Google Scholar]
[3]. Gonzalez Poggioli N, Lopez Amado M, Yebra Pimentel MT, Paraganglioma of the Thyroid Gland: A Rare EntityEndocr Pathol 2009 20:62-65. [Google Scholar]
[4]. Tobin H, Harris HH, Non chromaffin paraganglioma of the larynx- case report and review of the literatureArch Otolaryngol 1972 96:154-57. [Google Scholar]
[5]. Van Miert PJ, The treatment of chemodectomas by radiotherapyProc R Soc Med 1964 57:946-51. [Google Scholar]
[6]. De Vries EJ, Watson CG, Paraganglioma of thyroidHead neck 1989 11(5):462-65. [Google Scholar]
[7]. Ferri E, Manconi R, Armato E, Iannielo F, Primary paraganglioma of thyroid gland: a clinicopathologic and immunohistochemical study with review of literatureActa Otorhinolaryngol Ital 2009 29(2):97-102. [Google Scholar]
[8]. Napolitano L, Francomano F, Angelucci D, Napolitano AM, Thyroid paraganglioma: report of a case and review of the literatureAnn Ital Chir 2000 71(4):511-13. [Google Scholar]
[9]. Yu BH, Sheng WQ, Wang J, Primary paraganglioma of thyroid gland: a clinicopathologic and immunohistochemical analysis of three cases with a review of literatureHead Neck Pathol 2013 7(4):373-80. [Google Scholar]
[10]. Yano Y, Nagahama M, Sugino K, Ito K, Kamayema K, Paraganglioma of thyroid: report of a male case with ultrasonographic imagings, cytologic, histologic and immunohistochemical featuresThyroid 2007 17(6):575-78. [Google Scholar]
[11]. Schmit GD, Gorman B, Van Heerden JA, Gharib H, Inferior laryngeal paraganglioma mimicking a primary thyroid tumorEndocr Pract 2006 12(24):432-35. [Google Scholar]
[12]. Kronz JD, Argani P, Udelsman R, Silverberg L, Westra WH, Paraganglioma of the thyroid: two cases that clarify and expand the clinical spectrumHead Neck 2000 22(6):621-25. [Google Scholar]
[13]. Brownlee RE, Shockley WW, Thyroid paragangliomaAnn Otol Rhinol Laryngol 1992 101(4):293-99. [Google Scholar]
[14]. Feng N, Zhang WY, Wu XT, Clinicopathological analysis of paraganglioma with literature reviewWorld J Gastroenterol 2009 15(24):3003-08. [Google Scholar]