Co-existence of Wuchereria bancrofti Microfilaraemia in a Case of Multiple Myeloma: An Incidental Finding or an Association?
Sonam Sharma1, Rahul Mannan2, Rachit Sharma3, Sansar Chand Sharma4
1 Assistant Professor, Department of Pathology, Kalpana Chawla Government Medical College, Karnal, Haryana, India.
2 Professor, Department of Pathology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India.
3 Junior Resident, Department of Community Medicine, SHKM Government Medical College, Nalhar, Mewat, Haryana, India.
4 Director and Professor, Department of Orthopaedics, SHKM Government Medical College, Nalhar, Mewat, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sonam Sharma, B-5, Varun CGHS Ltd., Plot No. GH-03, Sector-52, Gurgaon-122003, Haryana, India.
E-mail: drsonamsharma@gmail.com
Filariasis is a global health problem which is endemic in tropical and subtropical regions of Asia, Central and South America and Pacific Island nations. The most common parasite causing lymphatic filariasis in India is Wuchereria bancrofti, the microfilariae of which has been detected incidentally in fine needle aspirates and aspirated body fluids. However, its presence in the bone marrow aspirates is quite uncommon and that too in co-existence with a haematological malignancy. We report one such extremely rare case of Wuchereria bancrofti microfilaraemia in a multiple myeloma patient, which is the second case to be documented in the world literature to the best of our knowledge.
Bone marrow aspirate, Microfilaria, Peripheral blood smear, Plasma cell dyscrasia
Case Report
