Breast carcinoma is the leading cause of cancer deaths among women throughout the world [1]. The incidence of breast cancer is increasing alarmingly both in developed countries as well as in developing countries like India. Most of the breast lesions present with palpable swelling in the organ. As per current practice, FNAC is still the most relevant primary investigation for breast lesions along with mammography and the clinical examination to exclude cancer especially in developing countries [2]. However, cytological diagnosis is based on the subjective evaluation of nuclear features and thus, may raise a difficulty in establishing the precise diagnosis preoperatively. Benign and malignant lesions usually do not pose much problem in diagnosis by FNAC. However, difficulty arises in cases of premalignant lesions, carcinoma in situ and minimally invasive carcinoma. In fact, cytology has its own disadvantages due to its intraobserver and interobserver variability [3].
Morphometry is the quantitative description of the biological structure. Quantification of nuclear pleomorphism by measuring nuclear features such as area, perimeter, and diameter has been suggested to improve the clinical value of malignancy grading [3]. In the last few years, there have been some studies based on morphometry of benign and malignant cells of breast cytology specimens, which showed that it can improve sensitivity and specificity of diagnosis on FNAC. Especially nuclear image analysis can act as a strong tool for objective pathological analysis [4-6]. Thus, this study was done with aims to apply nuclear morphometry on cytological smears of breast aspirates and to evaluate its utility in differentiating benign and malignant lesions and to correlate it with histopathological features.
Materials and Methods
This was a retrospective study done in the Department of Pathology, RG Kar Medical College and Hospital in collaboration with Multi-disciplinary Research Unit of same Institute. Archived FNAC smears of Department of Pathology of cases of breast lump and diagnosed either as benign epithelial breast lesion or as breast carcinoma by routine microscopy of Leishman-Giemsa and PAP stained cytology and confirmed by histopathological report were included as samples. Poorly stained smears and cases without corresponding histopathology reports were excluded. A total of 108 samples were selected based on inclusion and exclusion criteria from archive of last two years (January 2015 to December 2016).
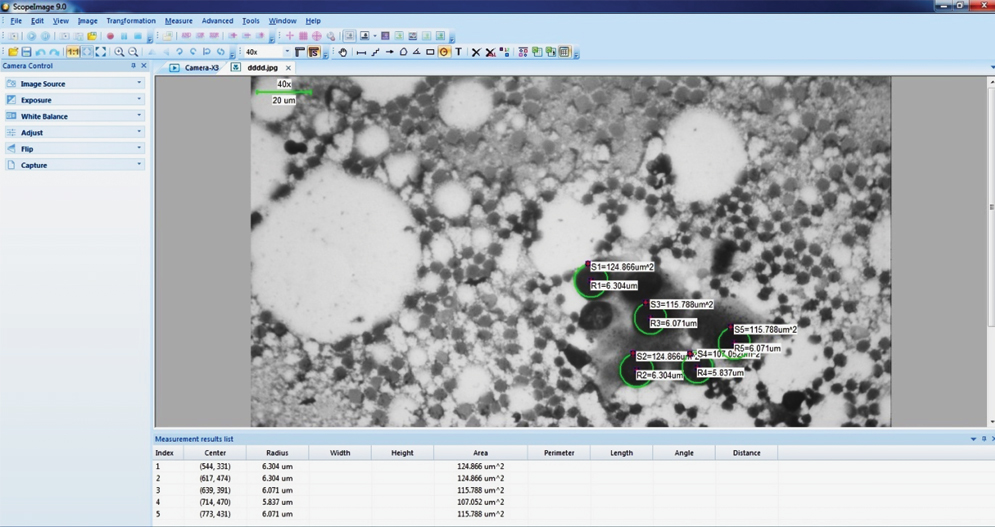
PAP-stained slides were examined under trinocular light microscope (Lawrence & Mayo LM-52-1802) with attached digital camera and computer system installed with imaging software in Multidisciplinary Research Unit. Nuclear morphometric analysis was performed on cytosmears using a computerised digital photomicrograph and imaging software (ScopeImage 9.0 software). The software system was properly auto-calibrated for each magnification and resolution. For each sample, one properly stained smear was chosen and on that smear, five high power fields (40X) were digitally captured and recorded [Table/Fig-1]. For evaluation of nuclear morphometric parameters, nuclei with non overlapping edges with one another were selected. Nuclear morphometric parameters were determined for 100 nuclei in each sample. Nuclei were analysed for following morphometric parameters- radius, perimeter and area. Data was transferred to MS-Excel sheet and mean of each parameter for each sample was calculated and recorded for further statistical analysis. Finally, mean and Standard Deviation (SD) was calculated for each of three study parameters for two groups-Malignant (Group A) and Benign (Group B) epithelial breast lesions.
