Sterile Aortic Root Abscess Mimicking Calcified Aortic Nodule: A Rare Case
Rupesh Kumar1, Javid Raja2, Alok Kumar3
1 Assistant Professor, Advanced Cardiac Center, Cardiothoracic and Vascular Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
2 Senior Resident, Advanced Cardiac Center, Cardiothoracic and Vascular Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
3 Senior Resident, Advanced Cardiac Center, Cardiothoracic and Vascular Anaesthesiology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rupesh Kumar, Room No. 4018, 4th floor Advanced Cardiac Center, Cardiothoracic and Vascular Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh-160012, India.
E-mail: rkctvs@gmail.com
Aortic root abscess or aortic annular abscess is a serious complication of aortic valve endocarditis. It usually occurs in patients with prosthetic aortic valve and coagulase-negative staphylococcal endocarditis. However, we came across a young individual of bicuspid aortic valve with no features of Infective Endocarditis (IE) with severe aortic valve regurgitation with sterile aortic root abscess and severe mitral valve regurgitation. He underwent repair of aortic root followed by replacement of both the valves with mechanical valve prosthesis.
Aortic annular abscess, Infective endocarditis, Valvular heart diseases
Case Report
A 19-year-old male, presented with complaints of palpitation for last ten years, intermittent chest pain for the last six months, symptoms of breathlessness, paroxysmal nocturnal dyspnoea and orthopnoea for the last six months. There was no history of diabetes mellitus, tuberculosis, any drug allergies or fever in the past. He was a non-smoker, non-alcoholic without any history of intravenous drug abuse.
Patient was conscious, well-oriented, afebrile, well hydrated and thin built (Body mass index 16.25 kg/m2). There was no pallor, cyanosis, clubbing, icterus, pedal oedema and generalised lymphadenopathy. He had a pulse rate of 76/minute, regular rhythm, normal volume, bounding in nature, no radio-femoral delay and blood pressure of 128/56 mmHg in the right upper limb in sitting position and respiratory rate of 22/minute. Cardiac examination revealed apical impulse in left 6th intercostal space 1 cm lateral to mid clavicular line, and was hyperdynamic in nature. First heart sound was audible, second heart sound muffled and had a grade 4/6 pansystolic murmur heard in mitral area and Grade 3 early diastolic murmur in aortic area. His blood investigations revealed haemoglobin 12.6 gm/dL and total leucocyte count 8900/mL. Renal function tests and Liver function tests were normal. ECG showed features of left ventricular hypertrophy.
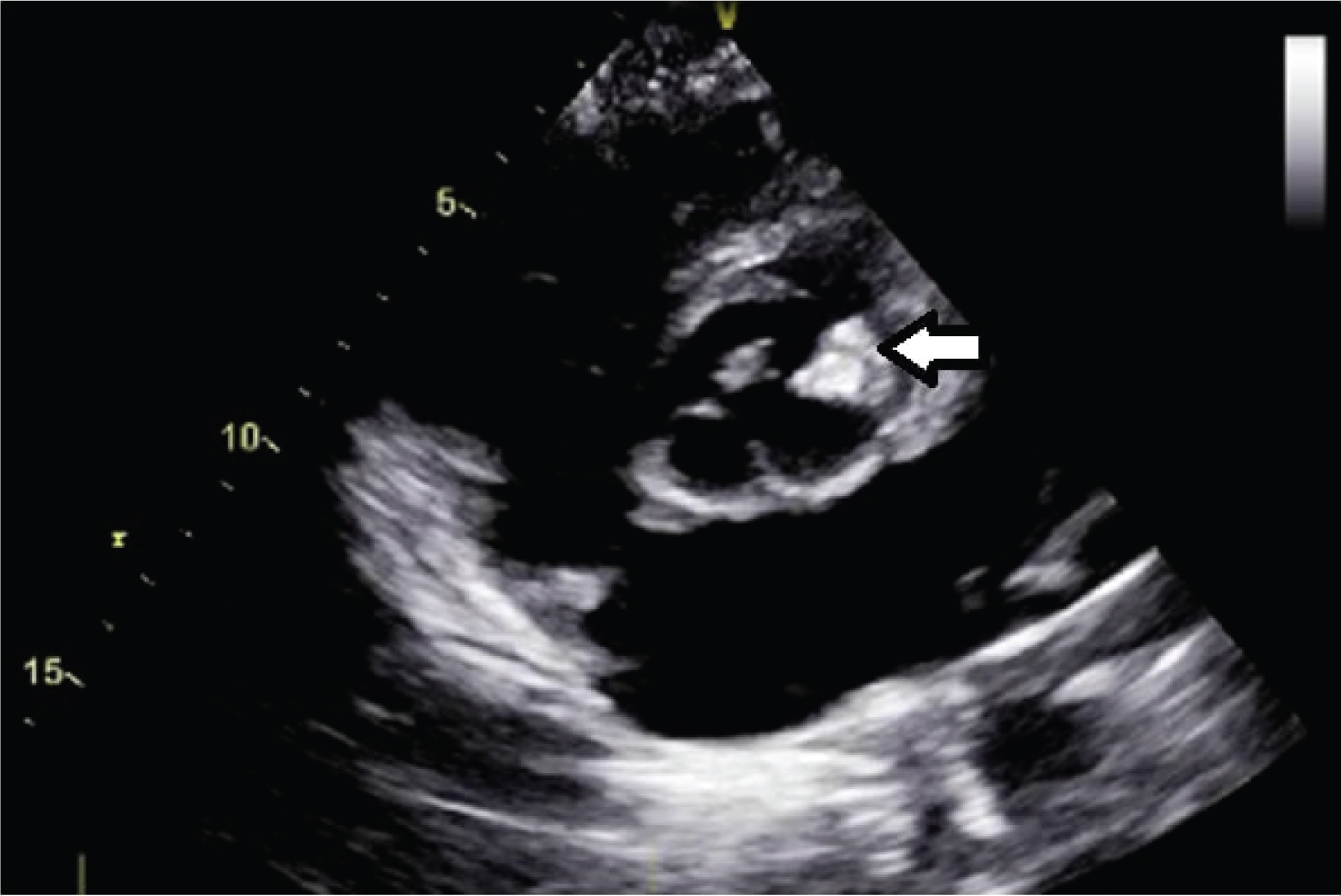
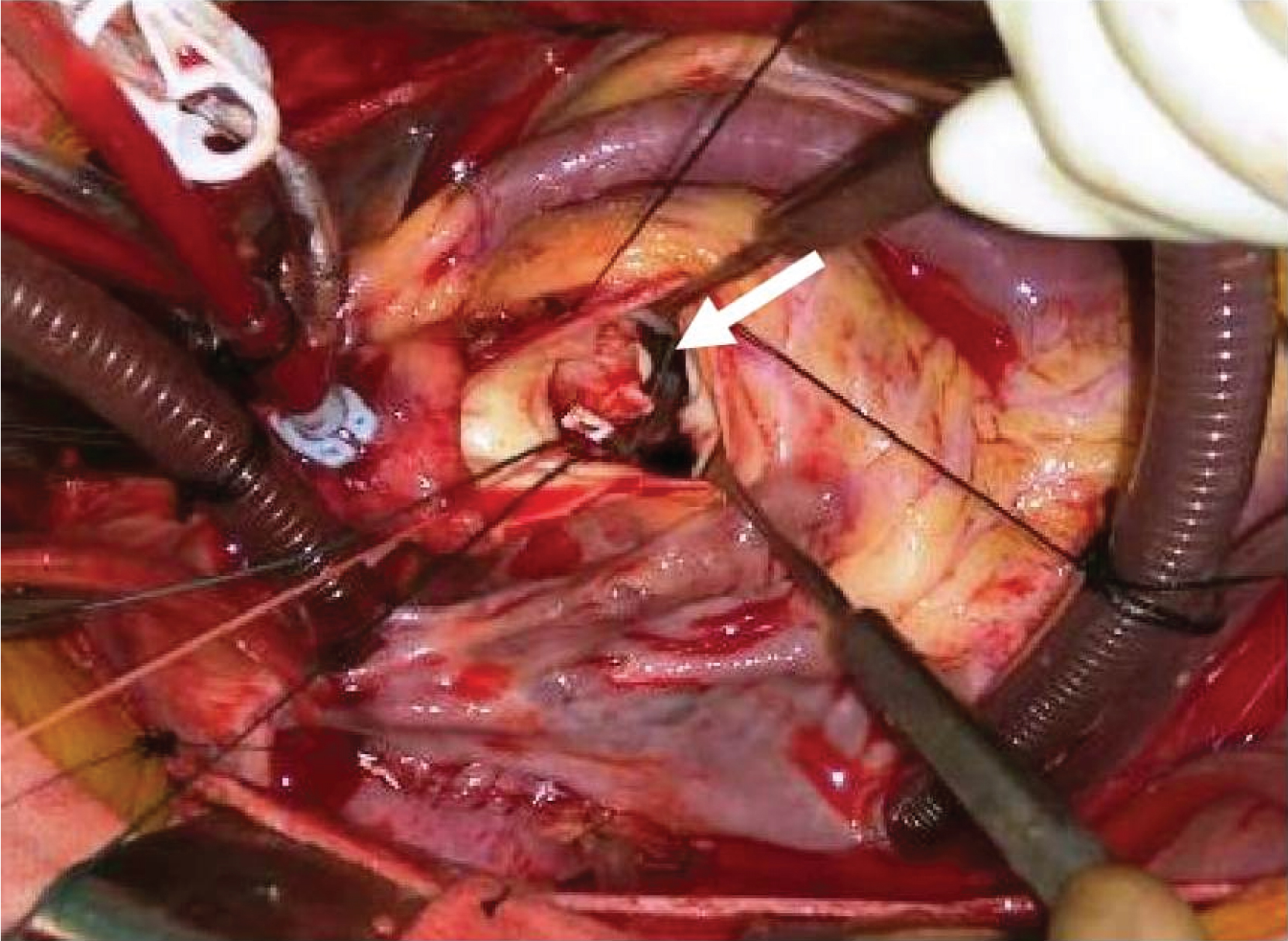
