In medicine for any disease, common differentials should be thought first but in cases of recurrent and resistant infections where desired result is not achieved with protocol and evidence based management, other rare causes should come into our minds. In this case, after extensive academic review, we ultimately reached to a very rare diagnosis of idiopathic CD4+ deficiency. So, in cases of chronic and recurrent resistant to treat infections, besides known causes of secondary immunodeficiency, idiopathic CD4+ deficiency should also be kept in mind. While labelling it idiopathic today, it should be realised that before 1992, CD4+ deficiency associated with HIV was also thought to be idiopathic. Here we describe a case, which started as a routine case of tubercular lymphadenitis but had a rare underlying aetiology.
Cytomegalovirus, Human immunodeficiency virus, Infection, Lymphoma
Case Report
A 35-year-old female, resident of Sonipat, Haryana, India and mother of a nine-year-old healthy child and with no known prior comorbidities presented to our institute with complaints of fever, weight loss and mucocutaneous ulcers in May 2016. She was apparently well till July 2015, when she started having intermittent low-grade fever, anorexia, occasional non-productive cough and weight loss of around 10 kilograms over a period of six months. Her haemogram, liver and kidney function tests were normal other than low albumin value of 1.9 gm/dL. Contrast Enhanced Computed Tomography (CECT) chest and abdomen showed right middle zone consolidation, hypodense lesions in liver and spleen and a necrotic external iliac lymph node. Biopsy of necrotic lymph node was done and it revealed necrotising granulomas. So, Cat I ATT (Anti Tuberculosis Treatment) was started for Tuberculosis in December 2015. She gradually improved over the next 2 months, but later developed jaundice, anorexia and vomiting. With the suspicion of drug induced hepatitis (ATT induced), ATT had been modified to ethambutol, levofloxacin and streptomycin. After taking modified ATT for over 1 week, she developed mucocutaneous lesions over lips, oral cavity and tongue [Table/Fig-1]. So, ATT was stopped in suspicion of drug induced eruptions for over 20 days with no improvement. ATT was again re-introduced and maintenance phase was continued. In the month of May’ 2016 (almost after 9 months of illness), she had a massive upper GI bleed with haematemesis and malena. Upper GI endoscopy revealed oesophageal ulcers in mid and lower oesophagus for which sclerotherapy was done and she was referred to our hospital for further evaluation. On examination, she was conscious and oriented, ill-nourished with crusting mucocutaneous lesions on lips, oral cavity and tongue. There was pallor with liver palpable 2 cm below costal margin and mildly enlarged non- tender spleen. Cardio-respiratory and nervous system examination was unremarkable. Initial blood investigations showed anaemia, leucocytopenia and hypoalbuminemia. At this point, we had differential diagnosis of either disseminated infection like tuberculosis or viral infection like Herpes Simplex Virus (HSV), Cytomegalo Virus (CMV) (in view of the mucocutaneous involvement), malignancy like a lymphoma or autoimmune disease like Systemic Lupus Erythematosus (SLE). Peripheral smear showed anisopoikilocytosis with microcytic hypochromic anaemia and leukopenia. Bone marrow aspirate and biopsy were negative for any infection or malignancy. Serum ferritin, vitamin B12, folate levels were normal and viral markers as well as autoimmune work up were negative. In the meantime, on the eighth day of her admission, she started complaining of painless decreased vision in her right eye.
Perioral mucocutaneous lesions.

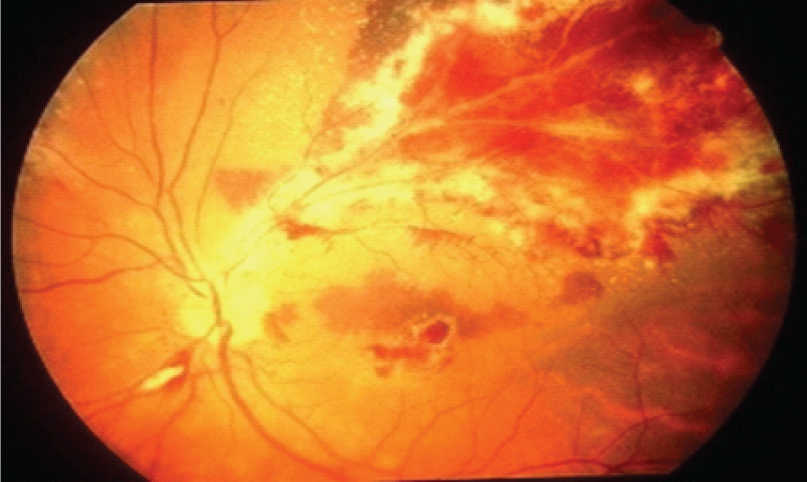
Fundoscopy showed peripapillary exudates and haemorrhages suggestive of CMV retinitis [Table/Fig-2]. CMV PP65 antigen were positive and she was started on systemic and intravitreal Ganciclovir. She improved dramatically and her mucocutaneous lesions resolved within a week, though there was only a slight improvement in her vision.
