Case Report
A 12-year-old healthy male patient along with his father was referred from a remote area of Maharashtra to the Department of Conservative Dentistry and Endodontics with a chief compliant of pain in fractured upper front teeth. Patient had history of road side accidental fall four years back, due to which both of his upper front teeth were fractured. After the traumatic event, patient went to the local dentist for his dental treatment regarding toothache and loss of tooth structure. As the patient was economically poor and apprehensive, he had not taken any dental treatment at that time and took analgesics prescribed by the dentist for the temporary relief of pain. Since last one month patient had severe pain in his both upper front teeth and thus reported to our department for the dental treatment.
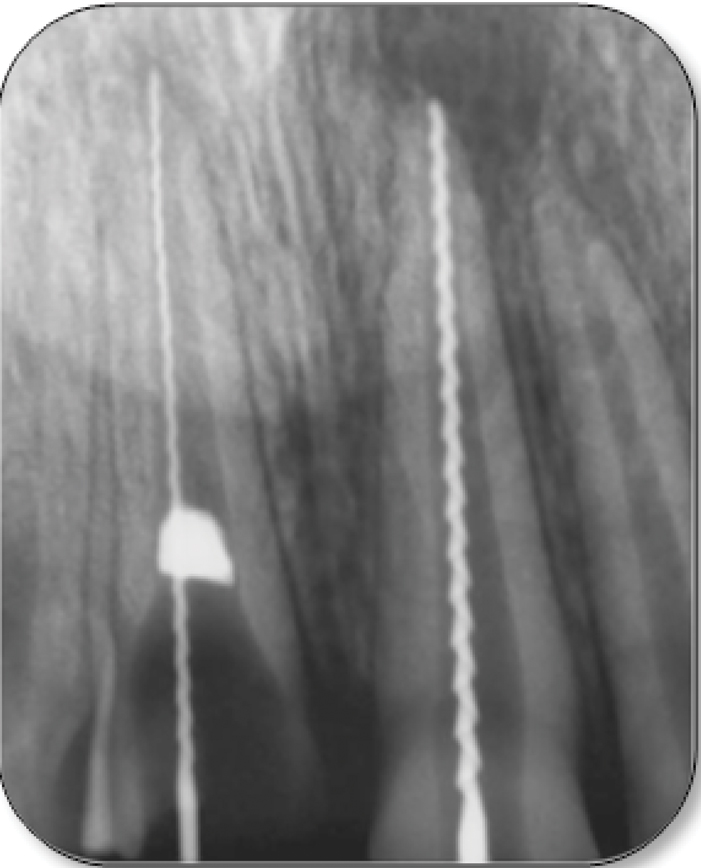
Clinical examination of the patient showed major loss of crown structure upto gingival level with gingival polyp in tooth #11 whereas, tooth #21 showed fractured incisal 1/3rd of the crown with discolouration [Table/Fig-1a,b]. Both teeth showed tenderness to percussion test and no response was seen on the electric pulp testing. Clinical examination confirmed Ellis Class IV fracture in teeth #11 and #21. Preoperative intraoral periapical (IOPA) radiographic examination revealed immature root apices with diffuse periapical radiolucency associated with tooth #11 and #21. Surprisingly an unusual, irregular radiopaque shadow was discovered in the cervical third of the root canal of tooth #11; indicating presence of some foreign body in the root canal [Table/Fig-2]. Patient and his father were willing to save the fractured teeth. After explaining the treatment protocol and long term prognosis of traumatised teeth to the patient and his father; we planned for functional and aesthetic rehabilitation of both maxillary central incisors with an endodontic, orthodontic and restorative multidisciplinary approach after obtaining their informed consent.
Preoperative labial view of mutilated #11 and fractured #21.

Preoperative palatal view of mutilated #11 and fractured #21.

Preoperative IOPA radiograph of teeth #11, #21 revealing radiopaque foreign object in the root canal of tooth #11.

