Actinomyces is anaerobic, gram-positive bacilli that superficially resemble fungi and give rise to suppurative and granulomatous infection. The organisms are commensals to human body but under suitable conditions can involve any organ system. Cervicofacial actinomycosis is the most common presentation while actinomycosis of extremity especially calcaneum is very rare. We report a rare case of 40-year-old woman who presented with chief complaints of pain and swelling of the right foot for one year. She was diagnosed with isolated calcaneal actinomycosis and was managed by antibiotics, curettage of calcaneum and triple arthrodesis.
Case Report
A 40-year-old woman from rural Maharashtra presented with chief complaints of pain and swelling of the right foot for one year. There was no history suggestive of recent or past trauma, fever, loss of weight, anorexia, other joint involvement, underlying systemic disease or being immunocompromised. Consent for examination, investigation and subsequent management was taken from the patient. Clinical examination revealed a 2x2 cm swelling on the dorsolateral aspect and similar two swellings medially in hindfoot region [Table/Fig-1a]. There was mild local rise of temperature and a slight tenderness at subtalar joint. There was no regional lymphadenopathy. Ankle joint movements were normal while subtalar joint movements were painful and restricted.
a) Swelling on the medial aspect of foot and heel; b) Preoperative X-ray of calcaneum (lateral view) showing ostelytic lesions and sclerosis; c) Axial CT scan showing calcaneum with multiple osteolytic lesions (arrow); d) H&E stain of sample showing basophilic actinomyces colonies in the central haematoxylin-stained area (arrow) and dense inflammatory infiltrate composed of neutrophils, lymphocytes, plasma cells; e) Specimen of the granules taken out during the surgery (2 mm-2.5 cm); f) Postoperative X-ray showing curettage and triple arthrodesis.
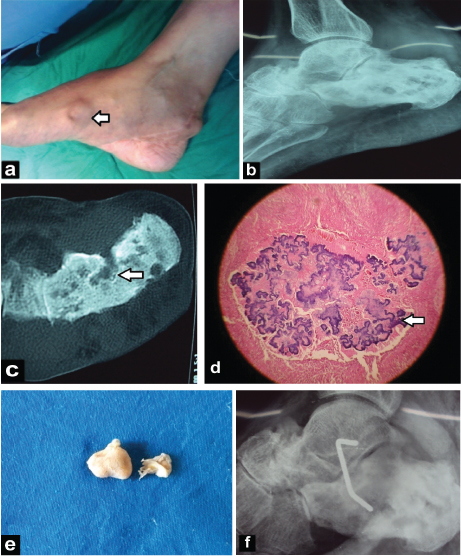
Radiography revealed soft tissue swelling around the ankle, osteopenia of underlying bones, sclerosis of calcaneum along with multiple osteolytic lesions in calcaneum [Table/Fig-1b]. Additional findings like narrowing of calcaneocuboid joint space were revealed on subsequent CT scan [Table/Fig-1c]. The possible radiological differential diagnosis entertained were chronic pyogenic osteomyelitis of calcaneum, Tuberculosis calcaneum and mycetoma (bacterial/fungal). Aspirate from the medial hindfoot swelling was subjected to histopathology and culture. On H&E stain, basophilic Actinomyces colonies were seen in the central haematoxylin-stained area surrounded by fibrocollagenous tissue, dense infiltrate of neutrophils, lymphocytes, plasma cells and occasional giant cells [Table/Fig-1d]. Simultaneously part of aspirate sent for anaerobic culture revealed A israelii as the causative organism. Culture of the aspirate on blood agar revealed Staph aureus as copathogen.
Tissue specimen removed at surgery comprised of necrotic bone debris and sulphur granules of variable size. Analysis of tissue specimen removed at surgery which consisted of necrotic bone debris and sulfur granules of varying size (2 mm to 2.5 cm) confirmed the diagnosis [Table/Fig-1e]. Patient was managed by thorough debridement of calcaneum and triple arthrodesis (Ollier’s approach) [Table/Fig-1f]. Postoperatively patient was managed by below knee cast for weeks. The response to penicillin therapy, curettage and triple arthrodesis was satisfactory in the patient. Regular follow ups were conducted at monthly interval. Patient was disease free at one year follow up without any reactivation or recurrence.
Discussion
Actinomycosis can present in various clinical forms e.g., cervicofacial, thoracoabdominal and pelvic, the latter being common in females. Actinomyces is normal flora of oral cavity and gastrointestinal tract. Primary actinomycosis of an extremity is very uncommon because of the endogenous habitat of the organism [1]. Haematogenous spread from some other primary site or direct extension following a mucosal breech are the possible mechanisms [1]. Males are more commonly affected than females (3:1) [1].
Few studies from literature have reported actinomycosis of the metacarpal bone [2,3], forefoot [1,4], lower leg [5] and calcaneum [6]. Lack of information among clinicians and population regarding disease aetiology, presentation and progression frequently leads to a delayed diagnosis and a late initiation of treatment [7].