Peripapillary exudates with disc oedema.
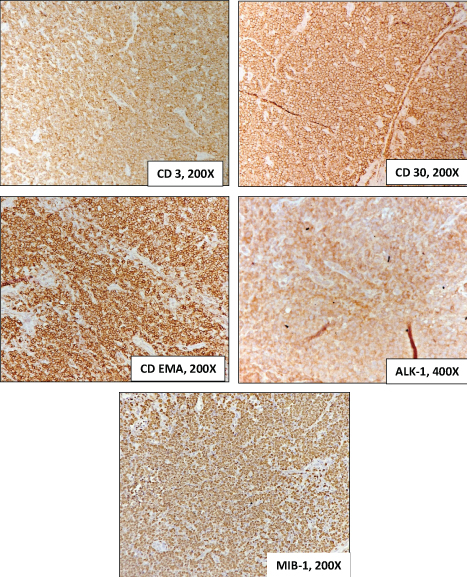
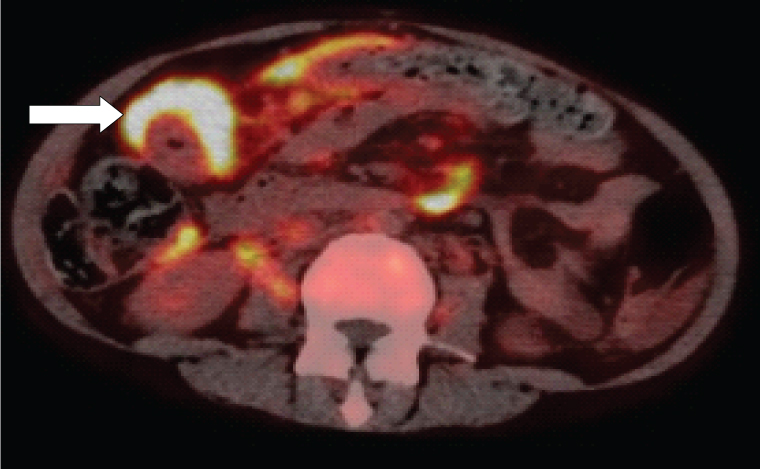
In view of CMV, to rule out immune deficient state HIV ELISA as well as RNA PCR were done and both were negative. Her workup for primary immunodeficiency revealed an absolute CD4+ value of 17 cells/mm3 (normal value 500-1500cells/mm3) with reduced CD4:CD8 ratio of 0.14 (Normal value being >1) with a normal CD3(T cell marker) value [Table/Fig-3]. Serum immunoglobulin levels and DHR (dihydrorhodamine) for Chronic Granulomatous Disease (CGD) were normal. To rule out causes which can cause transient CD4 lymphopenia, adenovirus, Epstein-Barr Virus (EBV) PCR and Cryptococcus antigen test were done and they were negative. So, with the diagnosis of isolated (probably idiopathic) CD4+ lymphocytopenia we discharged her with advice to follow up in the OPD. Her general condition improved and she gained over 8 kg weight in her follow up visit after 2 months. Six-month course of ATT was completed later and CECT abdomen showed resolution of necrotic lymph nodes. Three months later (after completion of ATT), she was readmitted with complaints of epigastric lump with recurrent vomitings and cervical lymphadenopathy. Biopsy from the mass revealed T cell lymphoma with ALK positivity [Table/Fig-4,5]. Positron Emission Tomography-Computed Tomography (PET-CT) showed uptake in multiple abdominal lymph nodes and also in stomach and duodenal wall [Table/Fig-6]. She was started on chemotherapy with cyclophosphamide along with steroids and is now planned for further cycles of chemotherapy.