Patient was scheduled for removal of the foreign object from the root canal of tooth #11, followed by single step apexification and completion of root canal treatment of teeth #11 and #21 using mixture of Bio-Oss and EMD. After root end barrier formation, root reinforcement was planned using fiber post and composite core build up in tooth #11. After composite core built up, extrusion of tooth #11 was initiated using removable orthodontic appliance. Once desirable extrusion of tooth #11 was achieved, aesthetic acrylic crowns were advised in teeth #11 and #21.
Patient was affirmative for the planned treatment but he was found to be very apprehensive and diagnosed as habitual mouth breather, thus rubber dam was not applied. Gingival polyp was excised after application of topical anesthetic gel. Under high vacuum suction and possible cotton roll isolation, access was achieved in teeth #11, # 21 and root canals were explored with No.10 K-file (Kerr file, MANI). The obstruction was felt in coronal 1/3rd of root canal of tooth #11, which confirmed the presence of some foreign object. The foreign object was bypassed with No. 25 H-file (Hedstrom) and working length was established using radiograph in teeth #11 and #21 [Table/Fig-3]. No. 25 H-file was inserted in the root canal of tooth #11 and the tip of activated scaler was kept in contact with coronal portion of the file for indirect ultrasonic vibrations. The intracanal foreign object was dislodged coronally due to ultrasonic vibrations and was retrieved using locking tweezer. The foreign object was found to be an irregularly shaped, transparent structure; suggestive of glass piece [Table/Fig-4]. An IOPA radiograph confirmed the complete removal of the foreign object from the root canal [Table/Fig-5]. Cleaning and shaping of root canals were done and canals were copiously irrigated using saline and 0.2% chlorhexidine using 27 gauge round ended, 2 side vented needle (Transcodent, Leur Lock 32mm long) to prevent extrusion of irrigant beyond the open apex. Intracanal calcium hydroxide (Metapex, Meta Biomed) was placed in both teeth #11 and #21 for about two weeks [Table/Fig-6] and access cavities were sealed with intermediate restorative material (IRM- Dentsply caulk).
Working length radiograph of teeth #11 and #21.
Retrieved foreign object (Glass piece) from tooth #11.

Confirmatory IOPA ensuring the removal of the foreign object from root canal of tooth #11.

IOPA radiograph of teeth #11and #21 after placement of calcium hydroxide with its slight extrusion through the apex of tooth #21.

After two weeks when patient was asymptomatic, root canals were irrigated with 0.2% chlorhexidine and dried with absorbable paper points. Apexification was attempted using a mixture of Bio-Oss (Geistlich Bio-Oss®) and EMD (Emdogain). Mixture was prepared by mixing Bio-Oss granules, EMD gel with sterile physiological saline in a mixing well and packed into the apical region of root with hand plugger with gentle pressure (Dentsply Maillefer, USA). Remaining intra canal space was obturated using thermo-plasticized gutta percha and AH Plus sealer (Dentsply Maillefer, USA) [Table/Fig-7] and access cavities were sealed using glass ionomer cement (GC Fuji, Type 2). For orthodontic extrusion of tooth #11 with removable appliance, impression was made and patient was recalled after a week for evaluation.
IOPA radiograph after apexification and root canal obturation of teeth #11, #21 showing progressive washout of apically extruded calcium hydroxide.

The post space was prepared in tooth #11 and the glass fibre, light transmitting post (Hi Rem PostTM, Overfibers) was cemented using dual cure resin cement (Relyx U200 3M SPE); followed by composite core (Luxacore, DMG) built up. An orthodontic bracket was bonded to the core of tooth #11 and extrusion was activated with removable orthodontic plate using elastics [Table/Fig-8]. Tooth was extruded approximately 0.5-1 mm per month and extrusion of 2.5 mm was achieved after three months [Table/Fig-9a]. To prevent relapse, supracrestal fibrotomy was performed in tooth #11. In this young patient as growth was not completed and occlusion was not established; fabrication of full jacket acrylic crowns were planned. Thus, teeth preparations were done in teeth #11, #21 and impression was made for fabrication of jacket crowns. A three months follow up radiograph showed reduction in periapical radiolucency in teeth #11, #21 [Table/Fig-9b].
Orthodontic extrusion of tooth #11 using removable appliance and elastic band at 3 months.
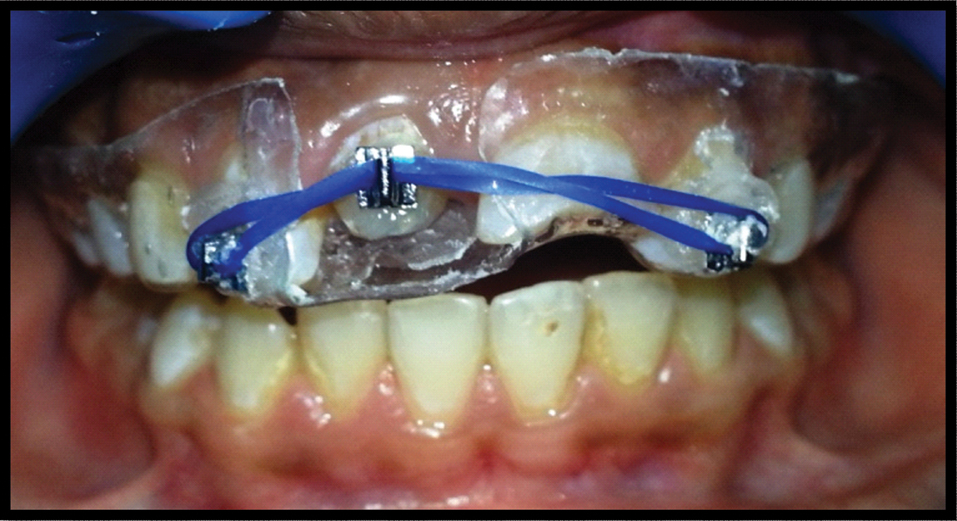
Clinical photograph after desired orthodontic extrusion in tooth #11.