Primary actinomycosis, mycetoma (actinomycetoma and eumycetoma) and chronic pyogenic osteomyelitis of calcaneum superficially resemble each other in their clinical presentation. But difference in causative organisms and sensitivity to different chemotherapeutic agents makes them discreet clinical entities. Causative organisms of actinomycosis are A israelii and related anerobic or facultative bacteria, while, actinomycetoma and Eumycetoma are caused by Nocardia spp. and Fungi respectively. S. aureus is the most common causative organism for pyogenic chronic osteomyelitis [8,9].
Primary actinomycosis involving extremity is very rare. Reiner SL et al., reported 36 cases of primary actinomycosis of extremity worldwide. Two more cases were reported with last case being reported in 1996 [6,10-12]. The present case of primary actinomycosis calcaneum being reported from India is one more addition to it. On the contrary mycetoma foot is quite common in India [13,14]; while incidence of 11% has been noted for chronic pyogenic osteomyelitis of calcaneum [15].
Mycetoma foot and ankle is worldwide in distribution with higher prevalence in geographic area between 15°S and 30°N also known as the mycetoma belt. But no racial and geographical predilection has been noted for actinomycosis calcaneum caused by A israeli. The latter affects people with middle age who have A israeli as part of their flora [6,13,14] The present case was a 40-year-old female from rural Maharashtra, India.
Pyogenic osteomyelitis of calcaneum may present with history of hindfoot surgeries, scars and signs of infection like reddening of the skin, hindfoot pain, oedema and toe walking [16]. Actinomycosis of extremity may present with history of trauma to extremity, immunocompromise or predisposing factors like rural background, poverty, malnutrition, poor oral hygiene, agricultural occupation and bare foot walking [1]. In case of actinomycosis of foot or calcaneum there is swelling, induration, multiple sinuses and exudate containing granules. Chronic infection and progressive destruction are hallmark of the disease. As pain and inflammatory signs are absent, so the individual keeps walking on a diseased limb leading to further destruction. Mycetoma is a relatively painless condition with possibility of a high incidence of secondary bacterial infection, deformities and recurrences of the affected foot.
In present case, calcaneum was affected by actinomycosis, a rarely reported presentation in literature. Patient had swelling on the dorsolateral aspect and similar two swellings medially in hindfoot region. There was mild local rise of temperature and a slight tenderness at subtalar joint. There was no regional lymphadenopathy. In another similar case presentation of calcaneal actinomycosis in the form of hindfoot swelling, moderately discoloured hyperpigmented skin on the lateral aspect of right heel, with two non draining sinuses and painful subtalar movements was noted [6]. Histopathology and culture is cornerstone to establish diagnosis. Material exuded in discharge from sinus or core needle biopsy from the site of pathology, is subjected to histopathology and culture to arrive at a diagnosis [6]. Colour of granules is helpful as white granules indicate actinomycosis, white to yellow granules actinomycotic mycetoma, while mycotic mycetomas have black granules. Gram-positive branching bacilli in tissue exudates or on culture confirm the diagnosis [17]. Actinomycotic infection can occur in isolation but most of the times it is a polymicrobial infection with multiple organisms being cultured in as many as 99% of cases of actinomycosis [2]. If any surgical debridement is planned, the tissue removed at the time of surgery can be re-examined by histopathology and culture to reach a conclusion [6]. Achieving a specific diagnosis is important as actinomycosis and Mycetoma are sensitive to different antibiotic treatments.
Molecular identification by 16S PCR aids in Actinomyces species identification [16]. In present study also it was a mixed infection with methicillin sensitive S aureus and A israelii being isolated on culture.
On pathological examination of specimen, bones are found riddled with spheroidal defects with sclerosis and periosteal reaction at periphery. In advanced stage, gross destruction and disorganisation of underlying bones is the norm. Radiography reflects the pathological changes showing circular lytic lesions and a sclerotic margin. Possible radiological differential diagnosis are multiple myeloma (punched out lesions without sclerosis) and fungal osteomyelitis (“fronts of resorption” and penetrating spicules) [18]. Osteopenia of underlying bones and multiple lytic lesions in calcaneum were noted in present study.
Since, infected and indurated tissues are avascular, surgical debridement along with high dose of antibiotics for prolonged period (6-12 months) are mandatory [19]. Penicillins are drug of choice for actinomycosis followed by other antibiotics like erythromycin, tetracycline, clindamycin, cephalosporins, meropenem, and chloramphenicol [20], while Nocardia are known to respond to Trimethoprim-sulfamethoxazole, amikacin and linezolid.
Antifungal agents like ketoconazole, miconazole and amphotericin B are used to treat fungal mycosis. Frequent co-infections with other microbes make combination therapy advisable.