A 52-year-old male patient presented with a history of weakness, lethargy and backache since last five months. On physical examination, he was afebrile and had moderate pallor. There was no significant organomegaly or lymphadenopathy. Haematological investigations revealed a haemoglobin level of 8.7 gm/dL, a total leukocyte count of 5,200 cells/cumm and the platelet count of 80,000/cumm. The differential leukocyte count was as follows: neutrophils 75%, lymphocytes 20%, eosinophils 2% and monocytes 3%. The Erythrocyte Sedimentation Rate (ESR) was 95 mm in the first hour as per the Westergren method. The peripheral blood smears showed normocytic normochromic Red Blood Cells (RBCs) with RBCs showing rouleaux formation with a slightly basophilic stained background.
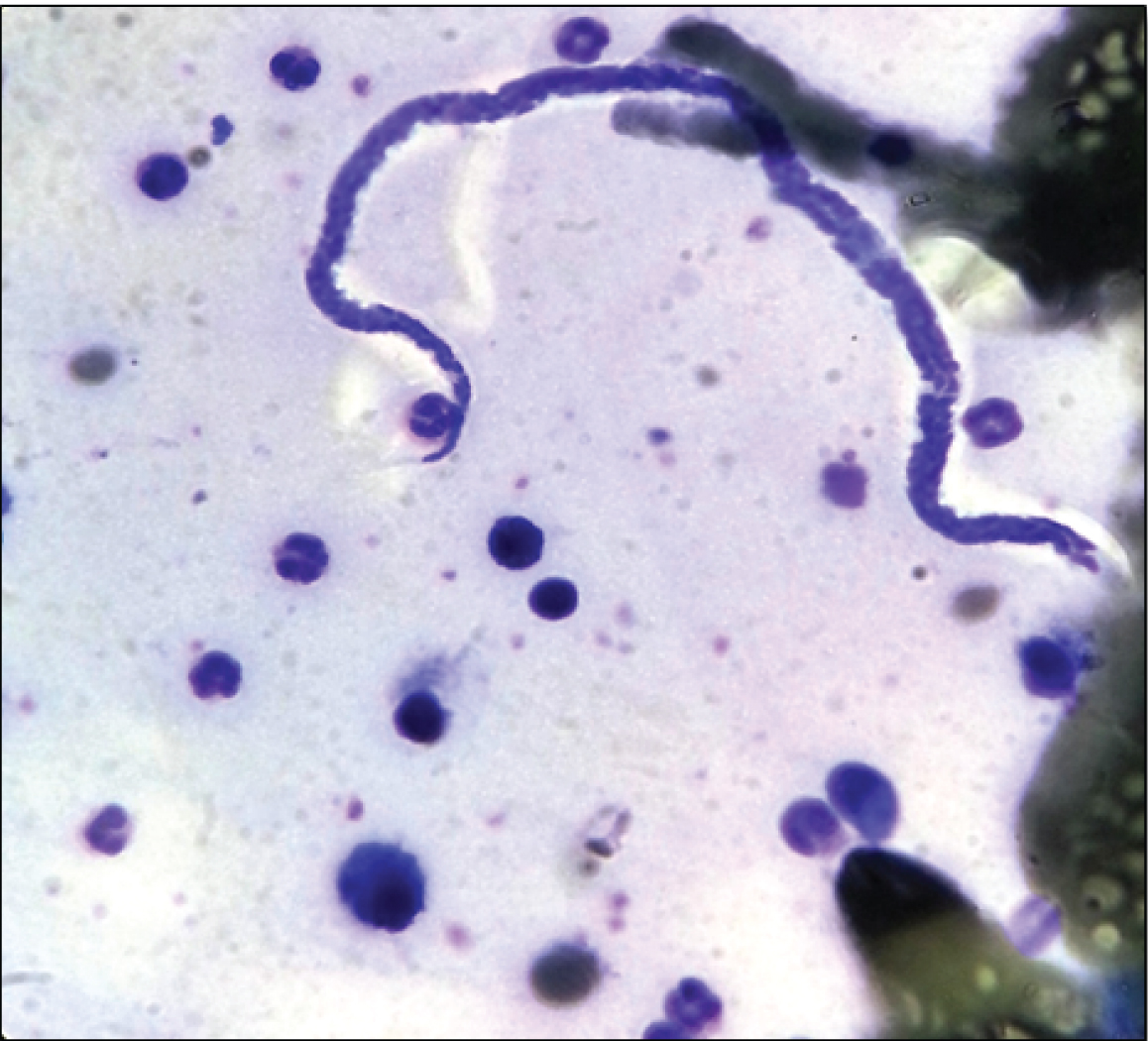
Based on the clinical history of backache, high ESR and peripheral smear findings, a bone marrow study was suggested. After taking and informed consent and all aseptic measures, patient’s bone marrow was aspirated from posterior superior iliac spine. The smears prepared were air dried and stained with May Grunwald Giemsa (MGG) stain. The bone marrow aspirate smears showed mainly sheets of mature plasma cells, some of which were bi-nucleated and tri-nucleated with presence of rare plasmablasts. These plasma cells constituted 70% of all nucleated cells. Rest of the haematopoietic lineages were reduced. Incidentally noted were a few sheathed Microfilariae (Mf), morphologically characterised as Wuchereria bancrofti, as they had smooth graceful curves, had no nuclei in the tail tip, had a clear space at the cephalic and caudal ends with pointed posterior ends [Table/Fig-1].
Wuchereria bancrofti microfilaria along with plasma cells in bone marrow aspirate smears (MGG stain, 40X).