Measurement of nuclear morphometric parameters by software system in a case of breast carcinoma.
Statistical Analysis
Statistical analysis for these two groups for each nuclear morphometric parameter was done by SPSS version 20.0 software. Unpaired t-test was done to evaluate the role of nuclear morphometric parameters to differentiate benign and malignant breast lesions (p-value <0.05 was considered as statistically significant).
Results
A total of 108 cases included under this study, 68 cases were of malignant epithelial lesions (Group A) and rest 40 cases were diagnosed as benign epithelial lesion of breast (Group B). The mean (±SD) age of malignant lesion was 56.8 (±8.3) years (range 39 years to 83 years) whereas for benign lesion, mean (±SD) age was 24.5 (±5.4) years (range 17 years to 38 years).
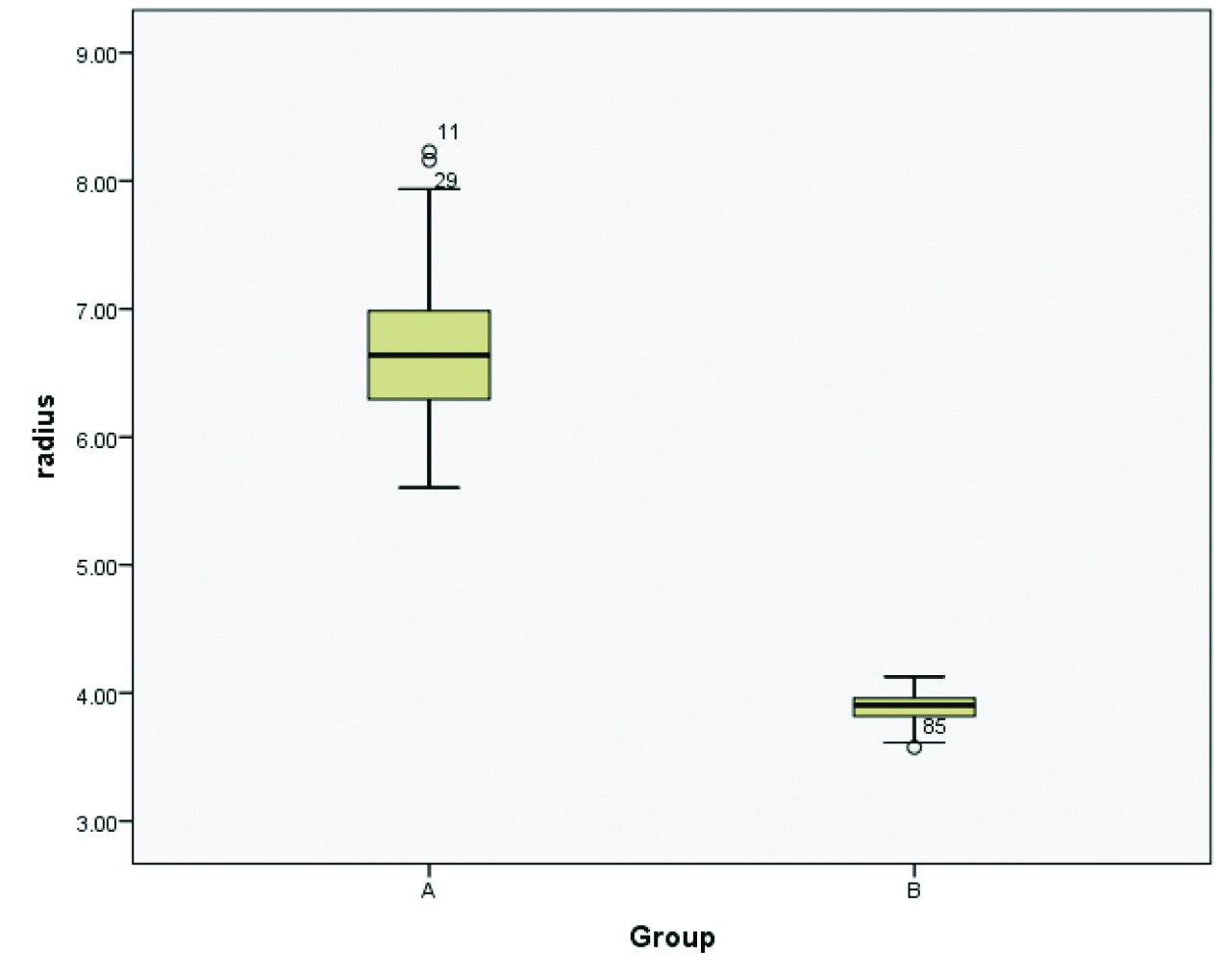
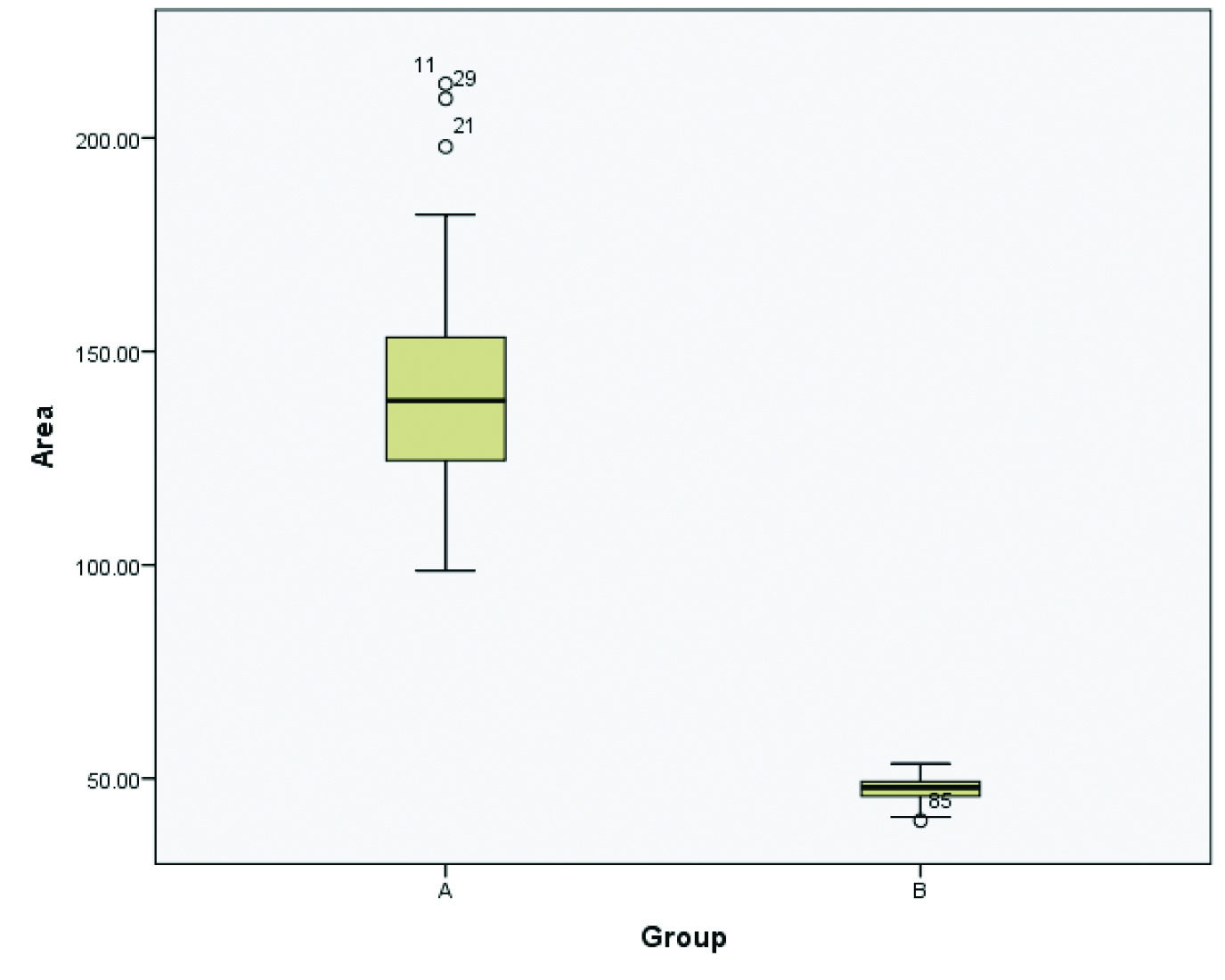
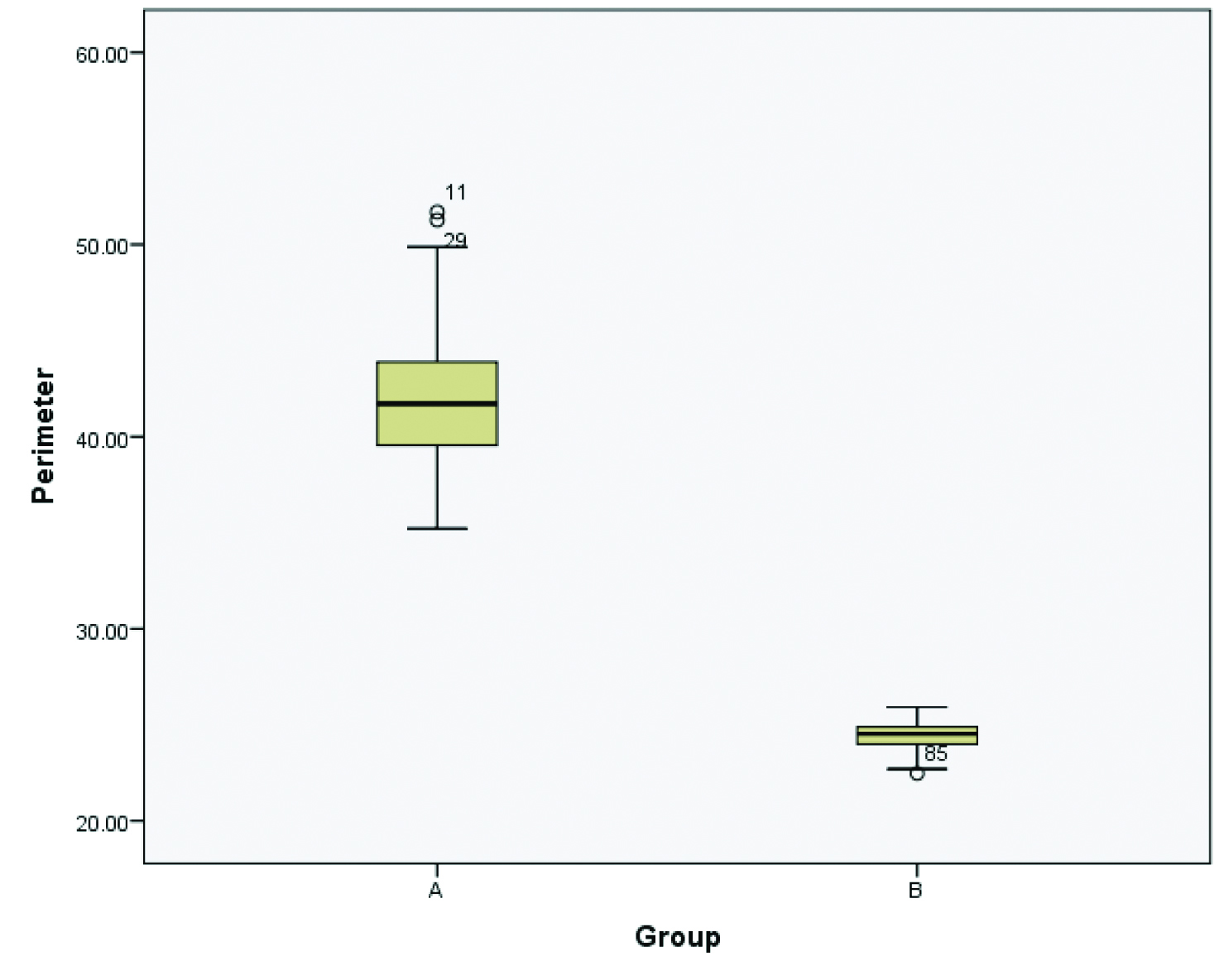
The results of statistical analysis for both the groups are presented by Box-plot diagram in the [Table/Fig-2,3 and 4]. The mean values along with SD of the nuclear morphometric parameters (radius, area and perimeter) for benign and malignant epithelial breast lesions are presented in [Table/Fig-5].
