Retained Foetal Bones with Recurrent Vaginal Discharge: A Case Report
Samarth Virmani1, Deeksha Pandey2, Pranadeep Inukollu3, Jyothi Shetty4, Ishan Sardesai5
1 MBBS Student, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal University, Manipal, Karnataka, India.
2 Associate Professor, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal University, Manipal, Karnataka, India.
3 Senior Resident, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal University, Manipal, Karnataka, India.
4 Professor, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal University, Manipal, Karnataka, India.
5 MBBS Student, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal University, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deeksha Pandey, Associate Professor, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal University, Manipal-576104, Karnataka, India.
E-mail: deekshiiiobg@gmail.com
Termination of pregnancy or abortion is rarely known to result in retained foetal bones. The presentation of a patient with retained foetal bones may be in the form of secondary infertility, chronic pelvic pain, dysmenorrhoea, menorrhagia, etc is common. It is a rare occurrence to have retained foetal bones presenting in the form of recurrent vaginal discharge. The following is a case report of a female who presented with vaginal discharge and was later diagnosed to have retained foetal bones.
Dysmenorrhoea, Menorrhagia, Termination of pregnancy
Case Report
A 38-year-old woman, with parity index G2P1Ab1, came to the gynaecological outpatient department with complaints of vaginal discharge since two months. The patient complained of scanty white foul smelling vaginal discharge that was present throughout the day since two months and subsequently got increased since two weeks prior to presentation. She also complained of abdominal pain since two months that was diffuse in nature, present intermittently, which increased since two weeks prior to presentation, with no aggravating or relieving factors. There were no complaints of fever, dysmenorrhoea, dyspareunia, irregular bleeding, etc. She gave history of similar episodes of foul smelling discharge per vagina occurring about once a year since the past six years which was managed by oral medications at a local rural hospital. Her last child birth was 13 years ago by a normal vaginal delivery, and there were no antenatal or postnatal complications. She conceived for the second time eight years ago and underwent medical termination of pregnancy at 16 weeks of gestational age at a rural hospital in view of anencephaly of the foetus. She has no history of tuberculosis or other significant medical or surgical history.
On examination, the patient’s general condition appeared normal, and her vitals were stable. Her systemic examination including cardiovascular system, central nervous system, and respiratory system was normal. On abdominal examination, there was no abdominal distension, and the abdomen was soft and non-tender on palpation. On per speculum examination, the cervix was healthy but there was non-foul smelling curdy white discharge present. On per vaginal examination, the uterus was anteverted, normal in size, mobile, non-tender, and fornices were free.
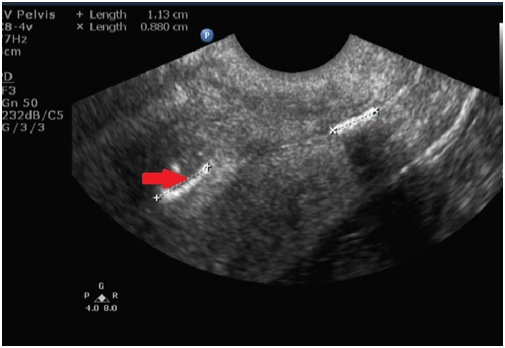
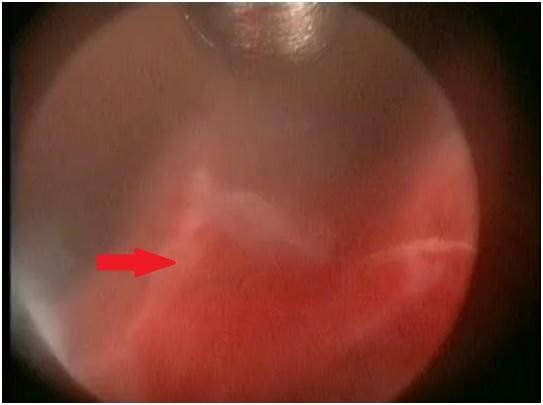
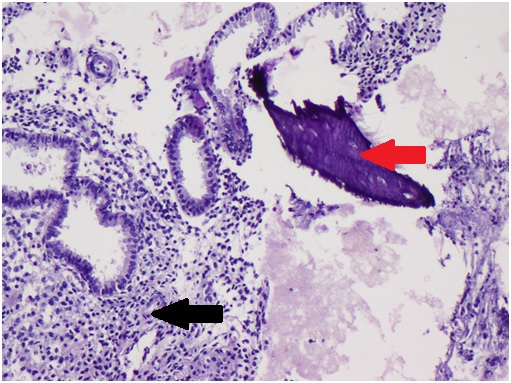
A Papanicolaou (PAP) smear was taken which was found to be negative for intraepithelial lesion or malignancy. A transvaginal ultrasound was done which showed a uterus measuring 6.2 x 4 cm, endometrial thickness of 5 mm, evidence of echogenic lesion in the uterine cavity measuring (1.13x0.2) cm (suggestive of calcified mass in uterine cavity), right ovary measuring (2.5x2.0) cm, and left ovary measuring (3.1x3.2) cm [Table/Fig-1]. Subsequently, hysteroscopy was done under spinal anaesthesia, and the calcified tissue measuring about (1.1x0.2) cm was recovered and sent for histopathological examination [Table/Fig-2]. The histopathology was reported to be a specimen of single flattened bony tissue bit, weighing less than 1 gram, measuring (1.0x0.5) cm [Table/Fig-3]. The patient was started on oral antibiotics and metronidazole for five days. The patient was symptomatically better following hysteroscopic removal of mass, with decrease in abdominal pain and vaginal discharge. The patient was subsequently discharged following three days of observation upon complete resolution of pain and vaginal discharge.
