Aseptic Inflammation and Synovitis of Knee by Splinter Injury in an Adult- A Rare Presentation
Pankaj Kumar Mishra1, Anil Kumar Pandey2, Aashish Anand Gupta3, Tanmay Shah4
1 Assistant Professor, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
2 Resident, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
3 Resident, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
4 Resident, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pankaj Kumar Mishra, House No. E-115/4 Shivaji Nagar, Bhopal-462016, Madhya Pradesh, India.
E-mail: drpankajv@yahoo.com
Synovitis of knee due to an unaware incident of splinter piercing is rare in adults. This is a case report of 30-year-old female with a painful knee in a flexed attitude with a swelling. Her history did not reveal any positive findings, i.e., recent trauma, fever or any such previous episode. Arthrotomy revealed a turbid synovial fluid with inflamed friable synovial thickening. On further inspection, there was a presence of a foreign body in the suprapateller pouch. It was removed and washed. This was ultimately found to be a splinter. Normal inflammatory markers with minimal signs and symptoms of infection may provide weightage to this differential diagnosis. Arthrotomy and antibiotic coverage can give an excellent result.
Arthrotomy, Foreign body, Inflammation
Case Report
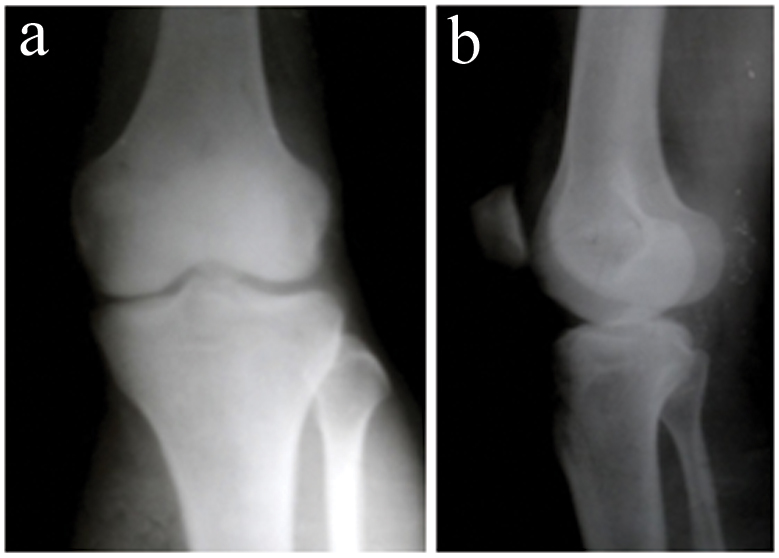
A 30-year-old female presented to the Outpatient Department (OPD) with a painful swelling of the left knee for 20 days. On inspection, the knee was in flexed attitude and was swollen. Due to pain, she was unable to flex and extend her knee actively. On palpation, it was synovitis (typical boggy feeling felt over suprapateller pouch) with slight effusion (negative patellar tap) and local rise of temperature. Under aseptic conditions, the joint was aspirated and was found to be slightly turbid. About 3 mL of synovial fluid was sent for culture, gram staining and synovial fluid examination, which showed hardly any demonstrable organisms, few epithelial cells, and 3+ pus cells. The routine blood examination was near normal, CRP level of <5 mg/L and ESR was 28. The patient was apyrexic but very anxious. Her history did not reveal any positive finding i.e., recent trauma, fever, similar type of previous episode. X-ray revealed normal bony findings [Table/Fig-1]. The MRI showed synovial thickening. Hence, the clinico-radiological differential diagnosis of sub-acute synovitis, pigmented villonodular synovitis, low grade septic arthritis and crystal disorder were considered.
Showing the normal anterioposterior and lateral X-ray of left knee.
The patient was admitted, her limb was rested. Ceftriaxone with amikacin were commenced. Hydration was improved using intravenous fluids. The arthrotomy was performed in an emergency Operation Theatre (OT) which revealed turbid synovial fluid with inflamed friable synovial thickening. On careful inspection, there was a foreign body found in the suprapateller pouch. It was removed and washed and was ultimately found to be a splinter measuring about 4 mm (width) x 3mm (height) x 35 mm (length) [Table/Fig-2].