Comparison of CD4 count and other T cell CD markers throughout the clinical course of illness.
| T cell markers | During 1st admission (May’16) | During follow up (Aug’16) | During 2nd admission (Sep’16) |
|---|
| Absolute lymphocyte count (cells/mm3) | 587 | 136 | 730 |
| Absolute CD4 count (cells/mm3) (500-1500) | 17 | 12 | 10 |
| CD3% of patient (control) | 66.7% (87.9) | 78.13% (59-83) | 15.8% (67.9) |
| CD4% of patient (Control) | 9.19% (79.4) | 9% (31-59) | 9.86% (53.7) |
| CD8% of patient (Control) | 65.1% (17.8) | 68.5% (12-38) | 81.8% (39.8) |
| CD4:CD8 ratio | 0.14 (4.46) | 0.13 (>1) | 0.12 (>1) |
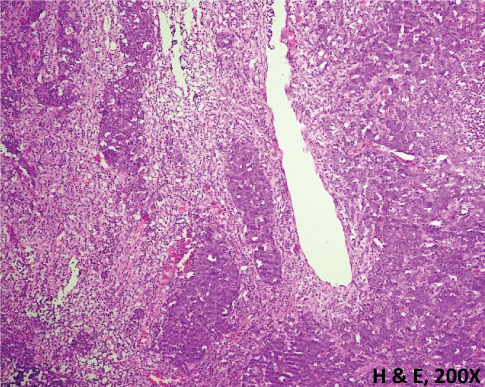
Biopsy from the epigastric mass revealing lymphoid cells.
Staining of the histological specimen with CD3, CD30, CD EMA, ALK-1 and MIB-1, suggestive of Anaplastic large cell lymphoma.
Concentric thickening with increased FDG uptake (white arrow) involving pyloric end of stomach, duodenum.
Discussion
Idiopathic CD4+ Lymphocytopenia (ICL) is a rare syndrome defined by persistent low CD4+ T cell count in the absence of other causes of immunodeficiency. Thus, it’s a diagnosis of exclusion. Infections that need to be ruled out include an exhaustive list, all of which can cause CD4+ lymphopenia. A few include, HIV-1, HIV-2, tuberculosis, hepatitis B and C, EBV, HHV-6, CMV, RSV, parainfluenza virus, enterovirus, adenovirus, parvovirus B19, corona virus, and congenital rubella, HPV, HTLV, disseminated fungal infections.
It is defined as persistent CD4+ T cell lymphopenia in the absence of infection with HIV-1 or any other cause of immunodeficiency. CD4+T cell lymphopenia is considered when CD4+ count is below 300 cells/μL or < 20 % of total lymphocytes on two different point of time with a gap of 2 or 3 months apart [1]. It was first described in 1992, in the beginning of HIV epidemic in a group of patients of CD4+ lymphopenia who were suspected to be having HIV infection, but they neither had HIV nor any other alternative aetiologic agent [2]. CD4 cells are helper T cells which are involved in the protection against viruses, fungus, autoimmunity, and cancers. They usually comprise 60-70% of T cells but in our patient, it was only about 9%. CD4:CD8 ratio usually describes the balance of the immune system and is normally 0.9-1.9. In retrovirus positive patients and ICL patients along with the CD4 count, CD4:CD8 ratio also drops to less than 1 [2].
In our patient [Table/Fig-3] this ratio was around 0.13. CD3 count, a pan marker of T cells was normal in our case except in the later phase of the disease probably due to development of T cell lymphoma.
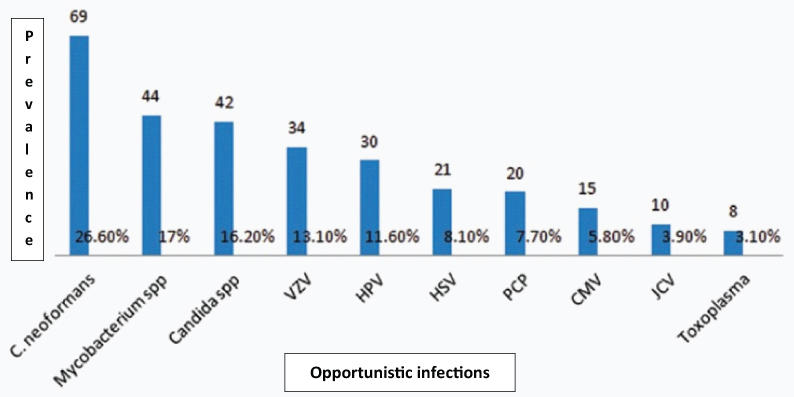
It typically presents with opportunistic infections (88%), malignancies (18%), or autoimmune disorders (14%) [2]. The different opportunistic infections, autoimmune diseases and malignancy in ICL are as described in [Table/Fig-7] [2].