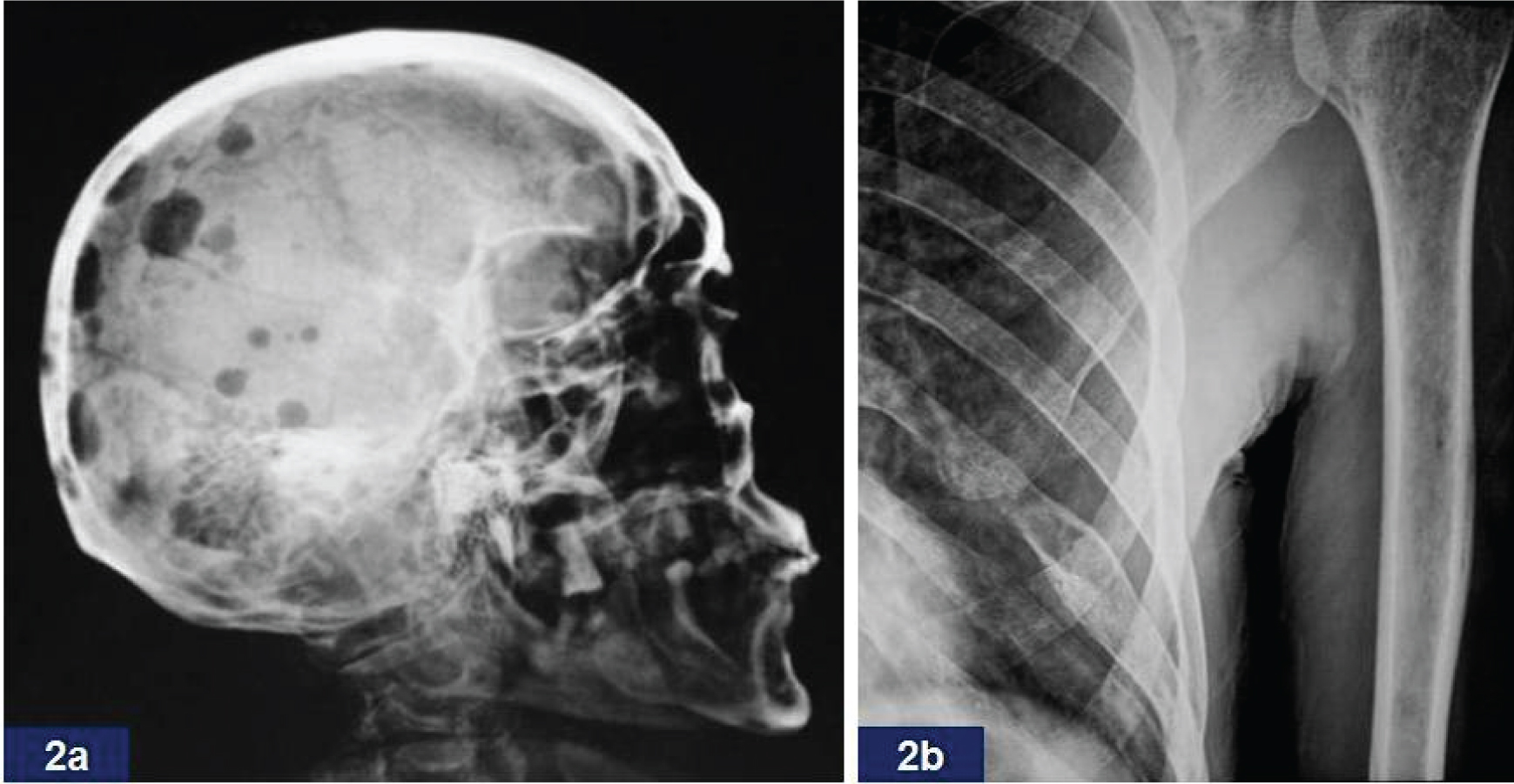
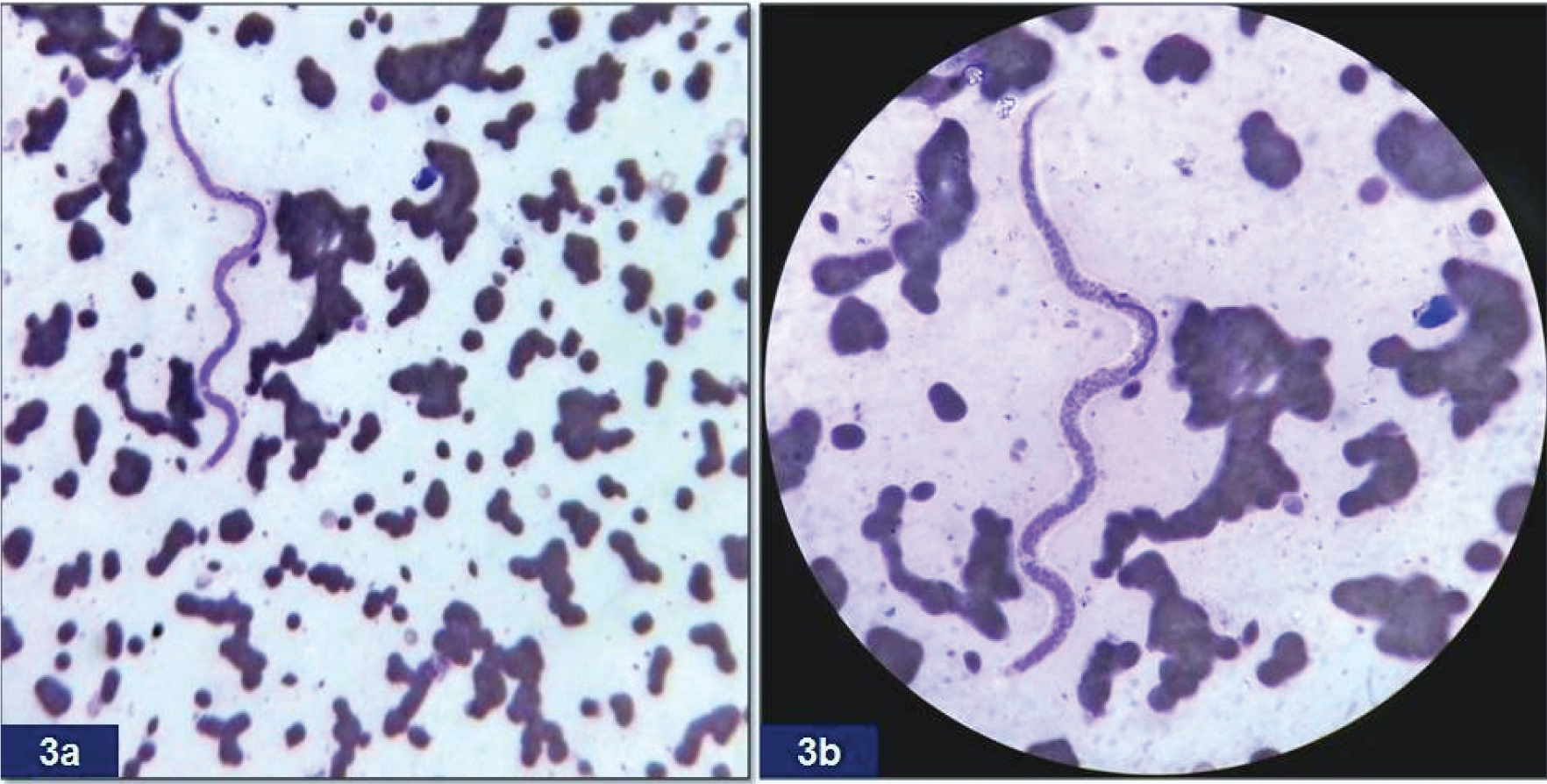
The patient revisited and was followed up further. His biochemical parameters showed M spike on serum electrophoresis, Immunoglobulin G (IgG) levels and beta-2 microglobulin levels on nephelometry were markedly raised. His skeletal survey revealed multiple lytic lesions in the skull, rib and spine [Table/Fig-2a,b]. Ultrasonography revealed no pleural or abdominal effusion. No lymphoedema or lymphangitis was noted. The peripheral blood smear and the bone marrow aspirate smears were again reviewed, and to our astonishment, the peripheral smear revealed microfilaria, which was missed during the initial screening [Table/Fig-3a,b]. A repeat blood film was made taking midnight sample and also 1 mL venous sample which was processed through membrane filtration technique. Both techniques revealed presence of Mf, more so with membrane filtration technique. No peripheral eosinophilia was recorded again. Based on these findings a final diagnosis of multiple myeloma with Wuchereria bancrofti microfilaraemia was rendered. The patient was taken up for myeloma as well as anti-filarial treatment. Further evaluations were not possible as the patient was lost to follow up.
a) Skiagram showing multiple punched out lytic lesions in the skull; b) Diffuse osteopenia with a lytic lesion in the left 8th rib.
a) Sheathed microfilaria with rouleaux formation of the red blood cells and blue background of the peripheral smear (Leishman stain, 20X); b) High power view (Leishman stain, 40X).