Transvaginal ultrasound showing calcified mass in uterine cavity (Bony remnant) (red arrow).
Hysteroscopy showing bony remnants (red arrow).
Microscopy showing endometrial glands (black arrow) with bony remnant (red arrow).
Discussion
Retention of foetal bones in the uterine cavity is rare, with very few cases that have been reported in India [1]. This may occur following abortions which may be spontaneous, incomplete, missed, or therapeutic abortions. An increased risk of retention of bones is also seen in anomalous uterus [2]. Presence of bone in the uterine cavity may be due to other causes such as bony metaplasia of the endometrium with chronic inflammation, ossification and dystrophic calcification of the endometrium [3,4].
Periods of retention of bones for as long as 2-17 years [5] have been reported in literature and our patient was found to have retained foetal bone eight years following termination of pregnancy. It is more common to have incomplete evacuation of the uterus during termination in advancing gestational age [6] and with lack of ultrasound guidance during termination of pregnancy. Our patient had a termination of pregnancy without the use of ultrasound scan to confirm the expulsion of all products of conception, which may have led to retention of foetal bones.
The most common symptom of retention of foetal bones is secondary infertility, such that in many cases, retained foetal bones have been discovered during investigation for infertility [6,7,8]. Other less common symptoms include chronic pelvic pain, dysmenorrhoea, abnormal uterine bleeding, dyspareunia, etc. [9,10]. Our patient presented with foul smelling vaginal discharge which is a very rare presentation of retained foetal bones, with a similar case reported by Demirtas O et al., [11].
Associated chronic pelvic pain is probably as a result of the increased levels of prostaglandins due to the retained foetal bones. In a study by Lewis V et al., increased menstrual prostaglandin E levels were found in females with retained foetal bones which got decreased following removal of the foetal bones [12].
A transvaginal ultrasound scan is usually the first modality chosen to investigate patients with infertility and abnormal uterine bleeding following abortion, to rule out the possibility of retained products of conception. Differential diagnoses such as Asherman’s syndrome, intrauterine device, calcified submucous fibroids, etc. have to be ruled out on the basis of history, ultrasound findings, hysteroscopy and histopathological examination [11]. In our case, history of medical termination of pregnancy was suggestive of retained foetal bones. Visualization of a hyperechogenic focus on the scan within the uterine cavity is usually suggestive of presence of a foreign body or bony fragments [13]. Upon detection of the foreign body, hysteroscopy can be done to confirm the presence and remove the foreign body from the uterine cavity [14]. If the scan does not show the presence of foreign body despite high suspicion of the same, a hysteroscopy can be done to establish the diagnosis and remove the foreign body or bony fragments [15,16]. Retained foetal bones are found in around 0.15% of patients undergoing diagnostic hysteroscopy [17]. Since, hysteroscopy is not available in some centres, especially in developing countries, a blind dilatation and evacuation of products of conception can be done, and subsequently be confirmed by ultrasound scan.
Bahceci M and Demirel LC reported return of fertility following removal of retained products of conception 12 years following abortion, and Moon HS et al., reported return of fertility in 10 out of 11 women following removal of products of conception. The prognosis of patients following removal of bony fragments is very good, since most women have a normal pregnancy following removal of the intrauterine bones, despite having a long period of infertility [3,7].
