Hernia repairs account for over 20 million operations performed annually and is considered one of the most frequently undertaken surgical procedures across the world today [1].
Hernias of the anterior abdominal wall or ventral hernias are abnormal protrusions of viscera or preperitoneal contents, through congenital or acquired defects in the fascia or musculature of the parietal abdominal wall [2]. They occur in 0.5-1% of the population [3]. Midline ventral hernias constitute approximately 20% of all abdominal wall hernias; they may be primary or secondary [4]. The former include umbilical, paraumbilical and epigastric hernias [2].
Generally, ventral hernias arise secondary to increased intra-abdominal pressure in the setting of obesity, multiparity or ascites [5]. In addition, defective primary wound healing, surgical site infection, malnutrition, multiple procedures and technical errors contribute in the development of incisional hernias [2,6].
Most, if not all, ventral hernias require surgery as they tend to enlarge over time and may develop complications such as incarceration, obstruction or strangulation resulting in considerable morbidity and mortality [5,7].
Experience with primary tissue repair revealed a lower incidence of wound-related complications, however, recurrence rates (ranging from 15-40%), were unacceptably high [8]. Introduction of prosthetic repairs have substantially reduced recurrence rates when compared to primary tissue approximation and are indicated in all but the smallest of ventral hernias [9,10]. However, higher rates of wound-related complications and chronic pain have been observed in this group [8,11]. Laparoscopic ventral hernia repair combines the advantages of these two techniques.
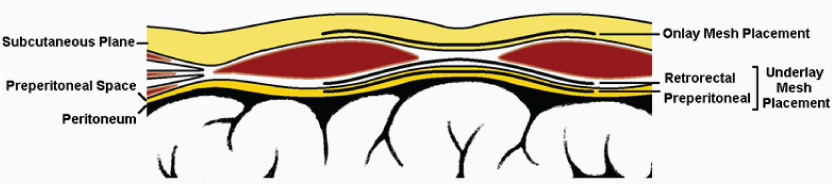
Today, a number of options exist with regard to operative approach, type of prosthesis and anatomical plane of placement. Position of the mesh influences the tissue reaction and subsequent ingrowth affecting tensile strength in the long-term [12-14]. Implantation of the mesh on the anterior rectus sheath over the defect is termed onlay repair whereas, inlay repair bridges the defect using a mesh sutured to the aponeurotic edges of the rectus sheath. Underlay repairs involve positioning the mesh below the defect, either deep to the rectus abdominis (retrorectal), in the preperitoneal space (preperitoneal) or in the peritoneal cavity (intraperitoneal) [3,15].
Presently, data regarding the superiority of one technique over the other is conflicting and inconclusive. There is no universal consensus regarding indications for surgery, optimal approach, most appropriate method of repair, need for a prosthesis, ideal material and location of placement.
This study sought to identify the clinical patterns of presentation of ventral hernias in adults, compare the commonly performed open repairs with regard to operating time, pain, wound-related complications, duration of hospital stay and recurrence, and determine the factors influencing these outcomes.
Materials and Methods
This prospective, observational study was undertaken at Bangalore Medical College and Research Institute from January 2012 to January 2015. A total of 199 cases were eligible for inclusion into the study.
For subject selection, we utilized the ventral hernia staging system which stratifies ventral hernias into three stages, based on width of the defect and wound class [16]. Patients over the age of 18 years diagnosed with stage one midline ventral hernias (defect size <10cm and no contamination) and meriting prosthetic repair, were included. These hernias could either be primary or following first recurrence.
Small hernias meriting anatomical repair, large hernias with loss of abdominal domain requiring alternative methods of repair, complicated (obstructed or strangulated) hernias precluding mesh repair, and hernias recurring after mesh repair were excluded. Patients with signs of infection or who were seriously ill (ASA 4 and 5) and patients unwilling to give informed consent were also excluded.
Demographic data, presence of relevant comorbidities and treatment history were recorded. Body Mass Indices (BMI) were calculated and grouped according to the Revised Consensus Guidelines for India with obesity defined as a BMI ≥25kg/m2 [17]. Prior to surgery, patients underwent ultrasonogram to assess the number, size and location of defects and to rule out any concurrent abdominal pathology precluding the use of a mesh.
Antimicrobial prophylaxis was administered and surgery was performed under spinal or general anaesthesia. Epidural catheterisation was used when indicated for postoperative analgesia.
