Introduction
Elastography is a new technique that aim to assess tissue hardness non-invasively. Recently, it has been used for differentiating benign from malignant lymphadenopathy.
Aim
To evaluate the sensitivity and specificity of elastography for differentiating benign from malignant cervical lymphadenopathy and to compare its findings with B-mode and color doppler findings.
Materials and Methods
The present study was conducted on 50 patients with cervical lymphadenopathy. In each patient, even if multiple enlarged lymph nodes were found, only one lymph node was sampled which was most suspicious for malignancy. This selection was based on size of the lymph node and other B-mode sonography characteristics. B-mode and color doppler findings were recorded. In addition to this, strain elastography was done and five elastography patterns were defined: high elasticity (soft): pattern I represented no or very small hard area while spectrum pattern V presented where almost whole of lymph node showed hard pattern on strain elastography. Patterns II and III represented hard areas <45% and >45% respectively while pattern IV represented peripheral hard area with central soft area (due to central necrosis). Patterns I and II were considered benign. Patterns III, IV and V were considered to represent malignant lymph nodes. Additionally, a cine loop of elastography was acquired for calculation of strain ratio using adjacent muscle as reference. A cut-off value of less then two (<2) of strain ratio was used to define benign lymph nodes and more then or equal to two (≥2) was used to define malignant lymph nodes. Final diagnosis of benign versus malignant lymph node was based upon other relevant investigations like Fine Needle Aspiration Cytology (FNAC)/biopsy findings and/or clinical follow-up after three months. Statistical analysis was done using StatPac version 4.0 (StatPac, Inc., Bloomington, MN). Chi-square test was used to compare various B-mode and color doppler parameters, elastography patterns and strain ratio between benign and malignant groups.
Results
Of all the B-mode parameters, only lymph node border and hilum showed more than 70% accuracy for correctly differentiating benign from malignant lymph nodes while color doppler showed 82% accuracy for the same. Elastography pattern and strain ratio achieved 90% and 94% accuracy for correctly differentiating benign from malignant lymph nodes.
Conclusion
Elastography pattern and strain ratio are useful in addition to B-mode and color doppler ultrasound for evaluation of cervical lymph nodes.
Introduction
Elasticity represents a tissue characteristic that denotes the ability to prevent tissue displacement under pressure. It varies in different types of tissue under physiological condition. In sonographic elastography, image representation of tissue hardness can be obtained using a conventional sonography machine and probe with the help of special software [1,2]. Strain elastography aim to assess the tissue elasticity by applying intermittent slight manual compressive force to the tissue of interest. Hard tissues will be much less deformable with pressure compared to soft tissues and these results can be colour coded and displayed as an elastography image. By convention, blue colour is used to represent hard tissue and red colour to represent soft tissue with yellow and green colors for intermediate elasticity tissues [2,3].
Cervical lymph nodes are easily accessible for clinical and sonographic assessment. They can get enlarged in a variety of malignant lesions especially of head and neck region and often have prognostic significance. Moreover, cervical lymph node enlargement can also be secondary to a variety of benign causes like tuberculosis and reactive lymphadenopathy in upper airway infections [4].
Sometimes metastatic cervical lymphadenopathy appears as the first symptom in patients without known malignancy and in about 5% of patients, the cause of metastatic cervical lymphadenopathy remains unknown even after extensive workup [5]. Therefore, it is important to discriminate benign from malignant lymph nodes in patients with a known primary tumour and also to detect malignant lymph node enlargement in patients without any known malignancy to direct further diagnostic evaluation.
Ultrasound evaluation with high frequency transducers is the cornerstone in investigation of enlarged cervical lymph nodes. Various B-mode (size, shape, echotexture, border, hilum) and color/power doppler parameters have been used for differentiating benign from malignant lymph nodes but results are often overlapping [6,7].
Malignant lymph nodes are relatively harder compared to benign lymph nodes, ultrasound elastography aims to depict tissue stiffness and thereby adds a new parameter to ultrasound assessment of lymph nodes [8]. The aim of present prospective study was to evaluate the sensitivity and specificity of elastography for differentiating benign from malignant cervical lymph nodes and to compare its findings with B-mode and color doppler findings.
Materials and Methods
This prospective study was conducted in Radiodiagnosis Department of Maharishi Markandeshwar Institute of Medial Sciences and Research, Ambala on 50 consecutive subjects from October 2016 to April 2017 presenting for sonographic assessment and willing to participate in the study during the study interval. Study was approved by the Ethical Committee. The study was conducted in patients with enlarged cervical lymph nodes of any sex/age group who presented for sonographic evaluation. Patients who have received chemotherapy or radiotherapy prior to examination were excluded from the study.
