Polysplenia syndrome is characterised by spectrum of abnormalities which are rarely diagnosed in adults as an incidental finding. The anomalies include multiple spleens, midline liver, gall bladder and biliary tract anomalies, short pancreas, agenesis of pancreas, right-sided stomach, intestinal malrotation, inferior vena cava interruption with azygous or hemiazygous continuation, and a Pre-Duodenal Portal Vein (PDPV). These anomalies may occur isolated or in combination. Since most of the minor anomalies do not cause clinical symptoms, polysplenia syndrome is mostly detected incidentally in the adults because of multi-detector computed tomography which is being used in diagnosis of associated disease process. Therefore, radiologists should become familiar with these rare and peculiar anomalies associated with polysplenia syndrome. In the present report, we describe the case of a 50-year-old male patient with heterotaxy syndrome with polysplenia incidentally diagnosed during an imaging evaluation of an unrelated pathological condition – Cholelithiasis.
Case Report
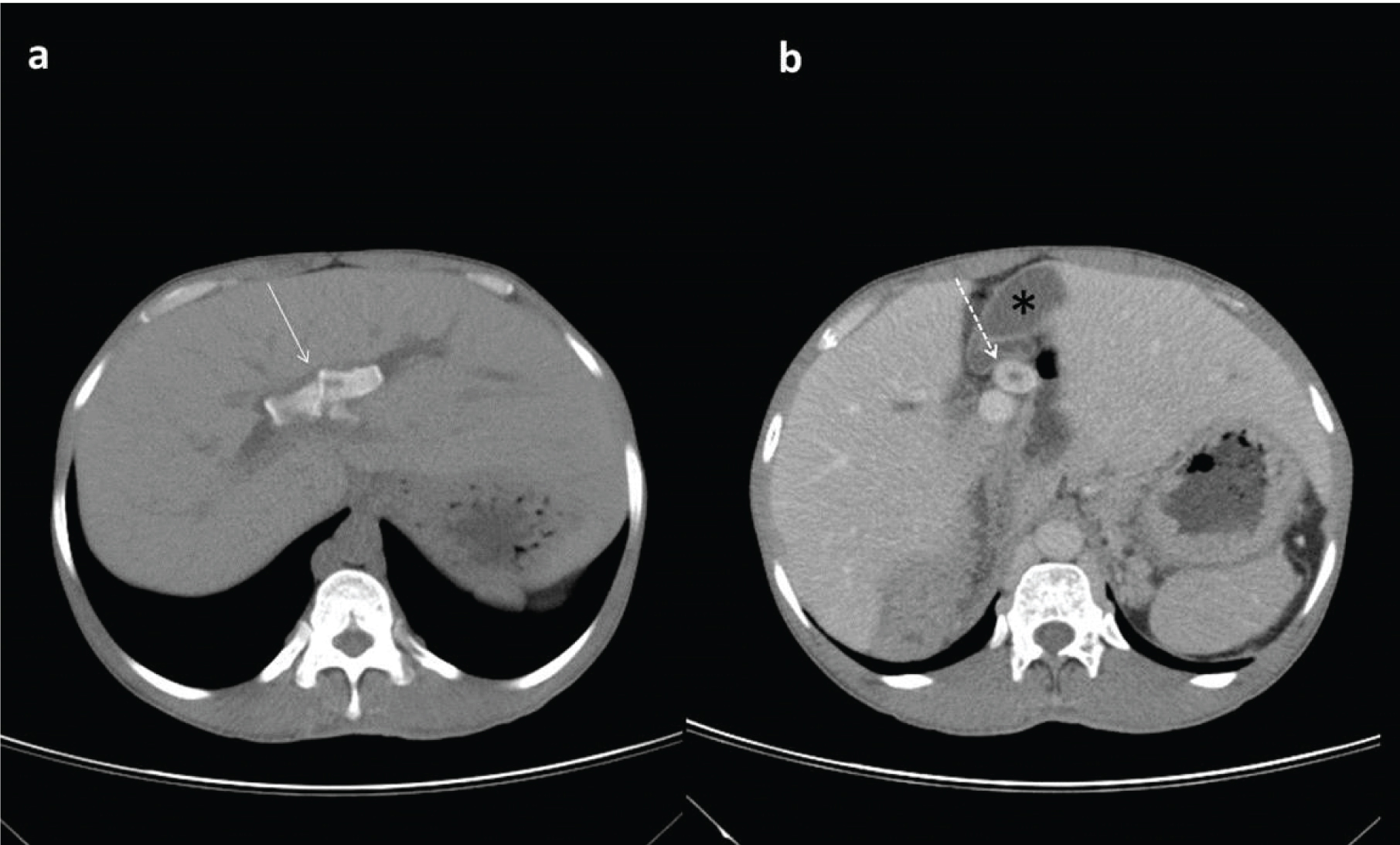
A 50-year-old male who was a case of uncontrolled diabetes mellitus presented to our outpatient department with chief complaints of easy fatiguability since 2-3 months, polyuria, and loss of weight and right upper quadrant pain. On examination his vitals were stable and clinical examination revealed no significant findings. Laboratory investigations revealed high fasting blood sugar levels. As a part of routine investigation ultrasonography of abdomen was done, which showed cholelithiasis and hepatolithiasis causing biliary obstruction. Contrast-enhanced MDCT of abdomen was done which showed few calculi at the confluence of common hepatic duct extending into both left and right hepatic ducts causing moderate central and mild peripheral intra-hepatic biliary duct dilatation as well as a large calculus in cystic duct. Gall bladder was located in the midline without wall thickening/pericholecystic fluid [Table/Fig-1a,b].