Conclusion
A female presenting with recurrent episodes of vaginal discharge should be evaluated further if she has a history of an abortion or medical termination of pregnancy. An ultrasound scan is necessary in order to visualise uterine pathology in such patients who present with recurrent episodes of vaginal discharge despite following syndromic management. This is especially important in developing countries where most women with vaginal discharge are treated by syndromic management without the use of an ultrasound scan. It is of utmost importance for the doctor to suspect this condition and diagnose it by ultrasound scan and hysteroscopy.
[1]. Singla A, Gupta B, Guleria K, First Trimester Abortion: A Rare Cause of Intrauterine Bony SpiculesCase Reports in Obstetrics and Gynaecology 2012 2012:701021 [Google Scholar]
[2]. Melius FA, Julious TM, Nagel TC, Prolonged retention of intrauterine bonesObstet Gynecol 1991 78(5 pt. 2):919-921. [Google Scholar]
[3]. Bahceci M, Demirel LC, Osseous metaplasia of the endometrium: a rare cause of infertility and its hysteroscopic managementHum Reprod 1996 11:2537-2439. [Google Scholar]
[4]. Acharya U, Hamilton MPR, Osseous metaplasia of the endometrium treated by hysteroscopic resectionBr J Obstet Gynaecol 1993 100(4):391-92. [Google Scholar]
[5]. Saahinoglu Z, Kuyumcuoglu U, An unusual case of postmenopausal vaginal bleeding: retention of fetal boneArch Gynecol Obstet 2003 267(3):160-162. [Google Scholar]
[6]. Harman CR, Fish DG, Tyson JE, Factors influencing morbidity in termination of pregnancyAm J Obstet Gynecol 1981 139(3):333-337. [Google Scholar]
[7]. Moon HS, Park YH, Kwon HY, Hong SH, Kim SK, Iatrogenic secondary infertility caused by residual intrauterine fetal bone after midtrimester abortionAm J Obstet Gynecol 1997 176(2):369-370. [Google Scholar]
[8]. Panama S, Triolo O, Arezio P, Prolonged retention of fetal bones: intrauterine device and extrauterine diseaseClin Exp Obstet Gynecol 1990 17(1):47-49. [Google Scholar]
[9]. Verma U, Chong D, Perez I, Medina C, Fetal bones retained in the uterine cavity as a rare cause of chronic pelvic pain: a case reportJ Reprod Med 2004 49(10):853-855. [Google Scholar]
[10]. Gupta N, Singh N, Mittal S, Misra R, Dadhwal V, Intrauterine retention of fetal bones: an unusual cause of pelvic painJ Obstet Gynecol India 2009 59(6):584-585. [Google Scholar]
[11]. Demirtas O, Terzi H, Kale A, Sanibrahim B, Guler O, A rare and unexpected case of retained foetal bone after an unsafe abortionJ Pak Med Assoc 2015 65:1119-1120. [Google Scholar]
[12]. Lewis V, Khan-Dawood F, King M, Beckham C, Dawood MY, Retention of intrauterine foetal bones increases menstrual prostaglandinsObstet Gynecol 1995 75(3 Pt 2):561-563. [Google Scholar]
[13]. Dawood MY, Jarret JC, Prolonged intrauterine retention of fetal bones after abortion causing infertilityAm J Obstet Gynecol 1982 143(6):715-7. [Google Scholar]
[14]. Cepni I, Kumbak B, Ocal P, Idil M, Aksu F, Infertility due to intrauterine residual fetal bone fragmentsJ Clin Ultrasound 2004 32(5):253-255. [Google Scholar]
[15]. Torne A, Jou P, Pangano R, Sanchez I, Ordi J, Vanrell JA, Endometrial ossification successfully treated by hysteroscopic resectionEur J Obstet Gynecol Rerod Biol 1996 66(1):75-77. [Google Scholar]
[16]. Louis LS, Kingman CEC, Cochrane GW, Heterotopic intrauterine bone formationJ Obstet Gynaecol 2007 27(2):208-9. [Google Scholar]
[17]. Makris N, Stefanidis K, Loutradis D, Anastasiadou K, Hatjipappas G, Antsaklis A, The incidence of retained fetal bone revealed in 2000 diagnostic hysteroscopiesJ Soc Laparoendo Surg 2006 10(1):76-77. [Google Scholar]