Box-plot diagram regarding nuclear radius showing mean and range for Group A as 6.67 μm and 5.60 μm to 8.22 μm while for Group B, they are 3.87 μm and 3.57 μm to 4.12 μm respectively.
Box-plot diagram regarding nuclear area showing mean and range for Group A as 140.75 μm2 and 98.66 μm2 to 212.65 μm2 while for Group B, they are 47.32 μm2 and 40.15 μm2 to 53.48 μm2 respectively.
Box-plot diagram regarding nuclear perimeter showing mean and range for Group A as 41.92 μm and 35.21 μm to 51.69 μm while for Group B, they are 24.36 μm and 22.46 μm to 25.92 μm respectively.
Comparison of different nuclear morphometric parameters in malignant and benign epithelial breast lesion using Unpaired t-test.
| Morphometric parameter | Malignant lesion (n=68)Group A | Benign lesion (n=40)Group B | p-value |
|---|
| Nuclear radius (μm)(Mean±SD*) | 6.67±0.531 | 3.87±0.145 | <0.001 |
| Nuclear perimeter (μm)(Mean±SD) | 41.92±3.33 | 24.36±0.916 | <0.001 |
| Nuclear area (μm2)(Mean±SD) | 140.75±22.94 | 47.32±3.53 | <0.001 |
*SD=Standard Deviation
Nuclear radius, perimeter and area were significantly higher in malignant lesions of breast tissue than benign epithelial lesions (p-value <0.001).
Discussion
In Indian women, breast cancer is becoming one of the most important causes of cancer related death and in addition to that, the incidence rate of breast cancer is also increasing recently [7].