Ultrasound Examination
Ultrasound examination was conducted on EPIQ 7G (Philips Ultrasound Systems, USA) using high frequency (5-18MHz) linear transducer. In each patient, only one lymph node which was considered most suspicious for malignancy was sampled. At gray-scale US, the following US characteristics were evaluated: size (Short axis dimension), shape (short axis/long axis ratio), border (regular/irregular), echogenicity (homogeneous/inhomogeneous), and hilum (present/absent). Color Doppler findings were classified into two patterns: Pattern I (hilar or no flow) and pattern II (central or peripheral flow). Pattern I was used to define benign lymph nodes and pattern II was used to define malignant lymph nodes.
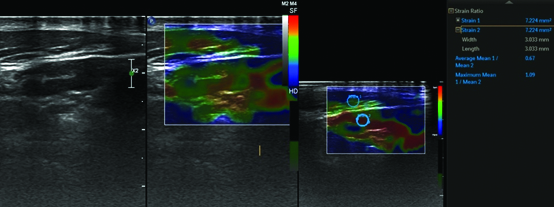
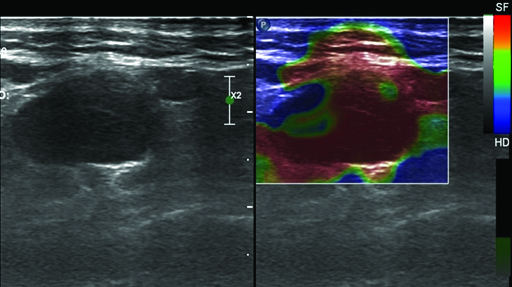
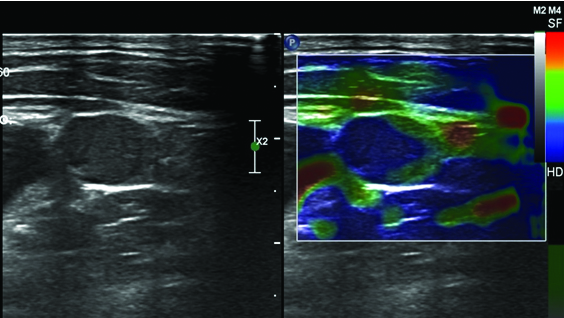
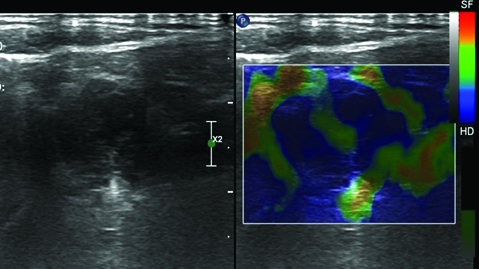
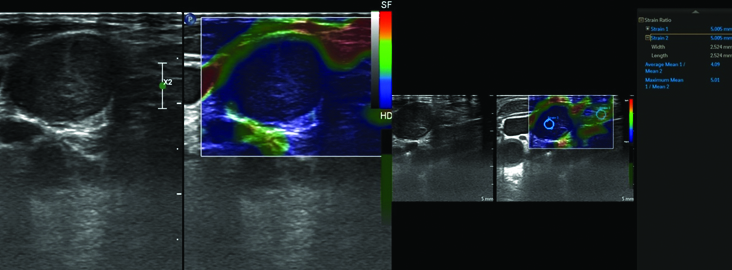
Each patient was subjected to additional real-time elastography examination using the same transducer. For elastography, compression with light pressure followed by decompression was repeated until a stable image was obtained. Five elastography scales were defined: high elasticity (soft): pattern I represented no or very small hard area while at other spectrum pattern V presented where almost whole of lymph node showed hard pattern on strain elastography. Patterns II and III represented hard areas <45% and >45% respectively while pattern IV represented peripheral hard area with central soft area (due to central necrosis). Similar patterns have been defined previously in literature [3,7]. Patterns I and II were considered benign. Patterns III, IV and V were considered to represent malignant lymph nodes. Additional a cine loop of elastography was acquired for calculation of strain ratio using adjacent muscle as reference. For obtaining strain ratio, rounded region of interest was taken at lymph node and at adjacent muscle and thus ratio of their mean elasticity was obtained. A cut-off value of <2 of strain ratio was used to define benign lymph nodes and ≥2 was used to define malignant lymph nodes [Table/Fig-1,2,3,4 and 5]. Final diagnosis of benign versus malignant lymph node was based upon other relevant investigations like FNAC/biopsy findings and/or clinical follow-up after three months.
