Extra-adrenal Myelolipoma: Tumour at an Unusual Site
BR Yelikar1, K Mamatha2, Abhey Chawla3, Neha Kathpal4
1 Professor and Head, Department of Pathology, Shri B.M.Patil Medical College Hospital and Research Centre, Vijayapura, Karnataka, India.
2 Assistant Professor, Department of Pathology, Shri B.M.Patil Medical College Hospital and Research Centre, Vijayapura, Karnataka, India.
3 Postgraduate Student, Department of Pathology, Shri B.M.Patil Medical College Hospital and Research Centre, Vijayapura, Karnataka, India.
4 Postgraduate Student, Department of Pathology, Shri B.M.Patil Medical College Hospital and Research Centre, Vijayapura, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K Mamatha, Assistant Professor, Department of Pathology, Shri B.M.Patil Medical College Hospital and Research Centre, Vijayapura-586103, Karnataka, India.
E-mail: mamatha.k@bldeuniversity.ac.in
A myelolipoma is a rare, well circumscribed, benign tumour composed of mature adipose and haematopoietic tissue. Classical location is adrenal gland but extra-adrenal cases are also reported in the presacral region, liver, mediastinum, perirenal, stomach with most common site being the presacral area. Only few cases of extra-adrenal myelolipoma have been reported in literature till now with an incidence of 14% of all myelolipomas. Differential diagnosis includes liposarcoma, teratoma, and extramedullary haematopoiesis. Histopathological diagnosis plays a major role in confirmation but also requires concordance of CT, MRI, and Guided biopsy. Extra-adrenal myelolipomas are very rare and their presence and location can be easily confused with malignant tumour. We present this case in a 54-year-old male with mass per abdomen and weight loss since one year.
Extra-adrenal, Pre-sacral, Retroperitoneum
Case Report
A 54-year-old male presented with mass per abdomen in the lower quadrant for last one year which was progressively increasing in size. Patient also had loss of appetite, weight loss and constipation. Patient denied any urinary symptoms. There was no significant past history of any systemic disease.
On systemic examination, a mass was noted in the left iliac fossa 3 cm below the umbilicus which was irregular, immobile, firm and hard in consistency. An ultrasound guided fine needle aspiration was performed and reported as atypical lipoma in a private hospital. Findings were presence of adipocyte fragments, area of necrosis, foamy macrophages and some of the adipocytes with atypical features in the form of nuclear indentation with hyperchromatic nuclei and vacuolated cytoplasm. Contrast enhanced axial CT (CECT) showed an evidence of heterogeneously enhancing retroperitoneal mass on left side [Table/Fig-1]. MRI pelvis showed a large lobulated T1 and T2 hyper-heterointense retroperitoneal mass in presacral region measuring 18 cm × 13 cm × 7.8 cm and was reported as liposarcoma. An exploratory laparotomy and surgical excision was done and specimen was sent for histopathological examination.
CECT showed heterogenously enhancing retroperitoneal mass.
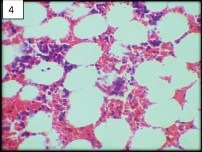
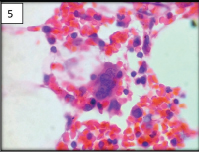
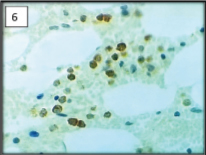
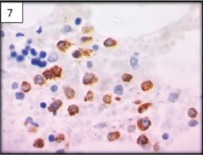
Grossly, single fibro-fatty tissue mass measuring 16 cm × 9 cm × 4 cm was received [Table/Fig-2]. External surface was encapsulated with areas of congestion. On the cut section, it was yellowish, greasy with areas of haemorrhage [Table/Fig-3]. On microscopic examination [Table/Fig-4,5] tumour tissue comprised of lobules of mature adipose tissue interspersed with haematopoietic cells. Individual adipocytes were large, round with eccentrically placed small nucleus and abundant clear cytoplasm. It was reported as myelolipoma and sent for immunohistochemistry for confirmation. Immunohistochemistry study with myeloperoxidase for myeloid cells [Table/Fig-6] and CD61 for megakaryocytes was positive, confirming our histopathological diagnosis of myelolipoma [Table/Fig-7].
Gross photograph of myelolipoma measuring 16 cm × 9 cm × 4 cm.
Cut Section having yellowish greasy with areas of haemorrhage.
Adipose tissue admixed with trilineage haematopoietic cells (H&E, 10X).
High power showing megakaryocytes and myeloid cells (H&E, 40X).
Myeloperoxidase positive for cytoplasmic granules of myeloid cells (IHC 40X).
CD61 positive for megakaryocytes showing membrane positivity (IHC 40X).
Post-operative recovery of the patient was uneventful. Patient did not comply with the postoperative follow up advice.