a) Axial non contrast CT image showing hepatolithiasis (solid white arrow); b) Axial CECT image showing calculus in cystic duct (dashed white arrow) with midline gall bladder (black asterisk).
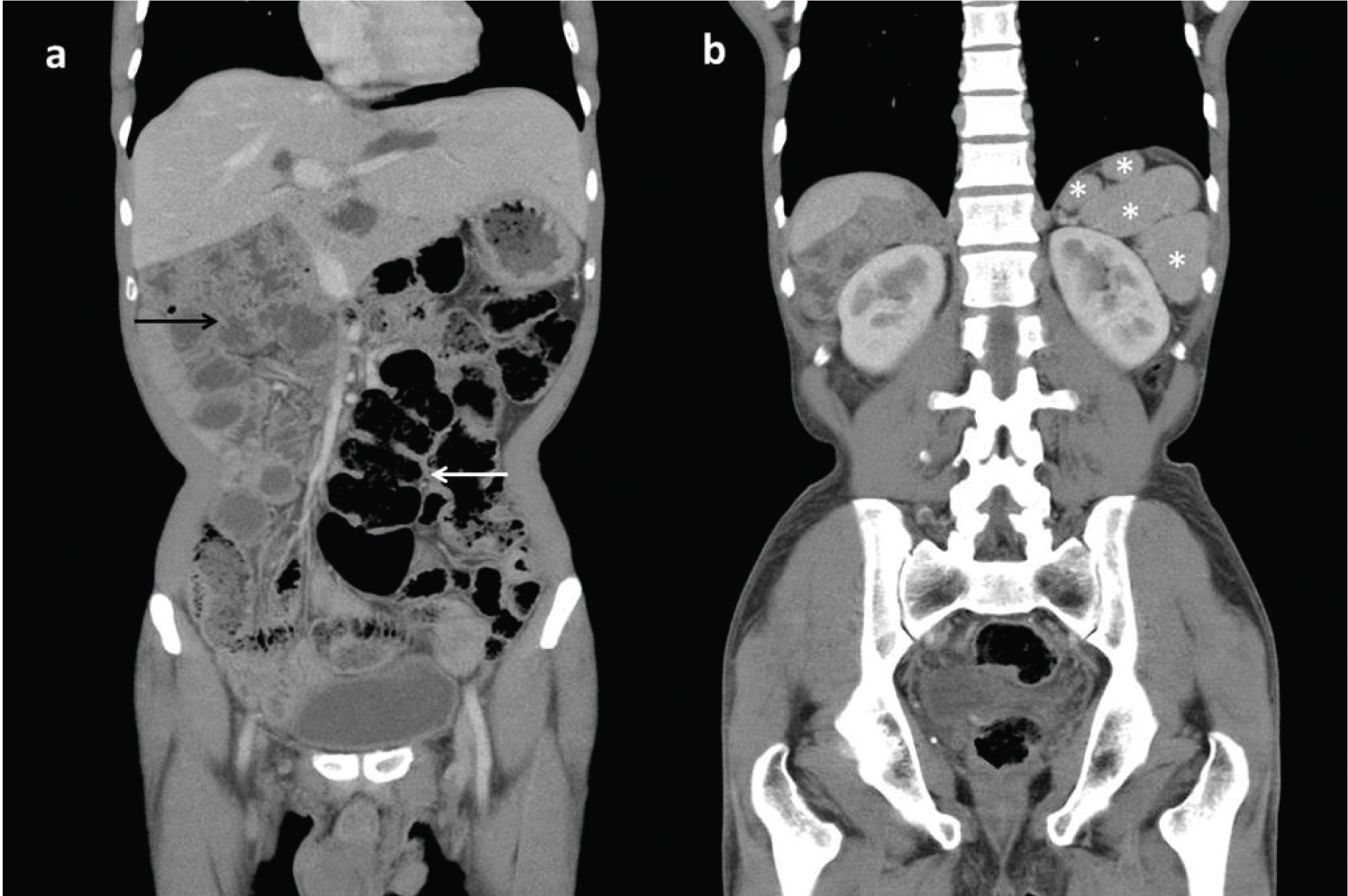
Duodenal loop was not seen to cross the midline, while jejunal and ileal loops were seen in the right lumbar region and right hypochondrium [Table/Fig-2a]. Duodenojejunal junction was located to the right of midline without any reversal of dudodenal loop. Liver was also located in the midline with multiple splenules in the left hypochondrium (polysplenia) [Table/Fig-2a,b]. Caecum and ascending colon were noted in midline while rest of the colonic loops was seen to the left of midline-suggestive of non-rotation of bowel [Table/Fig-2a]. Superior mesenteric vein was normal in location to right and ventral to superior mesenteric artery suggesting absence of intestinal malrotation.
