Melena Secondary to Duodenal Dieulafoy’s Lesion: A Rare Case Report
Uthamalingam Murali1, Mohammad Azhar Anis Ahmad2, Ahmad Rahuddin Bin Abdul Hali3, Muhamad Afiq Hamidin4
1 Professor and Head, Department of Surgery, Anna Medical College, Mauritius.
2 Consultant Surgeon, Department of Surgery, Tengku Abdul Rahman Hospital, Shah Alam, Selangor, Malaysia.
3 MBBS Student, Department of Surgery, Management and Science University, Shah Alam, Selangor, Malaysia.
4 MBBS Student, Department of Surgery, Management and Science University, Shah Alam, Selangor, Malaysia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Uthamalingam Murali, Professor and Head, Department of Surgery, Anna Medical College, Sans Souci Road, Montagne Blanche-80906, Mauritius.
E-mail: srimuralihospital2012@gmail.com
Melena is one of the presenting feature of Upper Gastrointestinal Bleeding (UGIB). Melena due to Dieulafoy’s lesion in the duodenum is one of the obscure causes of Gastrointestinal Bleeding (GIB) and is a rare but life threatening entity. We report a unique case of Dieulafoy’s lesion in a 74-year-old male patient with premorbid condition of diabetes who presented with two episodes of blackish coloured stools, filling up the entire toilet bowl. No other symptoms of either abdominal pain, vomiting of blood, fever or any intake of medications were noted. Upper Gastro-Intestinal (UGI) endoscopy revealed abnormal vessels at D1/D2 of C loop duodenum with normal mucosa consistent with Dieulafoy’s lesion along with active bleeding. Haemoclips were applied to the duodenal Dieulafoy’s lesion and patient recovered well. This case was reported for the first time from Malaysia.
Blackish coloured stools, Haemoclip, Upper gastrointestinal bleeding
Case Report
A 74-year-old male with a premorbid condition of diabetes mellitus, on oral hypoglycaemic drugs diagnosed three years back presented with an episode of blackish hard stool of one day duration. On the day of admission, he had another episode of passing blackish coloured loose stools which made him feel lethargic and weak. The content was large in amount as it fully occupied the toilet bowl. There was no fresh blood noted in the stool. He also reported that he was having loss of appetite since one month and lost around 1 kg of his weight during the last week. No other symptoms of either abdominal pain, vomiting of blood, fever or any intake of medications were noted. Patient gave negative history for smoking and alcohol intake.