Chest X-ray showed cardiomegaly. Two dimensional Transthoracic Echo (TTE) showed bicuspid aortic valve with 8x13 mm calcific nodule in the left coronary cusp [Table/Fig-1]. There was severe aortic valve regurgitation, severe mitral valve regurgitation, moderate pulmonary arterial hypertension, left ventricular ejection fraction of 42%. Transesophageal Echo (TEE) also corroborated the similar findings. Intraoperatively after midline sternotomy, pericardium was opened and full heparinisation was done. Aorto bicaval cannulation was done. After aortic cross clamping, aortotomy was done and aortic valve leaflets were inspected. Left coronary cusp was oedematous with pus beneath it. Pus was evacuated from abscess cavity and sent for culture and sensitivity [Table/Fig-2]. Thorough lavage was done with saline, the pus was evacuated and the lips of the left coronary cusp were approximated using pledgeted 4-0 polypropelene sutures. Then, left atriotomy was done and mitral valve replacement was performed with 31 mm St. Jude mechanical valve prosthesis followed by aortic valve prosthesis with 21 mm St. Jude mechanical valve. Postoperatively, patient was treated with intravenous vancomycin and meropenem for two weeks followed by oral antibiotics for four weeks even though, the pus culture report came sterile. Patient was discharged on the 14th day in a stable condition and was symptom free after one year of regular follow up.
Transthoracic image showing aortic valve calcification (arrow).
Intraoperative picture showing aortic root abscess (arrow).