Discussion
Filariasis is a disease group affecting humans and animals, caused by filariae which is a nematodal parasites of the order Filariidae [1]. Of all the species of filariasis, Wuchereria bancrofti alone accounts for a staggering 99.4% cases [2]. Human beings serve as the definitive host for the parasite where it most commonly resides in the lymphatic system and mosquitoes serve as the intermediate host. The adult female parasite, being ovoviviparous, gives birth to the ova containing Mf that circulates in the blood stream [3].
According to World Health Organization, half of the 12 million cases in the world, Lymphatic Filariasis (LF) occur in South East Asia with the disease being endemic in India. It is a major source of morbidity and causes disability as well as disfiguration next to leprosy. In a study it has been estimated that filariasis is a source of great economic burden to the susceptible population, costing the Indian treasury up to 842 million per year [4].
Mf has been associated as an incidental finding in many unusual settings and locations such as epulis (gingiva), in aspirates from the thyroid, breast, lymph nodes, subcutaneous nodules, in cervical scrape smears, nipple secretions, and physiological body fluids (including pleural, bronchial washings and cerebrospinal fluid) [5-7]. Mf has also surprised the pathologists with its appearance in cytological aspirates of malignancies [8]. While in bone marrow aspirates, it has been seldom reported in the literature. Usually, its presence in bone marrow aspirates has been seen to be associated with various haematological disorders such as marrow hypoplasia, metastatic carcinomatous deposits, megaloblastic anemia, acute leukaemias and chronic myeloid leukaemia [9-13]. An extensive search of the literature revealed one case of Wuchereria bancrofti Mf being found in a multiple myeloma patient [14]. The present case is the second such case occurring worldwide, to the best of our knowledge, which is being reported from Northern India.
The clinical presentation comprising of eosiniophilia, lymphangitis and lymphoedema usually accompanies filariasis in most of the cases. In the present case, none was encountered and the situation was confounded by presence of signs and symptoms of plasma cell dyscrasia. However, the absence of eosinophilia in the present case is not unique because a glance through most of the cases of Mf in bone marrow reveal the same finding [9,13]. There have been many hypothesis explaining this phenomenon with the most acceptable consensus attributing it to a state of increased oxidative ionic changes noted in occult and long standing filariasis which lead to an aberrant and deviant immune response [15].
Most of the case reports documenting Mf in bone marrow aspirates have explained the haematological changes in marrow on the basis of the aetiological factors such as pharmacotherapeutic agents, pathogens, myelopthesis due to marrow infiltration with the thrust on the fact that the haematological findings of pancytopenia, thrombocytopenia or megaloblastoid change being unrelated to filarial infestation. Hence, putting Mf as an incidental innocent bystander [10].
For LF, there is known mechanism of the mitogenic factors which acts on T4+ cells but not on T8+ T lymphocytes or on B cells. T4+ lymphocytes stimulated with filarial mitogen augment the in vitro production of immunoglobulins by autologous B lymphocytes that lead to polyclonal hypergammaglobulinemia [16].
Whether in occult marrow filariasis, a high load of Mf can stimulate over expression of plasma cells is also much debatable. In view of these findings, we speculate that demonstration of Mf in a case of multiple myeloma is only an incidental finding needs to be taken with a pinch of salt. Although, with the present case, there are only two case reports worldwide which have documented finding of Mf in a multiple myeloma patient, it is difficult to comment upon this rare occurrence. However, we propose that in all such cases bone marrow biopsy needs to be done followed by immunohistochemical studies to comment upon the monoclonality of the plasma cells and to exclude reactive plasmacytosis with polyclonal plasma cell population. In our case although the clinical presentation and other investigations like haematological, biochemical and radiological survey did back up a possibility of multiple myeloma, bone marrow biopsy study was not done as patient was lost to follow up.