Different opportunistic infections in ICL.
Autoimmune diseases associated with ICL:
Sjögren’s disease
Sarcoidosis
Psoriasis
Autoimmune haemolytic anaemia
ITP
SLE
Vasculitis
Malignancy in ICL:
Squamous cell carcinoma
Basal cell carcinoma
Kaposi’s sarcoma
Lymphoma
Leukaemia
Bladder tumour
Cervical intraepithelial tumour
It has been observed in the natural history of few lymphomas that the CD4+ count falls long before the clinical detection of the disease [3]. Patients with idiopathic CD4+ lymphocytopenia are more prone to malignancy especially T cell lymphomas (Anaplastic large cell lymphoma in our patient). But there can still be a possibility that T cell lymphoma might have caused CD4+ lymphopenia in this patient. As of now we are waiting to see if patient’s CD4 count remains the same or improves, after treatment of the lymphoma to decide whether CD4+ lymphocytopenia might have caused lymphoma or vice-versa. The fact that CD4+ count did not improve after adequate treatment of tuberculosis and CMV suggests that, they are unlikely to contribute to low CD4 counts.
Standard treatment protocol for ICL is still not available except for management of treatable associated infections or malignancy.
There is no standard treatment protocol for management or follow up of patients with ICL. Management consists of mainly treatment of opportunistic infections and various malignancies associated with ICL. Measurement of CD4 subsets twice yearly is to be done [4]. Prophylaxis for opportunistic infections should be given for patients with ICL and CD4 counts <200. Therapies to increase CD4 cell counts like IL-2 agonists (aldesleukin) have been tried with limited success [4]. A small number of patients with severe manifestations of ICL have been treated with haematopoietic cell transplantation. [5].
Conclusion
The presence of lymphoma in our patient, along with laboratory and pathological findings suggest that there might be some underlying aetiology (i.e., ICL here) that might have led to all these opportunistic infections. ICL is a rare entity that needs a high index of clinical suspicion for diagnosis and must be suspected in any patient presenting with low CD4+ count and HIV negative. A thorough evaluation for factors causing CD4+ lymphocytopenia should be done. Treatment of ICL patients may be very challenging.
Idiopathic CD4 lymphocytopenia challenges us not only with its cause, but also with its heterogeneous natural history; as evidenced by some patient having benign course while other subset is being doomed to a rapid deterioration. So, while understanding, diagnosing and treating patients with this entity which is AIDS like and yet very different, let us keep a hawk’s eye on this disease which might in the future turn out to be not an idiopathic condition, following the progress in immunology and virology.
[1]. Centers for Disease Control (CDC)Unexplained CD4+ T-lymphocyte depletion in persons without evident HIV infectionMortal Wkly Rep 1992 41(30):541-45. [Google Scholar]
[2]. Ahmad DS, Esmadi M, Steinmann WC, Idiopathic CD4 lymphocytopeniaAvicenna J Med 2013 3(2):37-47. [Google Scholar]
[3]. Gupta RK, Marks M, Edwards SG, Smith K, Fletcher K, Lee S-M, Declining CD4 count and diagnosis of HIV-associated Hodgkin lymphoma: do prior clinical symptoms and laboratory abnormalities aid diagnosis?PLoS One 2014 9(2):e87442 [Google Scholar]
[4]. Zonios DI, Idiopathic CD4+ lymphocytopenia: natural history and prognostic factorsBlood 2008 112(2):287 [Google Scholar]
[5]. Cervera C, Non-myeloablative hematopoietic stem cell transplantation in the treatment of severe idiopathic CD4+ lymphocytopeniaEur J Haematol 2011 87(1):87-91. [Google Scholar]