Aesthetics has become a respectable concept in dentistry as people are being more concerned of their appearance in today’s world. Malocclusion is one such condition for which patients seek treatment for because of its significant impact on function, aesthetics and psychological condition and we come across increased number of young adults who desire cost effective, non-surgical correction of these malocclusions in shortest possible time in our day-to-day practice. The optimal treatment for these malocclusions may include orthodontic therapy, orthognathic surgery, periodontics and fixed or removable prostheses. If the patients do not accept or undergo optimal dental treatment, other treatment modalities are to be considered. This article describes an aesthetic rehabilitation of class II malocclusion with a conservative interdisciplinary treatment plan tailored to the patient’s specific dental and skeletal problems, as well as considering her needs and desires.
Case Report
A 34-year-old female patient reported to the Department of Prosthodontics with the chief complaint of forwardly placed upper front teeth and missing lower front teeth and unpleasant smile. Patient had no significant medical conditions.
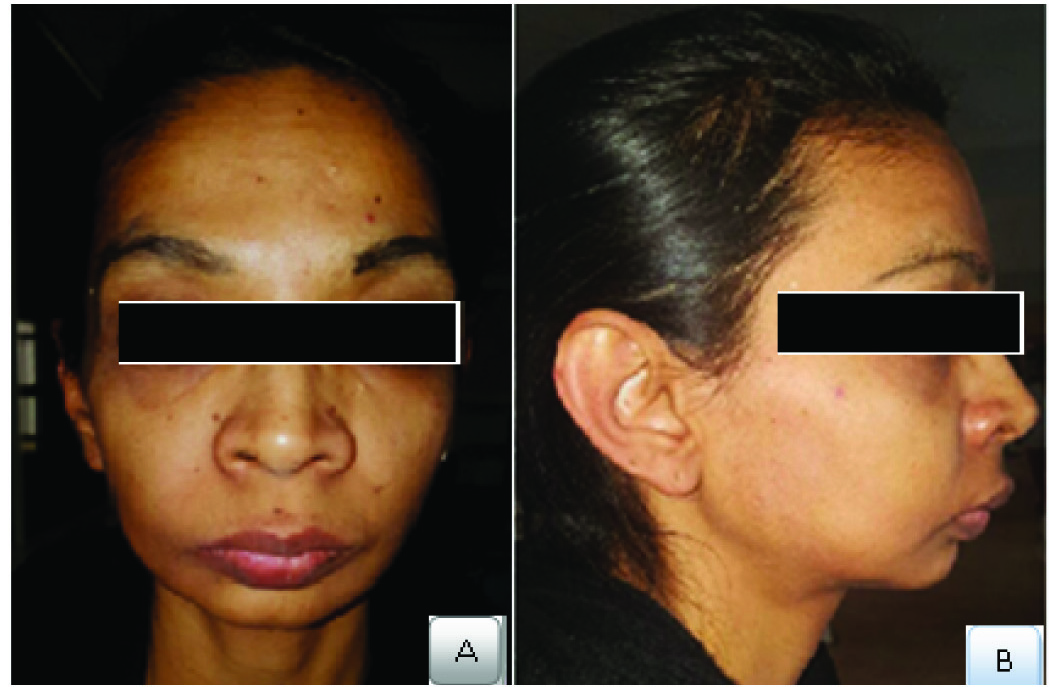
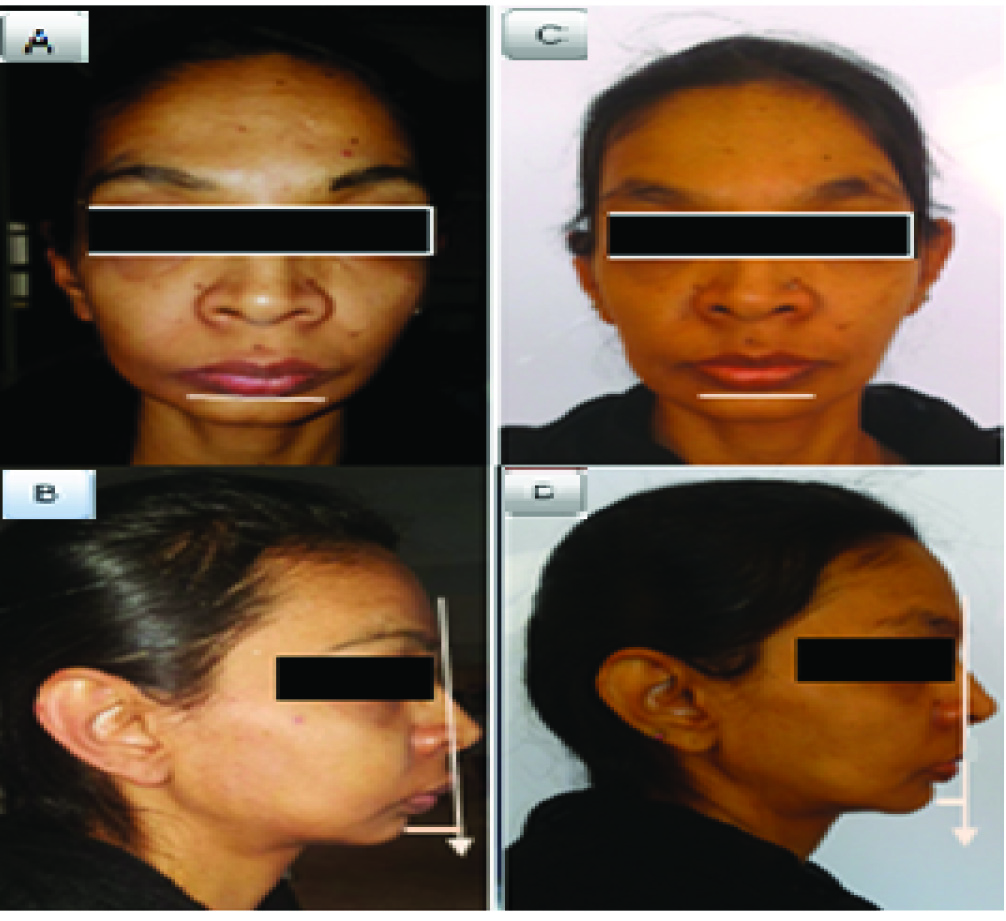
Extraoral examination revealed prognathic maxilla and retrognathic mandible [Table/Fig-1]. The patient showed good range of mandibular movements and no TMJ symptoms.
Pretreatment extraoral; A) Frontal profile; B) Lateral profile.
Intraoral examination [Table/Fig-2] showed Angle’s class II molar and canine relation with overjet of 12 mm and deep overbite of 7mm with tissue contact showing no signs of irritation and no interferences in centric relation position or excursive movements. Pronounced proclination of maxillary incisors with interdental spacing was observed. The maxillary canines were in supraocclusion and scissors bite was seen in premolars.
Preoperative intraoral view: A) frontal; B) right lateral; C) left lateral; D) maxillary; E) mandibular occlusal.
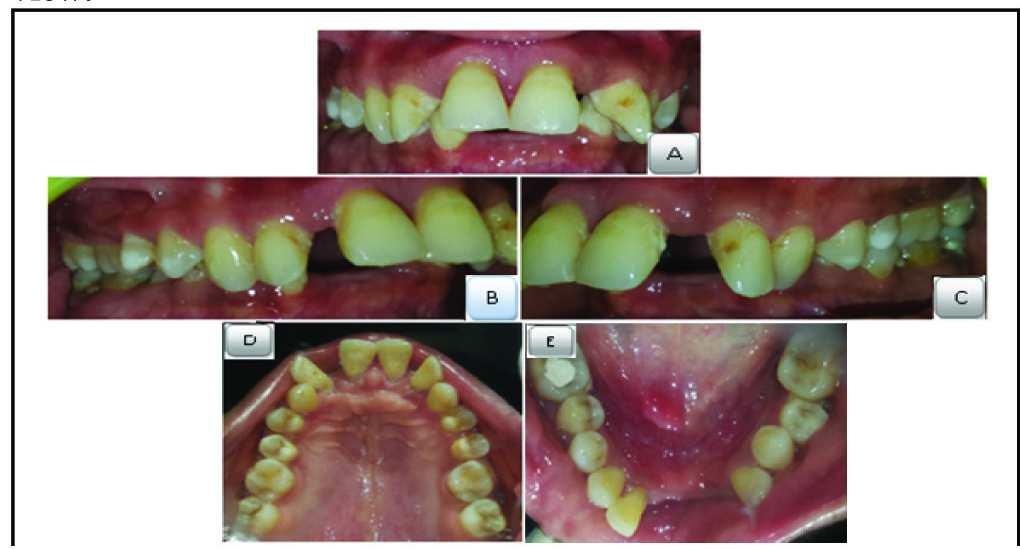
The right mandibular lateral incisor exhibited grade I mobility and other mandibular incisors were extracted due to poor periodontal support. The gingiva around remaining teeth bleed easily on probing and pockets were present in relation to maxillary and mandibular posterior teeth.