Showing elastography pattern I in a reactive lymph node with predominantly soft areas (orange/green) and very small hard area (blue). Strain ratio was 0.67.
Showing elastography pattern II in a reactive lymph node with hard area (<45%).
Showing elastography pattern III in a metastatic lymph node with hard area (>45%).
Showing elastography pattern IV with peripheral hard and central soft area in a metastatic lymph node.
Showing elastography pattern V with hard area occupying whole of lymph node in a metastatic lymph node. Strain ratio was 4.09.
Statistical Analysis
Statistical analysis was done using StatPac version 4.0 (StatPac, Inc., Bloomington, MN). Chi-square test was used to compare various B-mode and color doppler parameters, elastography patterns and strain ratio between benign and malignant groups. p-value of <0.05 was considered to be statistically significant and p-value of <0.01 was considered highly significant. Sensitivity, specificity, positive predictive value, negative predictive value and accuracy of individual B-mode, color doppler and elastography parameters were calculated.
Results
Out of the 50 patients in the study, 36 were male and 14 were female. Mean age of the patients was 41.1±12.7 years (range 21-78 years). On final diagnosis, 29 had benign lymph nodes (22 reactive and seven tubercular) while 21 patients had malignant lymph nodes (17 metastatic and four lymphoma). Out of metastatic lymph nodes, nine were from laryngeal and oropharyngeal carcinomas. Bronchogenic carcinoma accounted for five metastatic lymph nodes with one patient each having metastatic lymph nodes from esophageal carcinoma, papillary carcinoma of thyroid and gall bladder carcinoma [Table/Fig-6]. Of the gray scale findings, lymph node short axis dimension and shape (short axis/long axis ratio), show statistically significant difference between benign and malignant groups with p-value <0.05, while lymph node border and hilum showed highly significant difference between benign and malignant groups with p-value of <0.01. Color Doppler findings showed significant difference between benign and malignant groups [Table/Fig-7]. Elastography patterns and strain ratio showed significant difference between benign and malignant groups [Table/Fig-8].
Final diagnosis in subjects with benign and malignant lymph node enlargement.
| Final diagnosis | Number |
|---|
| Benign (29) | Reactive | 22 |
| Tubercular | 7 |
| Malignant (21) | Metastatic | 17 |
| Lymphoma | 4 |
B-mode and Color Doppler findings in cervical lymph nodes.
| B-mode and Color Doppler findings | Benign (29) | Malignant (21) | p-value |
|---|
| Short axis dimension | ≤8mm | 15 | 5 | 0.046 |
| >8mm | 14 | 16 |
| Short/long axis dimension | ≤0.6 | 18 | 7 | 0.045 |
| >0.6 | 11 | 14 |
| Border | Regular | 23 | 8 | 0.003 |
| Irregular | 6 | 13 |
| Echogenicity | Homogeneous | 16 | 7 | 0.13 |
| Inhomogeneous | 13 | 14 |
| Hilum | Normal | 20 | 4 | <0.005 |
| Abnormal | 9 | 17 |
| Color Doppler | Pattern I | 25 | 5 | <0.001 |
| Pattern II | 4 | 16 |
Showing elastography patterns and strain ratio in cervical lymph nodes.
| Elastography findings | Benign(29) | Malignant(21) | p-value |
|---|
| Elastography pattern | 1 | 20 | 0 | |
| 2 | 6 | 2 | |
| 3 | 2 | 4 | |
| 4 | 1 | 2 | |
| 5 | 0 | 13 | |
| Benign elastography pattern (I and II) | 26 | 2 | <0.001 |
| Malignant elastography pattern (III, IV and V) | 3 | 19 |
| Strain ratio | <2 | 27 | 1 | <0.001 |
| ≥2 | 2 | 20 |
Of all the B-mode parameters, only lymph node border and hilum showed more than 70% accuracy for correctly differentiating benign from malignant lymph nodes while color doppler showed 82% accuracy for the same. Elastography pattern and strain ratio achieved 90% and 94% accuracy for correctly differentiating benign from malignant lymph nodes [Table/Fig-9].