On clinical examination, he was conscious, anaemic but not in shock. His vital signs were within normal limits (pulse-86/minute and blood pressure-126/86 mmHg). On abdominal palpation, it was soft and non tender on all regions with no palpable mass. All other systemic examinations were normal. Rectal examination revealed fresh melena.
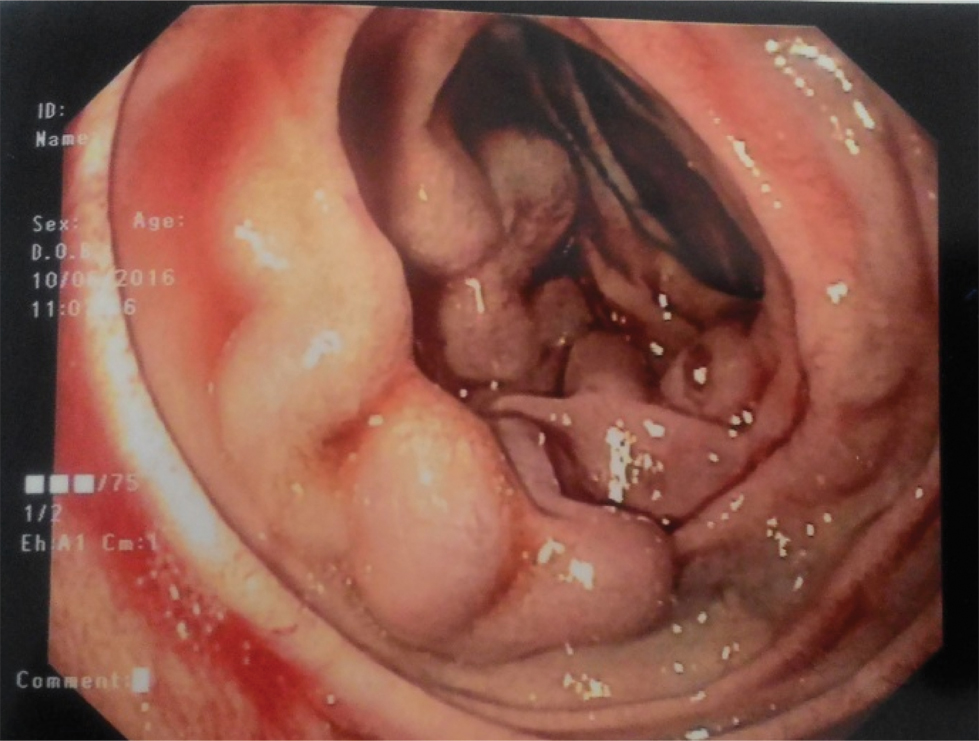
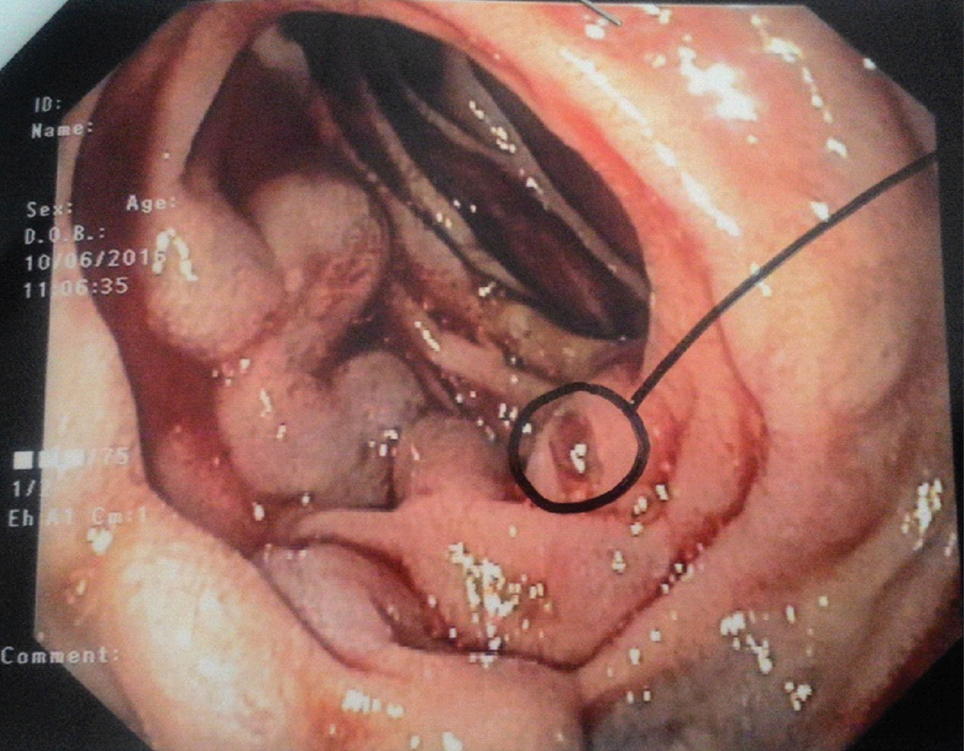
Clinically the diagnosis of UGIB was made. Later he was investigated to obtain the cause for UGIB. The significant laboratory reports showed: haemoglobin-6.1g/dL, RBC-count-1.94x106/μL, haematocrit-18%, and prothrombin time-14.5 seconds. His blood glucose levels were normal. Renal functions as assessed by measuring parameters like urea-13.4 mmol/L and creatinine-120 μmol/L were on the higher side. Other reports were normal. Chest X-ray and Electrocardiogram (ECG) were normal as well. Gastroscopy revealed abnormal vessels at D1/D2 of C loop duodenum suggestive of Dieulafoy’s lesion with evidence of active bleeding [Table/Fig-1,2].
Endoscopic findings suggestive of active bleeding at D1/D2 of C loop of duodenum with normal surrounding mucosa.
Upper gastrointestinal scopy shows close up endoscopic view of Dieulafoy’s lesion with mild mucosal defect.
He was immediately resuscitated with 4 units of packed cells and kept nil by mouth with nasogastric lavage. During gastroscopy haemoclip was applied to the dieulafoy’s lesion. Subsequently, he was treated with broad spectrum antibiotic with Proton Pump Inhibitor (PPI) for a week. The premorbid condition of diabetes was taken care of. The patient recovered well and was discharged after a week. The patient had a follow up for six months and was doing well.
Discussion
Acute UGIB is one of the common surgical emergencies in the world. Studies show an overall incidence of 50-100 per 100000 of the population per year around the world [1]. UGIB may be due to variceal or non-variceal sources. Dieulafoy’s lesion is one of the obscure causes of GIB and is a rare but potentially life-threatening entity [2]. It is also known as “persistent caliber submucosal artery”, accounting for 0.5-2% of acute GIB [3,4]. More than saying it as a rare case; it is not recognised due to its diagnostic challenge and silent nature until presentation, similar to the present case.