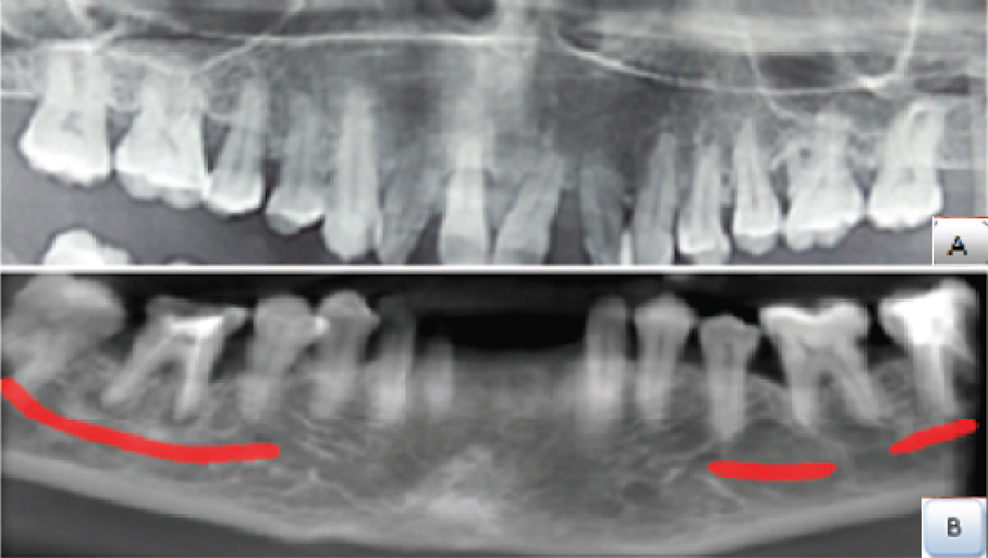
Radiographic evaluation showed generalized bone loss with maxillary and mandibular teeth. Cone Beam Computed Tomography (CBCT) revealed insufficient bone in maxillary anterior region for implant placement [Table/Fig-3]. Clinical diagnosis was generalized chronic periodontitis with class II malocclusion and deep bite.
CBCT view: A) Maxillary; B) Mandibular view.
After examining the patient’s existing clinical condition and radiographic evaluation, following treatment options were suggested:
Option-1: Periodontal regenerative therapy followed by orthodontic treatment and orthognathic surgery with maxillary set back (Le Fort I osteotomy) and mandibular advancement (Bilateral sagittal split osteotomy).
Option-2: Extraction of maxillary incisors followed by Fixed Partial Denture (FPD) with abutment support extending upto first premolars on both sides in maxilla and FPD extending from canine to canine in mandible or extraction of mobile lateral incisor #42 followed by implant supported FPD replacing missing mandibular incisors.
The patient opted for FPD as the patient was reluctant to undergo through time consuming and extensive surgical procedures involved in other options.
Treatment Objectives and Procedures
The treatment goals were to control the periodontal inflammation, stabilize the dentition, correcting proclined teeth and replacing missing teeth with FPD, ultimately enhancing the patient’s Aesthetic appearance which was challenging in the present case as the patient had skeletal class II relation and was not willing to undergo orthodontic or orthognathic procedure. So, the treatment plan was developed to restore the malocclusion and also improve the facial profile.