Conclusion
The present case is second case of concomitant Wuchereria bancrofti microfilaraemia and multiple myeloma worldwide. It is suggested that especially in tropical and sub-tropical countries a thorough screening for microfilaremia should be done in all the cases of haematological malignancies even in absence of eosinophilia and lymphatic obstructive symptoms. Further, molecular level investigations and more insight is required to understand the possible pathophysiology behind the haematological manifestations arising due to filariasis.
[1]. Knopp S, Steinmann P, Hatz C, Keiser J, Utzinger J, Nematode infections: filariasesInfect Dis Clin North Am 2012 26(2):359-81. [Google Scholar]
[2]. http://www.searo.who.int/entity/vector_borne_tropical_diseases/topics/lymphatic_filariasis/en/index.html [accessed 26 July 2016] [Google Scholar]
[3]. Park K, Epidemiology of communicable diseases. In: Park K, editorPark’s Text Book of Preventive and Social Medicine 2011 21st edNew DelhiBhanot publishers:245-46. [Google Scholar]
[4]. Ramaiah KD, Das PK, Michael E, Guyatt H, The economic burden of lymphatic filariasis in IndiaParasitol Today 2000 16(6):251-53. [Google Scholar]
[5]. Tewarson SL, Mehrotra R, Singh M, Mannan R, Detection of microfilaria of Wuchereria bancrofti in cerebro spinal fluidCytopathol 2007 18:393-94. [Google Scholar]
[6]. Mannan R, Bhasin TS, Manjari M, Misra V, Low Density Microfilaraemia as a causative agent in a case of unexplained ascitis of suspicious natureJ Clin Diagn Res 2013 7(7):1441-43. [Google Scholar]
[7]. Dhanya RCS, Jayprakash HT, Microfilariae, a common parasite in an unusual site: a case report with literature reviewJ Clin Diagn Res 2016 10(4):ED08-ED09. [Google Scholar]
[8]. Gupta S, Sodhani P, Jain S, Kumar N, Microfilariae in association with neoplastic lesions: Report of five casesCytopathol 2001 12(2):120-26. [Google Scholar]
[9]. Sharma S, Rawat A, Chowhan A, Microfilariae in bone marrow aspiration smears, correlation with marrow hypoplasia: a report of six casesIndian J Pathol Micrbiol 2006 49(4):566-68. [Google Scholar]
[10]. Tummidi S, Parto MK, Bal AK, Choudhury A, Microfilariae in a bone marrow aspirateBMC Res Notes 2016 9:256 [Google Scholar]
[11]. Arundhati Kumar A, Kumar R, Acute lymphoblastic leukaemia with Microfilariae: a rare coincidence in bone marrow aspiratesIndian J Haematol Blood Transfus 2011 27:111-12. [Google Scholar]
[12]. Molina MA, Cabezas MT, Giménez MJ, Mansonella perstans filariasis in an HIV patient: a finding in the bone marrowHaematologica 1999 84:861 [Google Scholar]
[13]. Kinger M, Chakrabarti PR, Sharma S, Kiyawat P, Unusual case of bancroftian filariasis co-existing with chronic myeloid leukaemiaAnn Trop Med Public Health 2014 7:64-66. [Google Scholar]
[14]. Kolte S, Mane P, Microfilaria of Wuchereria bancrofti in plasma cell myeloma: A case reportJ Vector Borne Dis 2015 52:342-43. [Google Scholar]
[15]. Pal BK, Kulkarni S, Bhandari Y, Ganesh BB, Goswami K, Reddy MV, Lymphatic filariasis: a possible pathophysiological nexus with oxidative stressTrans R Soc Trop Med Hyg 2006 100(7):650-55. [Google Scholar]
[16]. Wadee AA, Piessens WF, Microfilariae of Brugia malayi contain a T cell mitogenAm J Trop Med Hyg 1986 35(1):141-47. [Google Scholar]