Image showing the splinter found within the suprapatellar pouch.

The joint was generously washed after sub-total synovectomy and closed under drain. Swab obtained after arthrotomy did not show any bacterial growth. Postoperative recuperation was uneventful and she was discharged after three days on oral medication. After six months on follow up, the patient had recovered well.
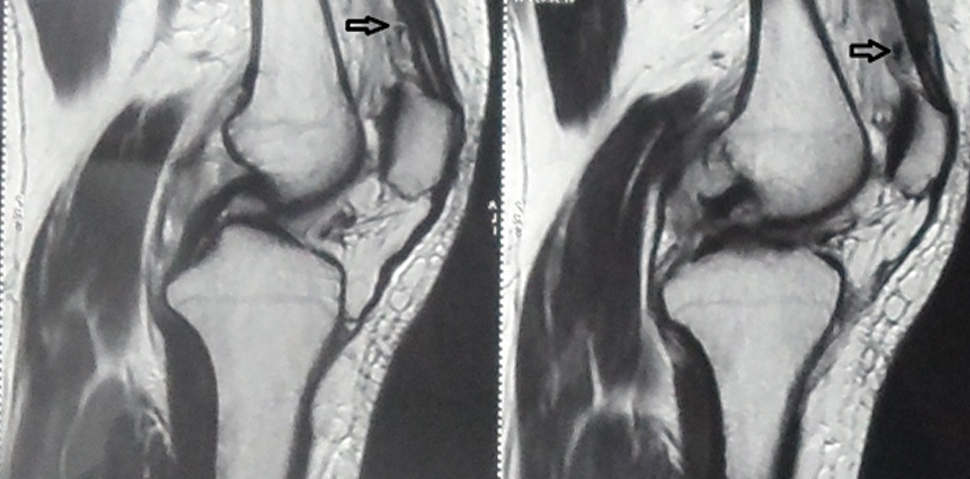
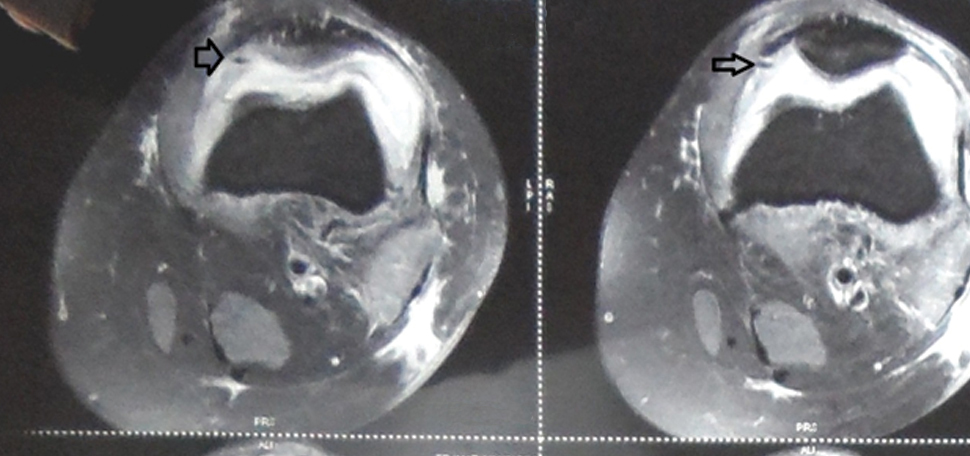
Upon the initial enquiry, the patient did not reveal history of any known injury. However, after removal of the foreign body, she recalled that a few months to an year back, she had sustained the injury around her left knee in the jungle but could not rembember any object piercing her at that time. In time, due to chronic inflammation, synovitis ensued. Hence, the foreign body was missed preoperatively. When the MRI film again re-reviewed postoperatively, it revealed the foreign material embedded in the medial retinaculum, corresponding to suprapatellar pouch [Table/Fig-3,4].