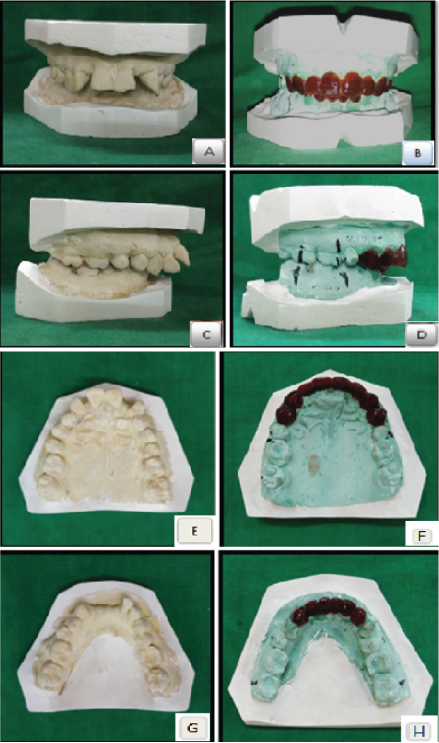
First, diagnostic casts were obtained and mock preparation was done on maxillary canines and first premolar extracting incisors and alveoloplasty of around 2mm was performed on the cast and diagnostic wax patterns were made to facilitate development of aesthetics which showed a definitive improvement [Table/Fig-4].
Preoperative cast: A,C,E,G) and wax up (B,D,F,H) Frontal (A,B), Lateral (C,D) and Occlusal (E,F,G,H) view.
So, the final treatment plan executed was as follows:
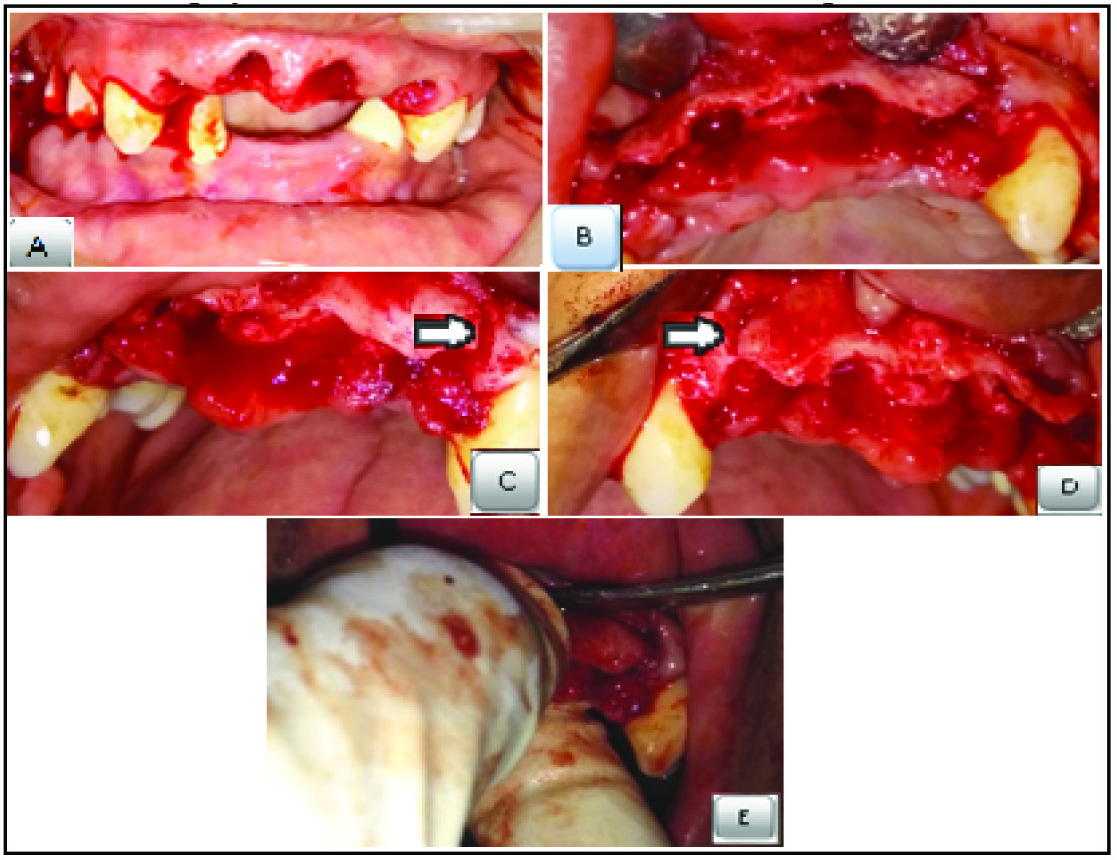
Periodontal treatments including oral prophylaxis and subgingival curettage were performed on both arches, followed by flap surgery for posterior teeth. After the periodontal condition was stabilized, after about 2 months (oral prophylaxis and curettage for 4 weeks; flap surgery for 4 weeks), extraction of maxillary incisors was done followed by Dean’s intraseptal alveoloplasty [Table/Fig-5]. A removable partial denture was fabricated in accordance with the mock-up done during the healing period and checked for aesthetics, phonetics and function. After the patient was satisfied, FPD procedure was initiated following healing of soft tissues at 4 weeks. Prophylactic endodontic treatments were performed w.r.t #13,#23,#42. Tooth preparation was done w.r.t #13,#14,#23,#24,#33,#42,#43 to receive all ceramic crowns [Table/Fig-6]. Provisional restorations were fabricated and satisfactory anterior and canine guidance were established simultaneously checking for aesthetics, phonetics and function. Then, final restorations were fabricated taking provisional’s as template [Table/Fig-7].