IOPA radiograph showing composite core built up after fibre post cementation and reduction in periapical radiolucency in teeth #11 and #21.

On the same day, acrylic crowns were fabricated and cemented to teeth #11 and #21 [Table/Fig-10]. Patient was kept under regular follow up. Crowns were replaced after its fracture by the patient two times in between recalls. After three years of recall, teeth #11 and #21 were asymptomatic and presented in functional efficiency. IOPA radiograph showed decrease in size of periapical radiolucency in teeth #11 and #21 indicating the process of healing [Table/Fig-11] and multidisciplinary treatment success.
Intraoral labial view showing aesthetic acrylic crowns in teeth #11 and #21.

Three years follow up IOPA radiograph of teeth #11, #21 showing satisfactory periapical healing.

Discussion
Traumatic injury or caries to the young permanent tooth often results in loss of pulp vitality and infection, which interferes with the normal root formation and might also result in thin, fragile dentinal walls with wide open apices [1]. Thus, cleaning, shaping and obturation as well as post endodontic restoration of such tooth would become an endodontic challenge.
Treatment of non-vital tooth with an immature apex must be directed to induce a calcified barrier at the apical end which is called as ‘Apexification’ [2]. Various materials have been used for apexification and calcium hydroxide is the most commonly used material for this purpose. Though calcium hydroxide was used traditionally, it has been reported with several disadvantages such as, extended treatment period (6 to 24 months) with multiple clinical visits [1], incomplete and porous calcific barrier formation and dehydration of root dentin making it more susceptible to fracture [3].
Single step apexification procedure is therefore, suggested to overcome these limitations and various materials like tri-calcium phosphate, freeze dried bone, freeze dried dentin, collagen calcium phosphate, platelet plasma, hydroxyapatite and Mineral Trioxide Aggregate (MTA) have been advocated for single step apexification procedure [4,5]. Out of these materials MTA has proven to be clinically more acceptable and successful. Though, MTA is well known for its superior sealing ability, biocompatibility, regenerative capabilities and antibacterial properties; limitations like long setting time, poor handling characteristics, low resistance to compression, tendency to washout before its setting and relatively high cost have been reported [6]. Also, apexification with MTA does not increase the root length or dentinal thickness to resist the root fracture. To overcome these disadvantages, regenerative endodontic procedures have been introduced to replace the damaged pulp tissue with new vital tissue [7].
Pulp regeneration could be described as replacement of damaged tissue by identical cells to the lost tissue which leads to the complete re-establishment of biological function [8]. The pulp regenerative procedure is usually advised when the tooth is traumatised and the pulp tissue is not infected. Regenerative endodontics could be described as “Biologically-based procedures designed to physiologically replace damaged tooth structures which include dentin, root structures and cells of the pulp-dentin complex” [9]. Banchs F and Trope M in 2004, reported a case elaborating the procedure of revascularization in open apex using triple antibiotic paste (ciprofloxacin, metronidazole and minocycline) as intra canal medicament. In the next visit, after paste removal bleeding was induced into the canal and the canal was sealed with MTA followed by bonded restoration [10].
Researchers suggested that, for successful regenerative endodontic treatment root canals should be effectively disinfected and the coronal access must be effectively sealed. Additionally, a root apex of 1.1 mm in diameter or larger is advantageous, as the open apex allows the migration of mesenchymal stem cells into the root canal space to form new tissue in the root canal [11,12]. Case reports in the literature suggested that, regenerative endodontic procedures have found to be successful in 8-16 years age group patients; as in our case and it should not be attempted in deciduous teeth due to risk of interfering with eruption of its successor [13,14]. In the presented case, patient was from remote village area and unable to come for traditional multiple visit apexification treatment procedure, hence, root end maturation was accomplished by using combination of deproteinized bovine bone mineral (Bio-Oss) and Enamel Matrix Derivative (EMD).