Saggital sections showing synovial debris and thickening. After the surgery and retrieval of foreign body in the joint the same MRI film was re-inspected and the foreign body was found in suprapatellar area (marked by arrow). (The foreign body was missed preoperatively).
Successive axial section of MRI film depicting foreign body (marked by arrow) engaged in medial retinaculum of the left knee, (which was missed preoperatively).
Discussion
Unnoticed splinter (part of wood) injury to the knee is a rare presentation. Sometimes, patients give a history of removing a pricked thorn or splinter around the knee. However, it is not uncommon for it to go unnoticed. In such circumstances, the piercing foreign body goes inside the joint and causes foreign body reaction, synovitis and septic arthritis. Synovitis due to foreign body may simulate septic arthritis [1]. For such a differential diagnosis the suspicion is paramount due to difficulty in appreciating the entry portal the foreign body.
A splinter is an organic type of foreign body and inflammatory reaction is caused by its inherent alkaloid, oils, and resins constituents, which are harmful for humans [2]. In earlier days, it was conceded that foreign body is a noninfective material. However, the synovial fluid and blood cultures have demonstrated Pantoea agglomerans, Staphylococcus albus as common pathogenic organism [3]. On the contrary, this case report has not showed any organism, so it could be labeled as aseptic synovitis due to splinter.
Joint lavage and hypertrophic synovium removal with antimicrobial coverage is mainstay of treatment. This can be performed by open as well as by an arthroscopic surgery. In comparison to arthrotomy, the arthoscopic surgery has better visualisation as well as lower morbidity. Overwhelming literature favours arthoscopy over the open procedure. The longer operating interval, its technicality and a small risk to articular cartilage damage are the concerns with arthroscopy [4].
Furthermore, the cons of arthroscopy in such a situation is to miss the foreign material due to an extra articular placement of foreign body and poor visibility created by plica reaction leaving the foreign body in situ. Thus, double inspection of joint during surgery is recommended in such cases [5,6]. However, ultimately it is the sovereign of surgeon to choose either of the modality, as per their preference and familiarity.
Conclusion
Careful history and attention should be paid to chronic synovitis of knee even with the insignificant history of trauma around knee. The penetrating injury with plant material (splinter) may occur with minor trauma and could go unnoticed. Usually, such type of injury is common in children, because either it remains unnoticed by them or they fear informing their parents. Such a presentation in adults is uncommon. Normal inflammatory markers and minimal signs and symptoms of infection may provide weightage to this differential diagnosis, whereas typical true infection has a short course of onset and toxemic clinical features with increased level of inflammatory marker. Simple arthrotomy or arthoscopic washing with antibiotic coverage can give an excellent result.
[1]. Sivakumar R, Singhi PK, Chidambaram M, Somashekar V, Thangamani V, A sub-acute septic arthritis of the knee; a sequelae to thorn prick injury of patella: a case reportJ Orthop Case Rep 2016 6(5):100-03. [Google Scholar]
[2]. Karshner AG, Hanafee W, Palm thorns as a cause of joint effusion in childrenRadiology 1953 60(4):592-95. [Google Scholar]
[3]. Kratz A, Greenberg D, Barki Y, Cohen E, Lifshitz M, Pantoea agglomerans as a cause of septic arthritis after palm tree thorn injury; case report and literature reviewArch Dis Child 2003 88(6):542-44. [Google Scholar]
[4]. Birr R, Wuschech H, Kundiger R, Heller G, Complications in 4,000 arthroscopiesBeitr Orthop Traumatol 1990 37(11-12):620-26. [Google Scholar]
[5]. Taskiran E, Toros T, Chronic synovitis caused by a date palm thorn: an unusual clinical pictureArthroscopy 2002 18(2):E7 [Google Scholar]
[6]. Pai VS, Tan E, Matheson JA, Box thorn embedded in the cartilaginous distal femurInj Extra 2004 35(5-6):45-47. [Google Scholar]