Comparison of B-mode, color Doppler and elastography findings in cervical lymph nodes.
| Sonography finding | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|
| Short axis dimension | 76.19% | 51.72% | 53.33% | 75% | 62% |
| Short/long axis ratio | 66.67% | 62.07% | 56% | 72% | 64% |
| Border | 61.90% | 79.31% | 68.42% | 74.19% | 72% |
| Echogenicity | 66.67% | 55.17% | 51.85% | 69.57% | 60% |
| Hilum | 80.95% | 68.97% | 65.38% | 83.33% | 74% |
| Color Doppler | 76.19% | 86.21% | 80.0% | 83.33% | 82% |
| Elastography pattern | 90.48% | 89.66% | 86.36% | 92.86% | 90% |
| Strain ratio | 95.24% | 93.10% | 90.91% | 96.43% | 94% |
PPV- Positive predictive value
NPV- Negative predictive value
Discussion
Sonography is frequently the first imaging modality used for assessment of cervical lymph nodes. Various B-mode parameters have been in use since long time for this purpose like size, shape, border, hilum and echopattern but overall sensitivity and specificity of these parameters is low and overlapping findings are not infrequent. In present study, only two B-mode parameters (border and lymph node hilum) achieved accuracy of more than 70% for differentiating benign from malignant lymph nodes. Similar results have been reported in other studies [3,7,9]. While some studies have also reported conflicting results with one study reporting normal hilum seen in more than 50% malignant lymph nodes [10]. Another study found short axis dimension as most useful B-mode parameter [11].
Color Doppler is a useful addition to B-mode findings. It has been observed that benign lymph nodes either shows no flow or hilar flow (Pattern I) and malignant lymph nodes show central or peripheral flow (pattern II) [12,13]. Addition of color doppler to sonography increases sensitivity and specificity of ultrasound. In our study, color doppler had high specificity (86.21%) and relatively lower sensitivity (76.19%). Similar findings have been reported in previous studies [12].
Ultrasound elastography is a relatively new technique. It aims to differentiate benign from malignant pathologies based on hardness of tissues assuming that the malignant tissues are harder as compared to benign tissues. It has been initially used for assessment of breast nodules and thyroid lesions. One of the earliest studies for evaluation of sonoelastography for assessment for cervical lymph nodes was conducted by Lyshchik A et al., [12] and they found it very helpful with more than 90% accuracy. Subsequently, few other studies have been conducted on sonoelastogaphy of cervical lymph nodes [3,7,11,14,15].
In present study, five elastography patterns were defined depending upon hardness of tissue. Patterns I and II were considered benign while patterns III to V were considered malignant. Elastography patterns showed excellent agreements for differentiation of benign from malignant lymph nodes (sensitivity – 90.48%, specificity- 89.66% and accuracy – 90%). Similar results have been seen in previous studies [3,7,11]. Hefeda and Badawy [7] found similar accuracy of elastography patterns (sensitivity of 85.3%, specificity of 95.5% and accuracy of 88.9%) for differentiating benign from malignant cervical lymphadenopathy. Alam F et al., [3] made similar observations with elastography patterns showing sensitivity of 83%, specificity of 100% and accuracy of 89% while in the study of Teng DK et al., [11], sensitivity of elastography score was high at 88.4% but specificity was lower at 35.1% and overall accuracy was 66.3%, while Acu L et al., [14] found no added value of elastography to B-mode and color doppler ultrasound.
Another parameter that was assessed in this study was strain ratio which compares elastography of lymph node with adjacent muscle. It has the advantage of making strain elastography semi-quantitative. We found strain ratio to be even better than elastography pattern with overall accuracy of 94% using a cut-off value of two for differentiating benign and malignant lymph nodes (strain ratio <2 considered benign and strain ratio more then or equal to two (≥2) considered malignant). Lyshchik A et al., [12] used a cut-off of 1.5 of strain ratio and achieved a specificity of 98%, sensitivity of 85% and overall accuracy of >90%. Teng DK et al., [11], using a cut-off of 1.78 of strain ratio, achieved sensitivity of >98% and accuracy of more than 84% which was higher than any other B-mode or color doppler or elastography pattern. These results are similar to present study. Similar observations have been made in other studies using different cut offs of strain ratios ranging from 1.18 to 2.3 [15,16]. While few studies found strain ratio to be less useful with only moderate sensitivity and specificity [14,17]. There is variability in the literature regarding optimal strain ratio to differentiate benign from malignant lesions which may be related to demographic variations and scanner differences. We suggest that observers should establish optimal strain ratios in their institutions using own observations over time over their scanners.
Limitation
One of the limitations of present study is small sample size. Another limitation is sampling of only one lymph node per patient. However, elastography appears to be promising technique and with addition of quantitative shear wave elastography in newer scanners, it should become standard part of ultrasound examination of cervical lymph nodes.
Conclusion
Elastography is a useful tool in addition to B-mode and color doppler ultrasound for evaluation of cervical lymph nodes. Elastography pattern and strain ratio are more accurate than B-mode and color doppler for differentiating benign from malignant lymph nodes. It adds very little time to total examination time and can be performed in same setting when patient presents for routine ultrasound. Therefore, it may be routinely used for gathering additional information in assessment of cervical lymph nodes.
