A Case of True Hemaphroditism Presenting with Dysgerminoma
Manika Khare1, Manish Kumar Gupta2, Ashish Airun3, Umesh Babu Sharma4, KM Garg5
1 Assistant Professor, Department of Pathology, JNUIMSRC, Jaipur, Rajasthan, India.
2 Assistant Professor, Department of Surgery, JNUIMSRC, Jaipur, Rajasthan, India.
3 Tutor, Department of Pathology, JNUIMSRC, Jaipur, Rajasthan, India.
4 Professor, Department of Pathology, JNUIMSRC, Jaipur, Rajasthan, India.
5 Professor, Department of Surgery, JNUIMSRC, Jaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manika Khare, 3/293, Malviya Nagar, Jaipur-302017, Rajasthan, India.
E-mail: drmanika09@gmail.com
The true hermaphroditism represents only 5% of all disorders of sexual differentiation, thus it is one of the rarest varieties. Diagnosis of true hermaphroditism requires the presence of both ovary and testis either as separate organs or combined to form unilateral or bilateral ovotestis. Dysgerminoma is one of the tumours which are commonly seen in true hermaphrodites. The main treatment modality includes removal of the dysgerminoma followed by chemotherapy if the tumour is Ib-IV stage So, early diagnosis of hermaphrodite and associated tumours can help the patient to lead a better life ahead as enlarged tumours have more aggressive treatment and are associated with poor prognosis. We are presenting this case because true hermaphrodites are themselves rare, and association with germ cell tumours is still rarer. This case is still special as the diagnosis of true hermaphrodite was made during surgery only.
Hermaphrodite, Ovarian tumour, Rare
Case Report
A 26-year-old male presented with chief complaint of primary infertility. On examination all secondary sexual characters were present. Genital examination showed empty scrotum, no testis was palpable. Semen analysis showed azoospermia. USG abdomen was done which showed left testis present in the pelvis and right testis was present in the right inguinal region. Along with this MRI abdomen was done which showed a large prevertebral hypoechoic mass lesion in umbilical region with ascites, and further confirmed the presence of testis on same site [Table/Fig-1]. For further confirmation CT abdomen was done which showed a large lobulated heterogenous mass in a suprapubic region with necrotic foci measuring 97 x 90 x 132 mm. Hormonal studies showed FSH, LH and testosterone levels within normal levels. Surgery of the patient was planned which showed a uterus with attached bilateral ovaries with massively enlarged left sided ovary measuring 15 cm in diameter [Table/Fig-2].
MRI image showing bilateral testis in inguinal canals with separately lying pelvic mass.

Photograph shows intraoperative large ovarian mass.