Bio-Oss (Geistlich Bio-Oss®) is an osteoconductive material which is widely used in bone regenerative procedures and forms the scaffold to support the new tissue growth [15]. It is derived from a cancellous bovine bone, where the organic and pathogenic components are eliminated by chemical extraction [10,16]. EMD proteins are secreted by the Hertwig’s epithelial root sheath (HERS) during tooth development and help in regeneration of the Periodontal Ligament (PDL), cementum, bone and vascular supply by its stimulating activity. Commercially available EMD i.e., Emdogain not only helps in healing of endo-perio lesions but also proved to be beneficial in cases of re-implantation of tooth, tooth transplantation and bone formation in infra-bony defects. Emdogain consist of enamel matrix derivate, water and a carrier, i.e., propylene glycol alginate [17]. The exact composition of EMD is not accurately known but it contains the same proteins similar to those secreted by Hertwig’s epithelial cells. EMD also contains proteins such as enamelin, tufelin and ameloblastin [18].
EMD helps in cementogenesis, osteogenesis and the periodontal tissue regeneration [19]. In our case, a mixture of EMD and Bio-Oss was used considering their biocompatibility, synergistic action on cementogenesis, osteogenesis and the periodontal regeneration in combination [20-22]. The resultant mixture has good handling properties without the need of waiting for its complete set. However in some teeth, regenerative procedure may not be suitable in teeth requiring a post for adequate coronal restoration [23] as seen in our case and three years follow up showed adequate seal which has proven to be the part of the physiologic remodelling process.
In presented case, the discovery of a foreign object in the root canal was a surprising phenomenon and the radiopaque nature of foreign object raised the suspicion of metal or glass piece in the root canal. Use of indirect ultrasonic vibrations is considered to be less invasive and safe method while removing foreign object in the presence of thin dentinal walls. In teeth with inadequate crown structure; crown lengthening procedure or orthodontic extrusion is recommended over surgical extrusion, as it is more conservative and aesthetic method in order to maintain optimum biologic width. But, certainly it requires a relatively longer period for treatment and the patient’s cooperation for the optimum results. In our case, the tooth #11 was extruded with removable appliance being simple and cost effective method. As tooth #11 is associated with thin dentinal walls, it requires reinforcement. Fiber post being the good option due to their similar modulus of elasticity to the subjacent dentin and exhibit monoblock effect which ensures even force distribution with reinforcement [24]. As the growth of our patient is not completed, full coverage acrylic crowns were given. The patient was advised regular follow up with fabrication of permanent aesthetic crowns after completion of his growth.
Conclusion
Regenerative endodontic procedures have become the treatment of choice for immature permanent tooth with necrotic pulp even though thickening of the canal walls and continuation of root maturation are not always predictable. Bio-Oss and EMD have shown promising results in the presented case as it showed optimistic effects on the bone regeneration and biocompatibility to the surrounding tissues. Regenerative procedures may bring a new era in endodontics as an alternative treatment to the conventional root canal treatment. Regenerative endodontics for mature permanent teeth with necrotic pulps is still in the early stage of clinical trials. Further, clinical trials are required for evaluation of the results of regenerative endodontics and non-surgical root canal treatment for immature and mature teeth with necrotic pulps.
[1]. Neha K, Kansal R, Garg P, Joshi R, Garg D, Grover HS, Management of immature teeth by dentin-pulp regeneration: A recent approachMed Oral Patol Oral Cir Bucal 2011 16(7):e997-1004. [Google Scholar]