Coronal CECT image shows midline liver with presence of large bowel loops on left side (thin white arrow) and small bowel on right side (thin black arrow) suggestive of intestinal non rotation; b) coronal CECT shows multiple discrete splenic tissues (white asterisks) in left sub-phrenic space consistent with polysplenia.
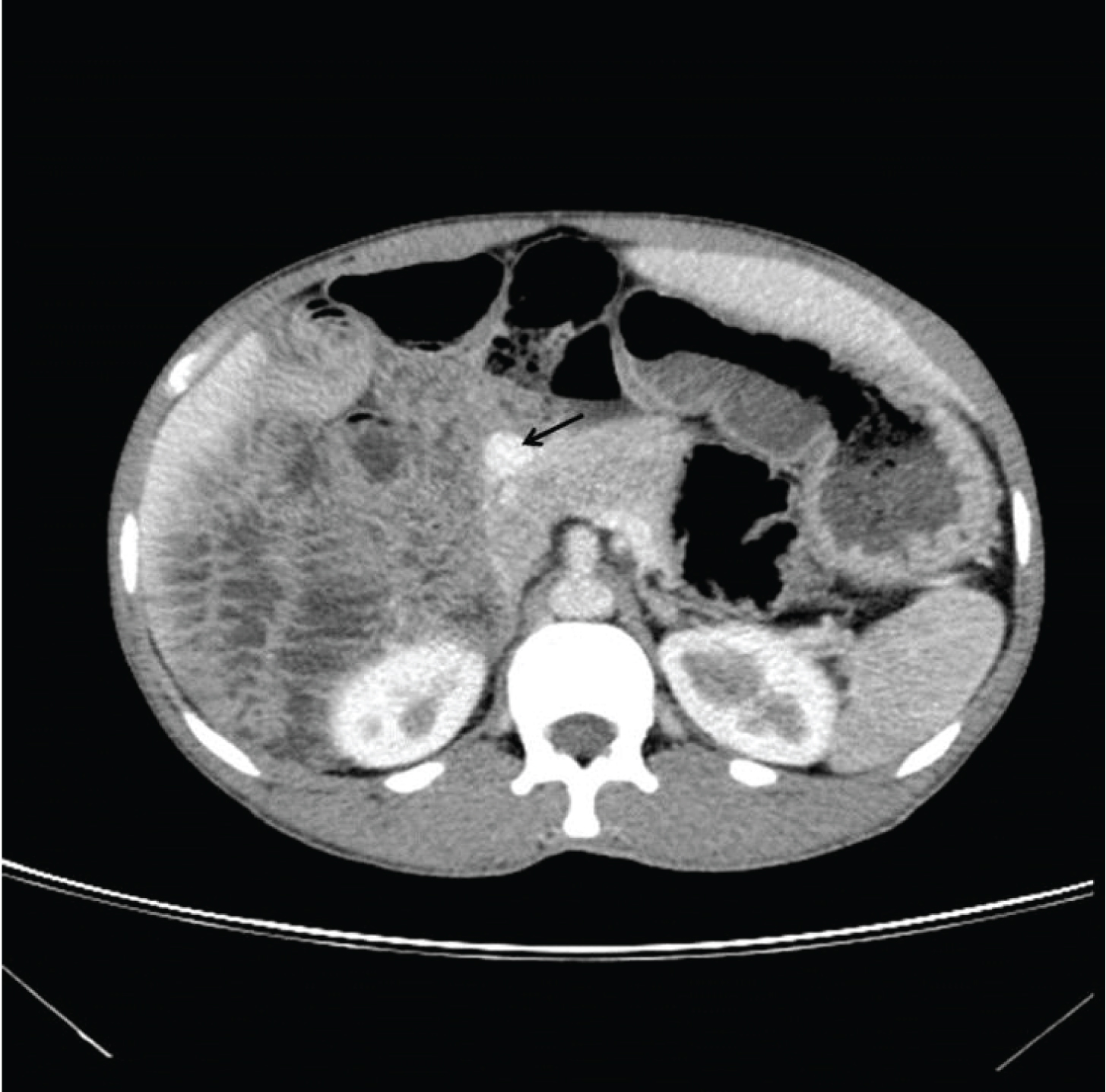
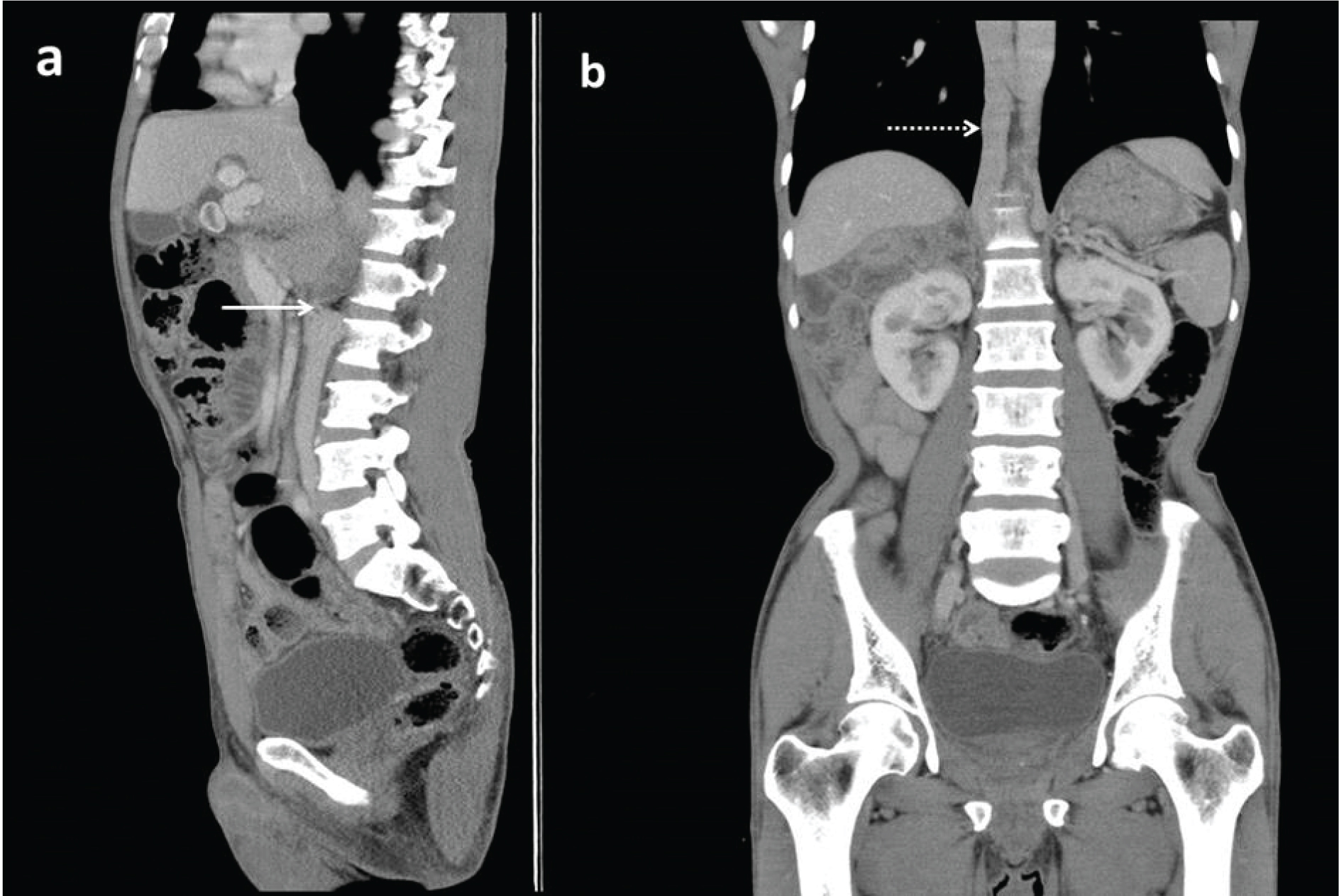
Portal vein was located anterior to the head of pancreas and duodenum–suggesting a pre-pancreatic and pre-duodenal course [Table/Fig-3]. Pancreas was normal in size and location without any anomalies. Supra-renal segment of Inferior Vena Cava (IVC) was not visualized but a dilated azygous vein, suggestive of interrupted IVC with azygous continuation was observed [Table/Fig-4a,b].
Axial CECT image showing pre-duodenal portal vein (black arrow) which is anterior to the head of pancreas.
a) Sagittal CT image showing interruption of IVC above the level of renal vein (solid white arrow); b) shows the azygous continuation of the interrupted IVC (dashed white arrow).
CT findings were consistent with heterotaxy syndrome with left isomerism (polysplenia syndrome) and a possibility of the PDPV causing compression of Common Bile Duct (CBD) leading to hepatolithiasis and cholelithiasis was given.
Based on above findings patient was planned for elective cholecystectomy and removal of intrahepatic calculi. However surgery was deferred due to uncontrolled diabetes. Patient failed to turn up for surgery on follow-up.
Discussion
Situs solitus refers to the usual position of the heart and abdominal viscera, with the cardiac apex, spleen, stomach and aorta located to the left and liver and Inferior Vena Cava (IVC) placed to the right. The mirror image position of these abdominal organs relative to situs solitus is known as situs inversus. A spectrum of abnormalities associated with atypical arrangement of organs and vessels is known as heterotaxy or situs ambiguous which has two subcategories which include polysplenia and asplenia [1].