Hence, timely and proper screening of all breast lumps is essential for early diagnosis and management. As per current protocol, in addition to clinical and radiological tests, FNAC is the first choice to evaluate such swellings as it is less invasive, simple and cost-effective than other modalities like Tru-cut biopsy especially in developing countries [2,8]. However, FNAC has few disadvantages as it is based on subjective visual evaluation of cellularity, chromatin pattern, nuclear-cytoplasmic ratio, cell morphology etc. To overcome these subjective biases, the role of morphology is being recently assessed by several researchers. Till now, majority of such morphometric image analysis have been performed on histopathological sections [9-14].
However, there are limited numbers of studies on nuclear morphometry of breast cytology smears [3-6,15-17]. In fact, nuclear morphometry can be better performed on cytology samples than histopathological sections as cells are better preserved and intact in cytology whereas in histopathological sections, during processing, fixation and cutting at various planes may produce some artefact [16].
On this background, this hospital based retrospective study has been performed to evaluate the role of nuclear morphometry in breast cytology.
Regarding age distribution of patients, this study has shown that average age of benign lesion (24.5 years) is lower than malignant lesion (56.8 years) which is similar to previous studies done by Kashyap A et al., where median age of benign (28.43 years) was lower than malignant cases (48.07 years) [16].
This study has clearly proved that all the three nuclear morphometric parameters (radius, perimeter and area) are significantly higher in malignant epithelial breast lesions in comparison to benign epithelial breast lesions. Kashyap A et al., found that mean nuclear area in benign and malignant cases were 25.49 μm2 and 51.43 μm2 respectively whereas mean nuclear perimeter were 18.39 μm and 25.69 μm respectively [16]. In another study, Narasimha A et al., showed that mean nuclear area for fibroadenoma cases and carcinoma cases were 71.6 μm2 and 117.33 μm2 respectively while mean nuclear perimeter were 29.95 μm and 40.87 μm respectively [6]. Regarding mean nuclear radius, they found 4.7 μm for benign cases and 6.02 μm for carcinoma cases. Laishram S and Shariff S obtained mean nuclear area as 18.59 μm2 in benign category while 39.59 μm2 in malignant category [17]. Yadav H et al., also revealed a progressive and significant increase in values of morphometric parameters from benign to borderline to malignant cases of breast lesions [18]. In present study, the mean nuclear radius, perimeter and area were 3.87 μm, 24.36 μm and 47.32 μm2 for benign cases respectively whereas 6.67 μm, 41.92 μm and 140.75 μm2 for malignant cases respectively. Though all the studies have established that these morphometric parameters are significantly higher in malignant cases, the mean values of the parameters are quite different in these studies. These discrepancies might be due to several factors like degree of fixation and its effect like cell shrinkage, methods of staining, ethnicity, aggressiveness, grade and stage of tumours etc. Regarding this, Yadav H et al., commented that these differences in observed values might be due to application of different morphometric methods in those studies [18]. The current studies only prove that the morphometric parameters are significantly different in benign and malignant epithelial breast lesions. However, prospective studies and meta-analysis with larger sample size and strictly standardised, uniform technique along with regular calibration of computerised morphometric software are required to increase the precision and accuracy which is essential for deciding a cutoff value of these morphometric parameters to differentiate between benign and malignant cases.
Limitation
There are certain limitations to this study. First of all, this was a retrospective study with archived slides and hence blinding could not be performed regarding FNAC and histopathology diagnosis. Secondly, reports of other modes of advanced investigations in breast lump cases like mammography and/or Ultrasonography (USG) were not available. Hence correlation with such parameters could not be done in this study. Lastly, correlations with histopathological staging and grading were not done with morphometric parameters in cytology smears.
Conclusion
This study has established that nuclear morphometric parameters like radius, perimeter and area are significantly higher in malignant epithelial breast lesions in comparison to benign epithelial breast lesions. Thus, these parameters can be utilised as an objective tool to assess breast cytology smears in adjunct to other subjective features. However, further studies with larger sample size are required to establish generalised cutoff values of these nuclear morphometric parameters to differentiate between benign and malignant lesions especially in grey zone areas.
*SD=Standard Deviation