Dean’s intraseptal alveoloplasty: A) Extraction of centrals and laterals; B) Interseptal bone cut; C) Vertical cut given at extraction socket and canine on left side; D) Vertical cut given at extraction socket and canine on right side; E) Digital pressure applied for compressing sockets.
Tooth Preparation: A) Maxillary occlusal view; B) Mandibular occlusal view; C) Frontal view

Permanent restorations cemented: A) Frontal view; B) Right lateral view; C) Left lateral view; D) Maxillary occlusal view; E) Mandibular occlusal view.

As the patient also had a retrognathic mandible, to improve facial profile, chin implant was planned. A porous polyethylene chin implant (BIOPORE™ CHIN IMPLANT, BIOPORE™ Surgicals) that best suits patient’s profile was selected based on lateral cephalometric analysis [Table/Fig-8] and put in place with titanium screws to enhance or reshape the size of chin [Table/Fig-9,10], thus achieving pleasing appearance [Table/Fig-11].
Lateral cephalogram before the placement of chin implant.

Chin implant placed. (Images from left to right)

Postoperative lateral cephalogram.

Preoperative A,B); and postoperative; C,D) frontal and lateral view.
A one year follow up was done with no appreciable changes at the treatment site and the patient was fully satisfied with the improved aesthetic outcome.
Discussion
Aesthetics in dentistry is becoming prominent day by day, making it imperative for a clinician to adopt Aesthetics in his/her practice, joining hands with other specialists to optimize the treatment outcome. The desire for a more aesthetic smile has become one of the most powerful incentives for a visit to the dentist and malocclusion is one such condition that affects aesthetics [1].
Correction of skeletal Class II malocclusion through prosthodontics without involving orthodontics and orthognathic surgery is one such difficult restorative challenge faced in clinical practice [2]. Restorative results can be disastrous if pitfalls are not recognized and addressed in the treatment plan.
Patients with skeletal Class II are typically treated with orthodontics followed by orthognathic surgery depending on severity of malocclusion [3].
A magnificent orthodontic treatment can be destroyed by poor periodontal support. In the present case, as there was inadequate bone support, bone grafting had to be preceded by orthodontics. A healing period of 4-6 months was required after regenerative periodontal therapy before initiating an orthodontic therapy [4]. Correction of skeletal class II malocclusion would require orthodontic therapy followed by orthognathic surgery [5], whole procedure taking a time period of 24-30 months, which the patient was not willing to go for.
CBCT showed insufficient bone for the placement of implants in maxilla and needed bone graft prior to implant placement. Since the maxilla was prognathic, placement of implants and subsequent prosthesis would also not yield desired aesthetic results.
As there was no occlusal instability in the present case, (occlusal interferences in centric and eccentric movements verified clinically) correction of such stable malocclusion was aimed at mainly improving aesthetics [6]. In this scenario, FPD was the only option through which aesthetic improvement had to be brought about. For this, a proper diagnostic wax-up prior to the start of treatment is essential. Diagnostic wax-up is the process of converting a programmed treatment plan into a three-dimensional visualization and acts as the best visual aid for the patient to understand the goals of treatment [6]. With the pre-evaluation temporaries in place, the aesthetics, the phonetics and even the occlusion can be evaluated and necessary corrections be made [7]. Therefore, a diagnostic wax-up was made following extraction of incisors and alveoplasty of around 2 mm, which showed a definitive improvement.