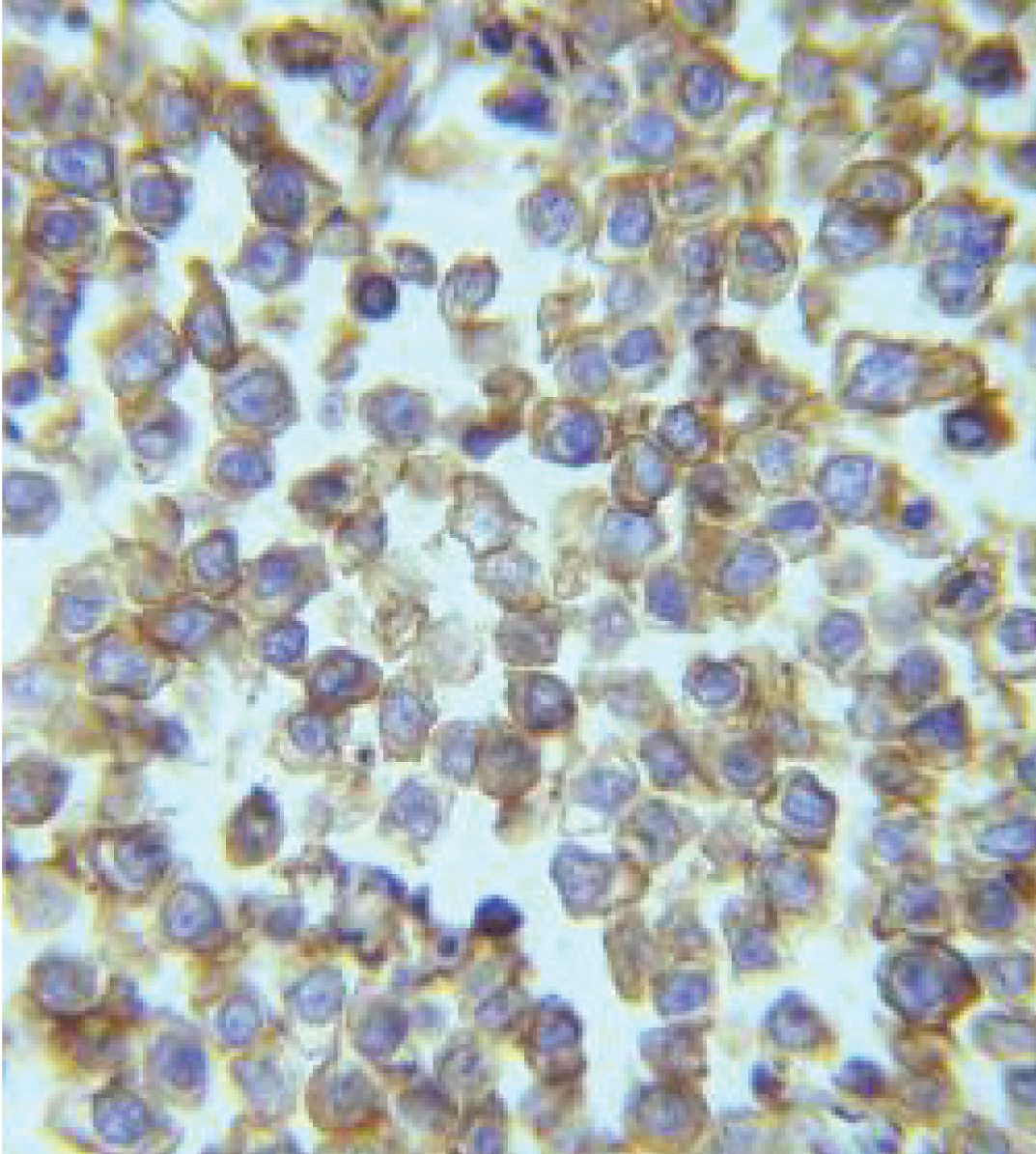
Left ovary with attachéd fallopian tube was removed and was sent for histopathological examination. Grossly ovary was massively enlarged; cut section was grey white with necrotic areas [Table/Fig-3]. Microscopic examination showed tumour cells arranged in sheets with interlacing thin fibrous band infiltrated with lymphocytes. Cells were polygonal with round nucleus with prominent nucleoli and abundant clear cytoplasm [Table/Fig-4,5]. Tumour cells showed membranous positivity for CD117 [Table/Fig-6]. On the basis of microscopic and immunochemical findings diagnosis of dysgerminoma left ovary was given. Section from fallopian tube confirmed fallopian tube microscopically. Patient is doing well now; he has received three cycles of chemotherapy.
Photograph shows cut section of the gross specimen of left ovary with areas of necrosis.

Photomicrograph showing tumour cells arranged in sheets with polygonal cell having clear cytoplasm round nucleus with prominent nucleoli (H&E 40X).
Showing tumour cell morphology on 100 X with a prominent nucleoli (H&E 100X).

Photomicrograph showing strong membranous CD117 positivity in tumour cells (IHC 40X).
Discussion
The term Disorder of Sexual Differentiation (DSD) refers to a child born without clear male or female phenotype [1]. True hermaphroditism represents only 5% cases of all of DSD, thus it is one of the rarest varieties. The gonads in a true hermaphrodite are asymmetrical and have both ovarian and testicular differentiation on either side separately or combined as an ovotestis [1]. These individuals are usually detected in their early childhood but when detected late have a great psychological impact on the individual along with this risk of have gonadal neoplasm is raised [2].
Diagnosis of true hermaphroditism requires the presence of both ovary and testis either as separate organs or combined to form unilateral or bilateral ovotestis. The rarity may be because most of the fetuses do not survive the intrauterine environment [3]. Individuals presenting with even minor ambiguity in the external genitalia and unilateral or bilateral undescended testicles should be investigated [4].
In a hermaphrodite, tumour can arise either from ovarian tissue or testicular tissue; often the gonads are destroyed so that site of origin cannot be determined. The descent and position of the gonad is dependent on the amount of testicular tissue present [5]. A 50% of the ovotestes are found in an abdominal position, while 25% are in the inguinal region. The other 25% are labioscrotal in position. An 85% of ovaries are found in the abdomen and 50% of the testes are labioscrotal [5]. The type of internal genitalia found depends on the nature of the adjacent gonad [6].