PPV- Positive predictive value
NPV- Negative predictive value
[1]. Okasha HH, Mansour M, Attia KA, Khattab HM, Sakr AY, Naguib M, Role of high resolution ultrasound/endosonography and elastography in predicting lymph node malignancyEndoscopic Ultrasound 2014 3(1):58-62. [Google Scholar]
[2]. Ophir J, Garra B, Kallel F, Konofagou E, Krouskop T, Righetti R, Elastographic imagingUltrasound Med Biol 2000 26(suppl 1):S23-9. [Google Scholar]
[3]. Alam F, Naito K, Horiguchi J, Fukuda H, Tachikake T, Ito K, Accuracy of sonographic elastography in the differential diagnosis of enlarged cervical lymph nodes: comparison with conventional B-mode sonographyAJR Am J Roentgenol 2008 191(2):604-10. [Google Scholar]
[4]. Ahuja AT, Ying M, Sonographic evaluation of cervical lymph nodesAJR Am J Roentgenol 2005 184(5):1691-9. [Google Scholar]
[5]. Calabrese L, Jereczek-Fossa BA, Jassem J, Rocca A, Bruschini R, Orecchia R, Diagnosis and management of neck metastases from an unknown primaryActa Otorhinolaryngologica Italica 2005 25(1):2-12. [Google Scholar]
[6]. Ho SS, Metrewefi C, Ahuja AT, Does anybody know how we should measure Doppler parameters in lymph nodes?Clin Radiol 2001 56(2):124-6. [Google Scholar]
[7]. Hefeda MM, Badawy ME, Can ultrasound elastography distinguish metastatic from reactive lymph nodes in patients with primary head and neck cancers?The Egyptian Journal of Radiology and Nuclear Medicine 2014 45(3):715-22. [Google Scholar]
[8]. Sigrist RMS, Liau J, Kaffas AE, Chammas MC, Willmann JK, Ultrasound Elastography: Review of Techniques and Clinical ApplicationsTheranostics 2017 7(5):1303-1329. [Google Scholar]
[9]. Rubaltelli L, Proto E, Salmaso R, Bortoletto P, Candiani F, Cagol P, Sonography of abnormal lymph nodes in vitro: correlation of sonographic and histologic findingsAJR Am JRoentgenol 1990 155(6):1241-4. [Google Scholar]
[10]. Vassallo P, Wernecke K, Roos N, Peters PE, Differentiation of benign from malignant superficial lymphadenopathy: the role of high resolution USRadiology 1992 183(1):215-20. [Google Scholar]
[11]. Teng DK, Wang H, Lin YQ, Sui GQ, Guo F, Sun LN, Value of ultrasound elastography in assessment of enlarged cervical lymph nodesAsian Pac J Cancer Prev 2012 13(5):2081-5. [Google Scholar]
[12]. Lyshchik A, Higashi T, Asato R, Tanaka S, Ito J, Hiraoka M, Cervical lymph node metastases: diagnosis at sonoelastography-initial experienceRadiology 2007 243(1):258-67. [Google Scholar]
[13]. Stramare R, Tregnaghi A, Fittà C, Torraco A, Khadivi Y, Rossi CR, High-sensitivity power Doppler imaging of normal superficial lymph nodesJ Clin Ultrasound 2004 32(6):273-6. [Google Scholar]
[14]. Acu L, Oktar SÖ, Acu R, Yücel C, Cebeci S, Value of Ultrasound Elastography in the Differential Diagnosis of Cervical Lymph Nodes: A Comparative Study With B-mode and Color Doppler SonographyJ Ultrasound Med 2016 35(11):2491-9. [Google Scholar]
[15]. Tugut E, Celenk C, Tanrivermis Sayit A, Bekci T, Gunbey HP, Arslan K, Efficiency of B-mode Ultrasound and Strain Elastography in Differentiating Between Benign and Malignant Cervical Lymph NodesUltrasound Q 2017 33(3):201-7. [Google Scholar]
[16]. Zhang YR, Lv Q, Yin YH, Xie M, Xiang F, Lu C, The value of ultrasound elastography in differential diagnosis of superficial lymph nodesFront Med China 2009 3(3):368-74. [Google Scholar]
[17]. Bhatia KS, Cho CC, Yuen YH, Rasalkar DD, King AD, Ahuja AT, Real-time qualitative ultrasound elastography of cervical lymph nodes in routine clinical practice: interobserver agreement and correlation with malignancyUltrasound Med Biol 2010 36(12):1990-7. [Google Scholar]