Polysplenia is a rare heterotaxy disorder with a reported incidence of 1 per 250000 live births [2]. Reports indicate that polysplenia syndrome occurs in both genders with an identical frequency [3].
Interestingly, Asians show a higher prevalence of heterotaxy syndrome (32%) compared to western population. Various studies have concluded that there is no single etiological factor responsible for heterotaxy [4].
Polysplenia syndromes are being detected incidentally by Multi-Detector Computed Tomography (MDCT) or magnetic resonance imaging for the evaluation of other medical diseases in the adults [5].
The spectrum of abnormalities in polysplenia include multiple spleens, visceral heterotaxy, right sided stomach, left sided or midline liver, intestinal malrotation, a short pancreas and IVC anomalies [2]. These anomalies are strongly associated with congenital heart disease, immune deficiency and intestinal obstruction hence described in pediatric population [6].
Around 40% of the patients reach 2 years of age and 75% of patients die before 5 years of the age due to cardiac anomalies. A 5-10% of the patients lack cardiac anomalies, which allows them to reach adulthood [7,8].
The spleen develops from the dorsal mesogastrium as several clusters and then bulges on the left side to become the initial splenic primordium during the fifth week of embryogenesis. Therefore, it is regarded that failure of fusion of these clusters can lead to multiple spleens. The spleen and stomach develop together within the dorsal mesogastrium hence are located adjacent to each other [5].
Symptomatic polysplenia in adults is often caused by abnormal biliary and pancreatic duct drainage, cholecystitis and bowel obstruction [9]. Very few case reports of right sided stomach and left sided spleen are reported [10].
In our patient there were multiple small spleens along the greater curvature of the stomach.
Pancreatic anomalies may be related with polysplenia comprising of truncated pancreas which is a result of congenital agenesis of dorsal pancreas, partial agenesis of pancreas, annular pancreas, pancreas divisum and pancreatic malrotation [10]. However, in the present case pancreas was normal in size and location with normal head, body and tail.
Preduodenal-prepancreatic portal vein is a rare anomaly when the portal vein courses anterior to pancreas and duodenum. This disorder was first defined by Knight in the year 1921 [3].
Venous blood is drained from the primitive gut, by two vitelline veins of the yolk sac which are connected by one cranial (liver), one middle (behind the duodenum) and one caudal anastomosis (infront of duodenum).
The usual S shaped portal vein develops from two vitelline veins by loss of caudal and cranial communication between vitelline veins. Loss of vitelline veins in cranial and middle communication during early stage of embryonic development leads to PDPV [2].
The dorsal pancreatic bud lies cephalad and ventral to the middle anastomosis. The pancreatic buds switch in a clockwise manner and fuse together subsequently placing portal vein in the typical position posterior to the duodenum and the pancreas [11].
A PDPV may be asymptomatic and can be incidentally diagnosed during work up for other diseases. Some disorders might be connected with PDPV like duodenal atresia, stenosis, web, annular pancreas and malrotation which may require surgical management [3].
PDPV in adults can compress the common bile duct and rarely cause cholelithiasis which is the indication for surgery. Preoperative evaluation with CT can detect PDPV prior to surgery which is necessary to prevent damage to portal vein due to its anterior location causing disastrous consequences like haemorrhage and vascular ligation [3].
Another rare entity described is prepancreatic post-duodenal portal vein which occurs when the dorsal pancreatic bud lies caudal and dorsal to the middle anastomosis and the caudal segment of the left vitelline vein. Rotation of the pancreatic buds in a clockwise manner results in a portal vein posterior to the duodenum and anterior to the pancreas. This variance can cause biliary symptoms requiring surgery [11].
Malrotation or non-rotation of the gastrointestinal tract is commonly observed in polysplenia syndrome [5]. Intestinal malrotation diagnosed by superior mesenteric vein rotation on CT is seen in 60% of cases of polysplenia [12].