The aetiology of this condition is still not clear but two studies have tried to explain its origin. One of them have shown it to be congenital in origin [5] while other reports it as acquired lesion, more of aneurysmal variety [6]. In one of the case study stress has been observed [6] as a factor while in another study it was associated with the drugs such as aspirin, warfarin and non-steroidal anti-inflammatory drugs; however, there is no strong supportive evidence [7]. The incidence of Dieulafoy’s lesion is twice as high in men than in women. It can affect any age group, however it is seen more commonly in the elderly (7th decade) similar to our case [8]. Most patients presenting with Dieulafoy’s lesion have an active comorbid (medical illness) condition as evidenced in our patient with diabetes and the reported incidence is between 60-90% [8,9].
Two theories have been attributed towards the pathogenesis of Dieulafoy’s lesion [10]. First theory is that the rapid pulsations of sub-mucosal vessel occasionally leads to thinning out of the overlying epithelium, exposing it to the contents of bowel resulting in rupture. Second theory states that it is due to constant wear and tear of gastric vessels; which develop thrombosis within it, resulting in further necrosis. So the likely suggestion to the pathogenesis could be possibly age-related mucosal erosion or atrophy, as evident in this 74-year-old man [11]. The most common site for Dieulafoy’s lesion is the lesser curvature of the stomach (70%) due to the vessels running directly from the arterial chain within the curvature. About 75-90% of these lesions are seen within 6-10 cm from the gastro-oesophageal junction [3]. However, 30% of Dieulafoy’s lesions are extragastric, mostly located in the duodenum, as in presented case and next involving the colon. The other less frequent sites include- oesophagus, jejunum-ileum, rectum, anus and bronchus [3].
Typical clinical presentation of Dieulafoy’s lesion will be in the form of acute GIB. The mode of presentation may be of various forms such as haematemesis, melena, haematemesis and melena, haemotochezia and iron-defeciency anaemia [8]. In the presented case, passing of blackish coloured stools (melena) without any other symptoms was the early presentation of acute GIB. Approximately 50-70% of cases in the literature [12] show that melena was the main mode of presentation of Dieulafoy’s lesion, as seen in our case.
Patient was taken up for investigations, considering UGIB to be the cause for melena. Most of the blood investigations showed the patient to be in haemodynamically unstable state. UGI endoscopy was done as an emergency procedure and it revealed abnormal vessels at D1/D2 of C loop duodenum with normal mucosa consistent with Dieulafoy’s lesion along with active bleeding. Literatures show that 75% of lesions can be diagnosed by GI endoscopy as in our case [13]. Diagnostic criteria for Dieulafoy’s lesion on endoscopy include - three categories: (i) active or minimal bleeding through normal mucosa or defect < 3 mm; (ii) appreciation of abnormal vessel with or without bleeding within normal mucosa or mucosal defect; (iii) appearance of fresh adherent clot within mucosal defect or normal mucosa associated with either of the symptoms as described earlier [7,14]. Our patient met these criteria. The other methods that can be used in successfully localising Dieulafoy’s lesion include endoscopic ultrasound, capsule endoscopy and push enteroscopy in small intestine lesions [7,15]. When endoscopic methods fail to identify the location of bleeding Dieulafoy’s lesion, the other techniques include selective angiography, CT-angiography and Technetium-99m labeled red blood cell scan [4,16]. However the treatment method may have its own limitations.
Resuscitative methods were undertaken to stabilise the patient using packed cells. As the bleeding site of the Dieulafoy’s lesion was identified by gastroscopy, haemoclips were applied and haemostasis secured similar to shown in the earlier studies [8,13]. No randomised studies so far have compared the treatment options for Dieulafoy’s lesion due to the relative scarcity of its incidence. The treatment options depend on the site of the lesion, mode of presentation and the available facilities. Several studies showed the treatment options like endoscopic methods, endoscopic ultrasound guided or angiography with embolisation [4,13]. Of these, endoscopic haemostatic procedures are the treatment of choice in most of these lesions with a success rate of over 90%. The procedures may be in the form of thermal electrocoagulation (heat probe or argon plasma), injection sclerotherapy or banding and haemoclip [13]. We opted for endoscopic haemoclip in our case.
Due to the advances and evolution of endoscopic haemostatic methods the role of surgery in Dieulafoy’s lesion has drastically reduced. Surgical procedures are currently reserved for cases that are refractive to either endoscopic or angiographic methods or likelihood of re-bleeding. It may be in the form of under-running of the vessel or surgical resection of the lesion [7]. Few studies have shown that laparoscopic surgery is a good option in treating Dieulafoy’s lesion provided, on precise pre-localization of the bleeding site, as it is minimally invasive to the patient [17,18]. The most common complication of Dieulafoy’s lesion reported in the literatures includes re-bleeding [11,17]. Recent advances in endoscopic procedures have improved the detection rate and in treating re-bleeding Dieulafoy’s lesion as well, which has significantly improved the prognosis of the patient [17,19,20]. In the presented case, patient had no re-bleeding and was discharged well. Apart from treating the Dieulafoy’s lesion, appropriate care was given for diabetes as well.