Dean’s intraseptal alveoloplasty was carried out following extraction of incisors. It is a technique usually done in maxillary anterior region immediately after extraction to reduce gross maxillary overjet [8,9]. After extracting incisors, interseptal bone was cut followed by vertical cuts in the labial cortex at distal end of the extraction sockets bilaterally. Next, labial cortex was fractured and compressed in approximation with palatal plate and then sharp margins were removed and sutures placed. Immediate removable partial denture was placed during healing period.
In the present case, we had opted for zirconia restorations, as ceramics best mimic the natural tooth due to their advantages like natural look, superior strength, high fracture toughness, high resistance to crack propagation, biocompatibility, durability etc., [10] and also as the patient’s chief complaint was aesthetics.
Chin augmentation with surgical implant provides better balance to the facial features by altering the underlying structure of the face. Chin implants, compared to other more popular surgeries, can be an excellent solution for individuals who wish to augment the size and shape of their chin without a major surgery. These chin implants build a better profile [11-13]. So, a chin implant was planned in the mandible as the patient had retrognathic mandible. This artificial implant sits under the skin and enhances the strength and definition of the chin, thus gives patients, a pleasing, well-proportioned look that seems completely natural.
Conclusion
This clinical report suggests a successful aesthetic anterior rehabilitation of a patient with complex class II malocclusion, in which interdisciplinary treatment planning improved facial harmony, and smile aesthetics, resulting in enhanced patient comfort and satisfaction through prosthetic and minimally invasive surgical procedures. This modality of treatment can be opted to improve facial aesthetics and occlusion in patients with dentoalveolar and skeletal defects who do not wish to undergo time consuming orthodontic therapy and complex surgical procedures.
[1]. McNamara L, McNamara JA Jr, Ackerman MB, Baccetti T, Hard- and soft-tissue contributions to the Aesthetics of the posed smile in growing patients seeking orthodontic treatmentAm J Orthod Dentofacial Orthop 2008 133(4):491-99. [Google Scholar]
[2]. Drago CJ, Caswell CW, Prosthodontic rehabilitation of patients with Class II malocclusionsJ Prosthet Dent 1990 64(4):435-45. [Google Scholar]
[3]. Proffit William R, Henry W. Fields, David M. Sarver, Contemporary Orthodontics 2007 St. Louis, MoMosby Elsevier [Google Scholar]
[4]. Zachrisson BU, Clinical implications of recent orthodontic-periodontic research findingsSemin Orthod 1996 2(1):04-12. [Google Scholar]
[5]. Pancherz H, Ruf S, Erbe C, Hansen K, The Mechanism of Class II Correction in Surgical Orthodontic Treatment of Adult Class II, Division 1 MalocclusionsAngle Orthod 2004 74(6):800-09. [Google Scholar]
[6]. Dawson PE, Functional Occlusion from TMJ to Smile Design 2007 St. Louis, MOMosby Elsevier [Google Scholar]
[7]. Gurel G, Discovering the artist inside: A three-step approach to predictable Aesthetic smile designs, Part IDent Today 2013 32(5):74:76-78. [Google Scholar]
[8]. Dean OT, Surgery for the denture patientJ Am Dent Assoc 1936 23:2124 [Google Scholar]
[9]. Steinhauser EW, Dean’s alveolotomy for the correction of maxillary protrusion with periodontal diseaseDtsch Zahnarztl Z 1976 31(3):232-34.[Article in German] [Google Scholar]
[10]. Agustín-Panadero R, Román-Rodríguez JL, Ferreiroa A, Sola-Ruiz MF, Fons-Font A, Zirconia in fixed prosthesis. A literature reviewJ Clin Exp Dent 2014 6(1):e66-e73. [Google Scholar]
[11]. Aufricht G, Combined plastic surgery of the nose and chin; resume of twenty seven years’ experiencesAm J Surg 1958 95(2):231-36. [Google Scholar]
[12]. Zide BM, Pfeifer TM, Longaker MT, Chin surgery: I. Augmentation-the allures and the alertsPlast Reconstr Surg 1999 104(6):1843-53. [Google Scholar]
[13]. Suman T, Enhancing facial aesthetics by other modalitiesInt J Dent 2011 2011:513957 [Google Scholar]