Intestinal non-rotation as described in the present case is generally asymptomatic. In a case series, intestinal rotation anomalies were observed in seven of eight patients with polysplenia with no history of obstruction [1].
Azygous continuation of IVC is an unusual asymptomatic vascular anomaly most commonly lined with heterotaxy (80%) with an occurrence of 0.10%. In this disorder there is agenesis of hepatic segment of IVC with continuation through the azygous system by persistent right supracardinal vein draining into superior vena cava [7,13].
Management of adult cases of polysplenia is chiefly symptomatic and surgical treatments is mainly due to biliary obstruction, intestinal obstruction or presence of other morbidities [7,10].
Conclusion
Heterotaxy syndrome in adults is a rare congenital disorder. The radiological recognition of its varied presentations, as well as their appropriate description, would prevent serious complications during abdominal surgery caused due to anatomical alterations.
Situs abnormality may not always cause symptoms or medical problems in adults. This case shows that situs ambiguous can present in adults as an incidental finding. These anomalies can result in confusion during invasive procedures and is necessary to perform careful analysis of these anomalies prior to any surgical or medical intervention. Through the use of radiology, these anomalies are being detected more frequently which is of utmost importance in patient management.
[1]. Fulcher AS, Turner MA, Abdominal manifestations of situs anomalies in adults 1Radiographics 2002 22(6):1439-56. [Google Scholar]
[2]. Low JP, Williams D, Chaganti JR, Polysplenia syndrome with agenesis of the dorsal pancreas and preduodenal portal vein presenting with obstructive jaundice—a case report and literature reviewThe British Journal of Radiology 2011 84(1007):e219-22. [Google Scholar]
[3]. Seo HI, Jeon TY, Sim MS, Kim S, Polysplenia syndrome with preduodenal portal vein detected in adultsWorld J Gastroenterol 2008 14(41):6418-20. [Google Scholar]
[4]. Kim SJ, Heterotaxy syndromeKorean Circulation Journal 2011 41(5):227-32. [Google Scholar]
[5]. Kim S, Lee YS, Jung JH, Anomalies of abdominal organs in polysplenia syndrome: multidetector computed tomography findingsJournal of the Korean Society of Radiology 2016 74(2):114-22. [Google Scholar]
[6]. Barbara RR, Rahaman RA, Case report of situs ambiguous with polysplenia and left-sided isomerismOpen J Clin Med Case Rep 2017 3(1):1-4. [Google Scholar]
[7]. Plata-Munoz JJ, Hernandez-Ramirez D, Anthon FJ, Podgaetz E, Avila-Flores F, Chan C, Polysplenia syndrome in the adult patient. Case report with review of literatureAnn Hepatol 2004 3(3):114-17. [Google Scholar]
[8]. Anand U, Chaudhary B, Priyadarshi R, Kumar B, Polysplenia syndrome with preduodenal portal veinAnn Gastroenterol 2013 26(2):182 [Google Scholar]
[9]. Kapa S, Gleeson FC, Vege SS, Dorsal pancreas agenesis and polysplenia/heterotaxy syndrome: a novel association with aortic coarctation and a review of the literatureJOP: Journal of the Pancreas 2007 8(4):433-37. [Google Scholar]
[10]. Rameshbabu CS, Gupta KK, Qasim M, Gupta OP, Heterotaxy polyplenia syndrome in an adult with unique vascular anomalies: case report with review of literatureJ Radiol Case Rep 2015 9(7):22-37. [Google Scholar]
[11]. Goussous N, Cunningham SC, Prepancreatic postduodenal portal vein: a case report and review of the literatureJ Med Case Reports 2017 11:2 [Google Scholar]
[12]. Nichols DM, Li DK, Superior mesenteric vein rotation. A CT sign of midgutmal rotationAJR 1983 141(4):707-08. [Google Scholar]
[13]. Gonçalves CM, Noschang J, Silva AC, Mello RJ, Schuh SJ, Maciel AC, Heterotaxy syndrome: a case reportRadiologia Brasileira 2014 47(1):54-56. [Google Scholar]