In actinomycosis calcaneum, appropriate antibiotics and surgical management in the form of curettage of lesions or partial/complete calcanectomy is opted; depending upon the extent of disease. Limited disease in calcaneum can be managed by antibiotics, local curettage and debridement of the lesion while, large extent of disease with multiple sinuses is managed by partial/total calcanectomy. Literature findings mention partial and total calcanectomy as a mode of treatment for chronic osteomyelitis of calcaneum with non healing ulcer and refractory chronic osteomyelitis [21]. Surgical procedure in the form of debridement, curettage and triple arthrodesis was used in present study while another study from literature has reported management with total calcanectomy [6].
Conclusion
This case report highlights the importance of actinomycosis as a rare but important cause of chronic osteomyelitis of calcaneum. The diagnosis is likely to be missed for more common conditions with sinuses e.g., chronic bacterial and granulomatous conditions like tuberculosis. A close interaction between clinician, pathologist and microbiologist can help achieve accurate diagnosis.
[1]. Bettesworth J, Gill K, Shah J, Primary actinomycosis of the foot: a case report and literature reviewThe Journal of the American College of Certified Wound Specialists 2009 1(3):95-100. [Google Scholar]
[2]. Blinkhorn RJ, Strimbu V, Effron D, Spagnuolo PJ, ‘Punch’ actinomycosis causing osteomyelitis of the handArch Intern Med 1988 148(12):2668-70. [Google Scholar]
[3]. Mendelsohn BG, Actinomycosis of a metacarpal bone: Report of a caseThe Journal Of Boneand Joint Surgery 1965 47:739-42. [Google Scholar]
[4]. Golsha R, Najafi L, Rezaei-Shirazi R, Vakilinejhad M, Mortazavi B, Roshandel G, Actinomycosis may be presented in unusual organs: a report of two casesJ Clin Diagn Res 2009 3:1938-41. [Google Scholar]
[5]. Vandevelde AG, Jenkins SG, Hardy PR, Sclerosing Osteomyelitis and Actinomyces naeslundii infection of surrounding tissueClin Infect Dis 1995 20:1037-39. [Google Scholar]
[6]. Atwaru RM, Rasool MN, Nelson R, Actinomycosis of the calcaneus – a case reportSA Orthopaedic Journal 2009 8(2):59-62. [Google Scholar]
[7]. Ahmed AA, Van de Sande WW, Fahal A, Bakker-Woudenberg I, Verbrugh H, van Belkum A, Management of mycetoma: major challenge in tropical mycoses with limited international recognitionCurr Opin Infect Dis 2007 20:146-51. [Google Scholar]
[8]. Sankhe A, Bava JS, Patil S, Kale K, Rare case of mycetoma foot without any discharging sinuses: a case reportInternational Journal of Science and Research 2016 5(2):521-24. [Google Scholar]
[9]. Hatzenbuehler J, Pulling TJ, Diagnosis and management of osteomyelitisAm Fam Physician 2011 84(9):1027-33. [Google Scholar]
[10]. Reiner SL, Harrelson JM, Miller SE, Hill GB, Gallis HA, Primary actinomycosis of an extremity: a case report and reviewRev Infect Dis 1987 9(3):581-89. [Google Scholar]
[11]. Pang DK, Abdalla M, Osteomyelitis of the foot due to Actinomyces meyeri: a case reportFoot Ankle 1987 8(3):169-71. [Google Scholar]
[12]. Vogen KW, Actinomycosis of the footJ Am Podiatr Med Assoc 1996 86(5):238-40. [Google Scholar]
[13]. Bakshi R, Mathur DR, Incidence and changing pattern of mycetoma in western RajasthanIndian Journal of Pathology and Microbiology 2008 51(1):154-55. [Google Scholar]
[14]. Venugopal TV, Venogopal PV, Actinomadura madurae causing mycetoma in MadrasIndian J Pathal Microbial 1991 34:119-25. [Google Scholar]
[15]. Schildhauer TA, Bauer TW, Josten C, Muhr G, Open reduction and augmentation of internal fixation with an injectable skeletal cement for the treatment of complex calcaneal fracturesJ Orthop Trauma 2000 14(5):309-17. [Google Scholar]
[16]. Chen K, Balloch R, Management of calcaneal osteomyelitisClin Podiatr Med Surg 2010 27(3):417-29. [Google Scholar]
[17]. Brown JR, Human actinomycosis. A study of 181 subjectsHum Pathol 1973 4:319-30. [Google Scholar]
[18]. Rothschild B, Naples V, Barbian L, Bone manifestations of actinomycosisAnnals of Diagnostic Pathology 2006 10(1):01-66. [Google Scholar]
[19]. Sudhakar SS, Ross JJ, Short-term treatment of actinomycosis: two cases and a reviewClin Infect Dis 2004 38(3):444-47. [Google Scholar]
[20]. Choi J, Koh WJ, Kim TS, Lee KS, Han J, Kim H, Optimal duration of IV and oral antibiotics in the treatment of thoracic actinomycosisChest 2005 128:2211-17. [Google Scholar]
[21]. Woll TS, Beals RK, Partial calcanectomy for the treatment of osteomyelitis of the calcaneusFoot and Ankle 1991 12(1):31-34. [Google Scholar]