Conclusion
Duodenal Dieulafoy’s lesion, even though rare, is a challenge to diagnose. It is one of the obscure causes of GIB affecting elderly group and usually associated with comorbidity. Melena is the most common mode of its clinical presentation and UGI endoscopy is the best diagnostic tool. Even though many treatment options are available, the endoscopic haemoclipping method remains the preferred treatment for Dieulafoy’s lesions. The role of surgery is limited in these types of lesions.
[1]. Longstreth GF, Epidemiology of Hospitalization for Acute Upper Gastrointestinal Haemorrhage: A Population-Based StudyAm J Gastroenterol 1995 90(2):206-10. [Google Scholar]
[2]. Al-Mishlab T, Amin AM, Ellul JP, Dieulafoy’s lesion: an obscure cause of GI bleedingJ R Coll Surg Edinb 1999 44:222-25. [Google Scholar]
[3]. Stojakov D, Velckovic D, Sabljak P, Bjelovic M, Ebrahimi K, Spica B, Dieulafoy’s lesion: rare cause of massive upper gastrointestinal bleedingActa Chir Lugosi 2007 54(1):125-29. [Google Scholar]
[4]. Zippi M, Traversa G, Bruni A, Pica R, Occhigrossi G, Scevola G, Gastric Dieulafoy’s lesion successfully treated by “adjuvant” arterial embolization and endoscopic clippingClin Ter 2013 164(6):511-13. [Google Scholar]
[5]. Marangoni G, Cresswell AB, Faraj W, Shaikh H, Bowles MJ, An uncommon cause of life-threatening gastrointestinal bleeding: 2 synchronous Dieulafoy lesionsJ Paediatr Surg 2009 44:441-43. [Google Scholar]
[6]. Scmulewitz N, Baillie J, Dieulafoy lesions; a review of 6 years experience of a tertiary referral centreAm J Gastrenterol 2001 96:1689-94. [Google Scholar]
[7]. Lee YT, Walmsley RS, Leong RW, Sung JJ, Dieulafoy’s lesionGastrointest Endosc 2003 58:236-43. [Google Scholar]
[8]. Chaer R, Helton WS, Dieulafoy’s diseaseAm Coll Surg 2003 196:290-96. [Google Scholar]
[9]. Kanth R, Mali P, Roy PK, Outcomes in dieulafoy’s lesion: a 10-year clinical reviewDig Dis Sci 2015 60(7):2097-103. [Google Scholar]
[10]. Alshumrani G, Almuaikeel M, Angiographic findings and endovascular embolization in Dieulafoy disease: a case report and literature reviewDiagn Intervent Radiol 2006 12:151-54. [Google Scholar]
[11]. Pathan NF, El-Fanek H, A 70-year-old man with episodes of upper gastrointestinal bleedingArch Pathol Lab Med 2006 130:27-29. [Google Scholar]
[12]. Iacopini F, Petruzziello L, Marchese M, Larghi A, Spada C, Familiari P, Haemostasis of Dieulafoy’s lesion by argon plasma coagulationGastrointest Endosc 2007 6:20-26. [Google Scholar]
[13]. Nojkov B, Cappell MS, Gastrointestinal bleeding from Dieulafoy’s lesion: Clinical presentation, endoscopic findings and endoscopic therapyWorld J Gastrointest Endosc 2015 7(4):295-307. [Google Scholar]
[14]. Hyun C, Periampullary Dieulafoy’s lesionHosp Phys 2005 :23-27. [Google Scholar]
[15]. Prasad TR, Lim KW, Lim KT, Yap TL, Bleeding jejunal Dieulafoy pseudopolyp: capsule endoscopic detection and laparascopic-assisted resectionJ Laparoendosc Adv Surg Tech 2007 17:509-12. [Google Scholar]
[16]. Lee KS, Moon JM, Lee SI, Park IS, Sohn SK, Yu JS, A case of bleeding from the Dieulafoy lesion of the jejunumYonsei Med J 1997 38:240-44. [Google Scholar]
[17]. Baxter M, Aly EH, Dieulafoy’s lesion: current trends in diagnosis and managementAnn RCS Eng 2010 92(7):548-54. [Google Scholar]
[18]. Eisenberg D, Bell R, Intraoperative endoscopy: a requisite tool for laparoscopic resection of unusual gastrointestinal lesions - A case seriesJ Surg Res 2009 155:318-20. [Google Scholar]
[19]. Jeon HK, Kim GH, Endoscopic Management of Dieulafoy’s LesionClin Endosc 2015 48(2):112-20. [Google Scholar]
[20]. Khan R, Mahmad A, Gobrial M, Onwochei F, Shah K, The diagnostic dilemma of dieulafoy’s lesionGastroenterology Res 2015 8(3-4):201-06. [Google Scholar]