The incidence of germ-cell neoplasms is higher in true hermaphrodites with 46,XY karyotype and with other chromosome complements containing a Y chromosome, most frequently 46,XX/46,XY than in those with a 46,XX karyotype [7]. The risk of malignancy ranges from 2.6% to 4.6%, although in true hermaphrodites it is lower than in other types of DSD [8]. Dysgerminoma is one of the tumour which is commonly seen in true hermaphrodites. Meyer R reported 27 cases of the dysgerminoma in hermaphrodite [9]. In addition to hermaphrodite dysgerminoma can also be seen in persons with less striking sexual abnormalities, like male cryptorchidism and female hypoplasia of genital organs. Although germ-cell tumours are the most common neoplasms occurring in true hermaphrodites, a few cases of benign common epithelial tumours of the ovary, including mucinous and serous cystadenomas and Brenner tumours, have been also reported [10].
Imaging tests which are used for the diagnosis of true hermaphrodite are USG, MRI and genitography [11]. USG is the non invasive and easy procedure which should be used for the screening of such individuals. MRI and CT scan should be done in cases of unidentified gonads or lumps associated with the gonads as was seen in this case [12].
The main treatment modality includes removal of the dysgerminoma followed by chemotherapy if the tumour is Ib–IV stage. However, despite the large size of the tumour, there was no evidence of metastatic disease, supporting the view that dysgerminomas arising from gonadoblastomas have a lower metastatic potential than dysgerminomas arising de novo [13].
Conclusion
We are presenting this case because true hermaphrodite are themselves rare, association with germ cell tumours is still rarer. This case is still special as the diagnosis of true hermaphrodite was made during surgery only, so early diagnosis of hermaphrodite and associated tumours can help the patient to lead a better life ahead.
[1]. Iqbal MZ, Jam MR, Saleem M, Ahmed M, True hermaphrodite: a case reportAPSP Journal of Case Reports 2011 2:16 [Google Scholar]
[2]. Rangecroft L, British Association of Paediatric Surgeons Working Party on the Surgical Management of Children Born With Ambiguous Genitalia. Surgical management of ambiguous genitaliaArch Dis Child 2003 88:799-801. [Google Scholar]
[3]. Lee S, High incidence of true hermaphroditism in the early human embryosBiol Neonate 1971 18:418-25. [Google Scholar]
[4]. Kropp BP, Keating MA, Moshang T, Duckett JW, True hermaphroditism and normal male genitalia: an unusual presentationUrology 1995 46:736-39. [Google Scholar]
[5]. Barseghyan H, Vilain E, The genetics of ovotesticular disorders of sex developmentGenetic Steroid Disorders 2014 :261-63. [Google Scholar]
[6]. Ceci M, Callega E, Said E, Gut N, A case of true hermaphroditism presenting as a testicular tumourCase Rep Urol 2015 2015:598138 [Google Scholar]
[7]. Verp MS, Simpson JL, Abnormal sexual differentiation and neoplasiaCancer Genet Cytogenel 1987 25:191-218. [Google Scholar]
[8]. Montero M, Méendez R, Valverde D, Fernández JL, Gómez M, Ruíz C, True hermaphroditism and normal male external genitalia: a rare presentationActa Paediatrica 1999 88:909-11. [Google Scholar]
[9]. Meyer R, The pathology of some special ovarian tumours and their relations to sex characteristicsAm Jour Obstet and Gynec 1931 2:697 [Google Scholar]
[10]. Talerman A, Marion S, Senekjian E, Gilewski T, Vogelzang N, True hermaphrodite with bilateral ovotestes, bilateral gonadoblastomas and dysgerminomas, 46, XX/46, XY karyotype, and a successful pregnancyCancer 1990 66:2668-72. [Google Scholar]
[11]. Nanni L, Mirk P, Buonuomo V, Rinaldi P, Pintus C, Bonomo L, Ultrasonographic appearance of fallopian tube and ovotestis in a true hermaphroditeEuropean Journal of Radiology Extra 2008 66:e35-e37. [Google Scholar]
[12]. Mansour SM, Hamed ST, Adel L, Kamal RM, Ahmed DM, Does MRI add to ultrasound in the assessment of disorders of sex developmentEuropean Journal of Radiology 2012 81:2403-10. [Google Scholar]
[13]. Talerman A, Gonadoblastoma. In: Kurman RJ, edBlaustein’s Pathology of the Female Genital Tract 1987 ed. 3New YorkSpringer Verlag:704-09. [Google Scholar]