Discussion
Aortic root abscess is one of the most dreaded complications of aortic valve IE and carries a high risk of mortality and morbidity [1]. IE in this region with perivalvular extension may lead to complications like periannular or intramyocardial abscess, mycotic false aneurysm, and aortico-left ventricular or aortico-pericardial fistula formation. The incidence of perivalvular extension ranges from 10% to 30% in native valve IE and 30% to 55% in prosthetic valve endocarditis [2]. This involvement of valve and annulus in IE occurs by direct extension due to the anatomic vulnerability of the aortic valve and its surrounding structures [3]. Aortic root abscess may lead to persistent sepsis, heart failure, conduction abnormalities, fistula formation and unprecedented risk to life [4].
IE should be suspected in any patient with aortic valve disease who fails to improve within 72 hours on appropriate antibiotics. Non resolution of fever, persistently elevated white blood cell counts, skin manifestation and embolic episodes with the raised biochemical markers of systemic inflammation points towards uncontrolled infection [5].
TTE is a sensitive tool to diagnose valvular vegetations preoperatively, the haemodynamics of valvular regurgitation, and presence of aortic root abscess [6]. The sub-aortic zone of the aortic mitral continuity and the anterior mitral leaflet should be assessed in patient with suspicion of endocarditis of the aortic valve. Altered morphology at the base of anterior mitral leaflet, should alert the clinician to the possibility of these complications which was not suspected in our case as the patient did not have any features of IE. TEE also provides superior anatomical definitions like the extent of annular involvement, extension of abscess to involve the sub-aortic curtain or upper inter-ventricular septum and for planning surgery [7].
Once an aortic root abscess is detected, it is a surgical emergency. Aggressive debridement of all infected and devitalised tissue is the mainstay of the surgical treatment of aortic root abscess. Reconstruction of the left ventricular outflow tract with autologous pericardium or translocation of the aortic valve may also be required. However in our patient there were no signs of IE and the patient was not having any other comorbid illnesses such as tuberculosis, or other immunocompromised illnesses. Young patients mask a multitude of signs and present with subtle symptoms given good physiological reserve.
Conclusion
Aortic root abscess is a dreadful complication of valvular disease and should be suspected if there is any altered valvular morphology depicted on echocardiogram. The signs of sepsis may be masked in young individuals due to good physiological reserve. A proper plan for surgery in these groups of patients favours good outcome postoperatively.
[1]. Revilla A, López J, Vilacosta I, Villacorta E, Rollán MJ, Echevarría JR, Clinical and prognostic profile of patients with infective endocarditis who need urgent surgeryEur Heart J 2007 28(1):65-71. [Google Scholar]
[2]. Graupner C, Vilacosta I, San Roman JA, Ronderos R, Sarriá C, Fernández C, Periannular extension of infective endocarditisJournal of the American College of Cardiology 2002 39(7):1204-11. [Google Scholar]
[3]. Kang N, Wan S, Ng CS, Underwood MJ, Periannular extension of infective endocarditisAnnals of Thoracic and Cardiovascular Surgery 2009 15(2):74-81. [Google Scholar]
[4]. Panduranga P, Aortic root abscess presenting as pyrexia of unknown origin and the importance of echocardiographyCase Reports in Critical Care 2013 :01-03. [Google Scholar]
[5]. Larry MB, Walter RW, Arnold SB, Vance GF, Ann FB, Matthew EL, Infective EndocarditisCirculation 2005 111:e394-e434. [Google Scholar]
[6]. Molnar A, Diana S, Simona M, Amanda R, Ruxandra B, The value of transthoracic and transesophageal echocardiography for the diagnosis of the native aortic infective endocarditis valve complications: a case report and literature reviewMedical Ultrasonography 2016 18(2):253-56. [Google Scholar]
[7]. Hill EE, Herijgers P, Claus P, Vanderschueren S, Peetermans WE, Herregods MC, Abscess in infective endocarditis: the value of transesophageal echocardiography and outcome; A 5-year studyAm Heart J 2007 154(5):923-28. [Google Scholar]