Discussion
Myelolipomas are rare benign neoplasms characterized by the presence of mature adipose tissue and variable amount of haematopoietic tissue most commonly occurring in adrenal gland [1]. Adrenal myelolipomas are more common and account for incidence of 15% of incidental adrenal masses. There have been only few case reports of extra-adrenal myelolipoma in the current literature [1-9]. It occurs in 6th-8th decade with a female to male predominance of 2:1 [1-9]. Myelolipoma can manifest in various clinicopathological patterns such as: extra-adrenal myelolipoma, solitary adrenal myelolipoma, adrenal myelolipoma with haemorrhage, and myelolipoma associated with other adrenal diseases [2]. This case report alerts to the possibility of myelolipoma as a differential diagnosis in fat containing tumour [1].
Extra-adrenal myelolipomas are very rare and about half of which occur in retroperitoneal space and presacral region as found in our case too. Other common sites are perirenal, mediastinum, liver and stomach [1-3]. Out of these, pre-sacral region is common, accounting for half of the cases. Presacral myelolipoma have a predilection towards females in fifth to seventh decades [1]. The symptoms are directly related to size of the tumour, although, majority are small and incidental. But, there are few case reports with large mass measuring upto 26 cm in literature [1]. Myelolipomas are associated with conditions like cushing’s syndrome, addison’s disease, adrenal hyperplasia, and chronic use of exogenous steroids [4].
Although, the etiology is unknown, some theories about the pathogenesis of extra-adrenal myelolipoma suggest that they occur due to: (a) embolization of bone marrow tissue; (b) reactivation of peritoneal embryonic connective tissue, in response to a triggered stimulus, like an endocrine dysfunction or in septic conditions [2].
Imaging characteristics of extra-adrenal myelolipomas are similar to adrenal counterparts. If the tumour predominantly contains erythroid/myeloid cells then it appears as a hypoechoic mass on ultrasonography if it predominantly contains fat. On CT scan, appearance depends on composition of the lesion and often appears as encapsulated mass with macroscopic fatty tissue admixed with areas of soft tissue which suggests the diagnosis of myelolipoma. On MR imaging, fat component yields high intensity on T1-weighted images and haematopoietic elements will have lower signal intensity on T1-weighted images and intermediate on T2-weighted images [5].
Differential diagnosis for myelolipoma when located in retroperitoneum is mainly lipoma, liposarcoma, teratoma and even extramedullary haematopoiesis. Liposarcomas can be differentiated because of their infiltrative growth pattern [6].
Extra-medullary haematopoiesis resembles myeloliopma, however their imaging characteristics are quite different as they are multifocal, poorly circumscribed and with insufficient macroscopic fat. Clinically extramedullary haematopoiesis is seen in young to middle aged men and in association with myeloprolifrative disorders and chronic haemolytic anaemias [5].
Teratomas can be differentiated by the presence of derivatives from other germ cell layers.
Imaging modalities are of little help in cases of fat containing tumours as they exhibit overlapping features. Thus, histopathological examination is a cornerstone for diagnosis of myelolipoma and confirmation with immunohistochemistry [1].
Immunohistochemistry markers like myeloperoxidase, glycophorin A, factor VIII-related antigen and CD68 which stains myeloid, erythroid and megakaryocytic cells respectively aids in confirming the histopathological diagnosis [7].
Conclusion
Myelolipomas are rare benign tumours that can have both locations: adrenal and extra-adrenal. Imaging studies typically reveal heterogeneous lesion predominantly fat-containing masses with areas of enhancing soft tissue. Histopathological confirmation is mandatory for extra-adrenal myelolipoma mainly to rule out malignancies like liposarcoma.
[1]. Fourati H, Fourati M, Hentati Y, Daoud E, Mnif Z, Presacral myelolipoma: Imaging featuresPresse Med 2015 44(11):1196-98. [Google Scholar]
[2]. Leite M, Gonçalves A, Ferreira A, Ortiz S, Esteves R, Tavora I, An unusual fat-containing presacral tumour in an elderly patientCase Rep Radiol 2014 2014:01-06. [Google Scholar]
[3]. Gagliardo C, Falanga G, Sutera R, La Tona G, Lo Casto A, Midiri M, Presacral MyelolipomaNeuro Radiol J 2014 27:764-69. [Google Scholar]
[4]. Baker K, Lee D, Huang M, Gould E, Presacral myelolipoma: a case report and review of imaging findingsJ Radiol Case Rep 2012 6(6):01-09. [Google Scholar]
[5]. Ghatak S, Mridha A, Laparoscopic resection of a large adrenal myelolipoma: a case reportCases J 2009 2(1):9313 [Google Scholar]
[6]. Dann P, Krinsky G, Israel G, Case 135: Presacral MyelolipomaRadiology 2008 248(1):314 [Google Scholar]
[7]. Sato K, Ueda Y, Katsuda S, Tsuchihara K, Myelolipoma of the lung: a case report and brief reviewJ Clin Pathol 2007 60:728-30. [Google Scholar]
[8]. Shen C, Zhou K, Lai Y, Fan J, Liu L, Che G, Review of primary extra-adrenal myelolipoma of the thoraxJ Surg Res 2017 207:131-37. [Google Scholar]
[9]. Chauhan K, Garg M, Chaudhry M, Sharma M, Bindal T, Retroperitoneal myelolipoma, a diagnostic dilemma: A case report and review of literatureSaudi J Health Sci 2016 5(2):90-92. [Google Scholar]