[2]. Morse DR, O’Larnic J, Yesilsoy C, Apexification: review of the literatureQuintessence Int 1990 21:589-98. [Google Scholar]
[3]. Ajwani P, Saini N, Non-surgical management of a mutilated maxillary central incisor with open apex and large periapical lesionIndian J Dent Res 2011 22(3):475-77. [Google Scholar]
[4]. Rossmeisl R, Reader A, Melfi R, Marquard J, A study of freeze-dried (lyophilized) cortical bone used as an apical barrier in adult monkey teethJ Endod 1982 8(5):219-26. [Google Scholar]
[5]. Hiremath H, Gada N, Kini Y, Kulkarni S, Yakub SS, Marquard J, Single-step apical barrier placement in immature teeth using mineral trioxide aggregate and management of periapical inflammatory lesion using platelet-rich plasma and hydroxyapatiteJ Endod 2008 34(8):1020-24. [Google Scholar]
[6]. Parirokh M, Torabinejad M, Mineral trioxide aggregate: a comprehensive literature review - Part III: clinical applications, drawbacks, and mechanism of actionJ Endod 2010 36(3):400-13. [Google Scholar]
[7]. Petrino JA, Boda KK, Shambarger S, Bowles WR, McClanahan SB, Challenges in regenerative endodontics: a case seriesJ Endod 2010 36(3):536-41. [Google Scholar]
[8]. Lin LM, Rosenberg PA, Repair and regeneration in endodonticsInt Endod J 2011 44(10):8891-906. [Google Scholar]
[9]. Glossary of Endodontic Terms, 8th edition [Internet]. Chicago: American Association of Endodontists, 2012. Available from: http://http://pages.nxtbook.com/nxtbooks/aae/endodonticglossary/offline/aae_endodonticglossary.pdf [Google Scholar]
[10]. Banchs F, Trope M, Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol?J Endod 2004 30(4):196-200. [Google Scholar]
[11]. Lovelace TW, Henry MA, Hargreaves KM, Diogenes A, Evaluation of the delivery of mesenchymal stem cells into the root canal space of necrotic immature teeth after clinical regenerative endodontic procedureJ Endod 2011 37(2):133-38. [Google Scholar]
[12]. Kim JY, Xin X, Moioli EK, Chung J, Lee CH, Chen M, Regeneration of dental-pulp-like tissue by chemotaxis- induced cell homingTissue Eng Part A 2010 16(10):3023-31. [Google Scholar]
[13]. Garcia-Godoy F, Murray PE, Recommendations for using regenerative endodontic procedures in permanent immature traumatized teethDent Traumatol 2012 28(1):33-41. [Google Scholar]
[14]. Chueh LH, Huang GT, Immature teeth with periradicular periodontitis or abscess undergoing apexogenesis: A paradigm shiftJ Endod 2006 32:1205-13. [Google Scholar]
[15]. Wong RWK, Rabie ABM, Effect of bio-Oss® collagen and collagen matrix on bone formationOpen Biomed Eng J 2010 4:71-76. [Google Scholar]
[16]. Rosen VB, Hobbs LW, Spector M, The ultrastructure of an organic bovine bone and selected synthetic hydroxyapatite used as bone graft substitute materialsBiomaterials 2002 23(3):921-28. [Google Scholar]
[17]. Bosshardt DD, Biological mediators and periodontal regeneration: a review of enamel matrix proteins at the cellular and molecular levelsJ Clin Periodontol 2008 35(suppl 8):87-105. [Google Scholar]
[18]. Zeichner-David M, Chen LS, Hsu Z, Reyna J, Caton J, Bringas P, Amelogenin and ameloblastin show growth-factor like activity in periodontal ligament cellsEur J Oral Sci 2006 114(Suppl 1):244-53. [Google Scholar]
[19]. Rathva VJ, Enamel matrix protein derivatives: role in periodontal regenerationClin Cosmet Investig Dent 2011 3:79-92. [Google Scholar]
[20]. Donos N, Kostopoulos L, Tonetti M, Karring T, Lang NP, The effect of enamel matrix proteins and deproteinized bovine bone mineral on heterotopic bone formationClin Oral Implants Res 2006 17(4):434-38. [Google Scholar]
[21]. Razavian H, Haerian A, Mosleh H, Novel apexification method in a non-vital tooth with an open apex: a case reportJ Dent (Tehran) 2014 11(3):371-78. [Google Scholar]
[22]. Pietruska MD, A comparative study on the use of Bio-Oss and enamel matrix derivative (Emdogain) in the treatment of periodontal bone defectsEur J Oral Sci 2001 109(3):178-81. [Google Scholar]
[23]. Saoud TMA, Ricucci D, Lin LM, Gaengler P, Regeneration and repair in endodontics- A special issue of the regenerative endodontics - A new era in clinical endodonticsDent J 2016 4(1):3 [Google Scholar]
[24]. Schmoldt SJ, Kirkpatrick TC, Rutledge RE, Yaccino JM, Reinforcement of simulated immature roots restored with composite resin, mineral trioxide aggregate, gutta-percha, or a fiber post after thermocyclingJ Endod 2011 37(10):1390-93. [Google Scholar]