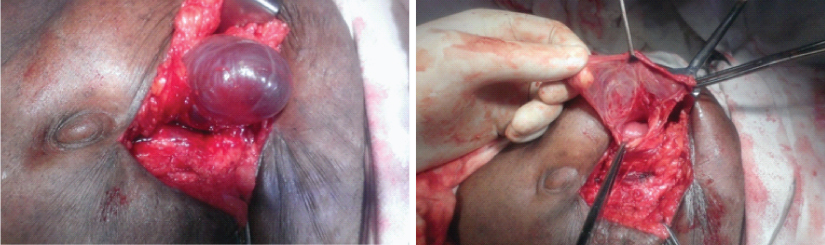
Procedures were performed by experienced general surgeons. Intraoperatively, hernia sac was identified, adhesions released, contents reduced and the peritoneum closed [Table/Fig-1]. The repair was completed by primarily approximating the defect without tension and reinforcing the same with an artificial prosthesis, placed either onlay, retrorectus or in the preperitoneal space, the latter two constituting underlay repairs [Table/Fig-2]. A lightweight macroporous polypropylene mesh permitting overlap of at least 4 cm from fascial margin in all directions was used. Care was taken to avoid contact with underlying viscera. Closed suction drains were placed when indicated and removed when the output was under 20 ml. Total time taken for surgery was documented.
Intraoperative picture showing hernial sac, a) in a case of incarcerated incisional hernia, which had formed a hydrocele of the sac; b) After the sac was opened.
Schematic diagram of the anterior abdominal wall and position of mesh placement in the respective repairs.
Pain was assessed on the fifth postoperative day using a visual analogue scale (VAS) ranging from 0 (no pain) to 10 (unbearable pain). Surgical Site Occurrences (SSO) in the early postoperative period was noted. Before discharge, all patients were counselled regarding follow up for a minimum period of two years.
Data was entered in Excel software and analysed using R software version 3.2.2. Continuous variables were presented as mean and Standard Deviation (SD) and categorical variables as count and per cent. To compare means of more than two groups, one-way ANOVA was used. Chi-square test was used to determine the association between categorical variables, and when expected cell count was less than five, Fisher’s-exact test was used. A p-value of <0.05 was considered statistically significant.
Results
A total of 199 cases were studied. Age of the patients ranged from 18–85 years with a mean age of 44.3 years (SD±12.90). Statistically significant difference (p< 0.001) was noted on comparing mean age at presentation of primary (41.7 years, SD±11.33) and secondary (49.4 years, SD±14.30) ventral hernias.
Overall, 22.1% (n=44) were male and 77.9% (n=155) were female. Primary and secondary hernias were equally distributed between both the genders.
Most patients were asymptomatic apart from the swelling (n=164, 82.4%). Only 17.6% complained of pain associated with swelling.
Mean BMI of the study population was 24.4kg/m2 (range 20.2–30.6kg/m2; SD±2.08kg/m2). Normal BMI (18.5–22.9kg/m2) was observed in 29.6%, 45.7% were overweight (23.0–24.9kg/m2) and 24.6% were obese (≥25kg/m2).
The average diameter of the hernial defects was 3.8cm (range 2.2–6.0cm; SD±0.76cm). Incisional hernias were noted to have significantly larger defects (4.6cm) when compared to primary ventral hernias (p<0.001).
The majority of ventral hernias were primary (n=132, 66.3%); incisional hernias constituted the remaining 33.7%. Gynaecological procedures (n=45; 22.6%) were the most common preliminary operation that these patients had undergone. Others included laparotomies (6.5%) and ventral hernia repairs (4.5%).
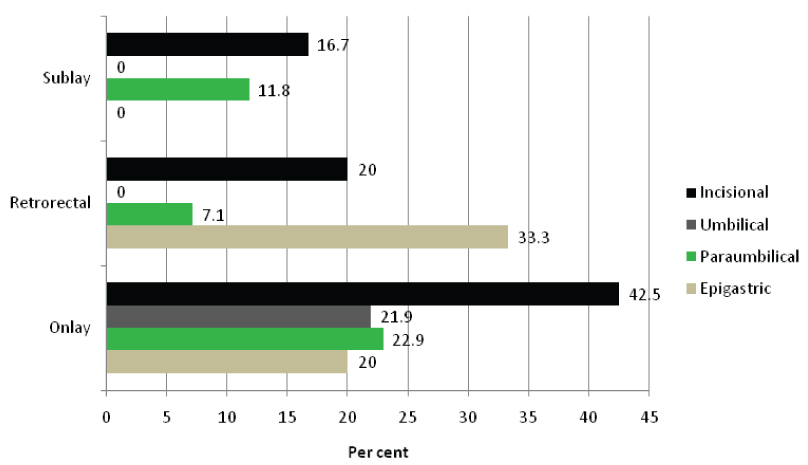
The different surgical modalities of repair performed with respect to hernia type are shown in [Table/Fig-3]. Overall, onlay repair was the most commonly performed procedure (56.3%). Retrorectal and preperitoneal repairs constituted 22.6% and 21.1% of repairs, respectively. There was no significant difference in age, sex, presence of comorbidities, BMI, hernia type or defect size between the repair groups.
Demographic features and types of hernia with respect to the different surgical modalities of repair performed.
| Type of Repair Performed | p-value |
|---|
| Onlay | Retrorectal | Preperitoneal |
|---|
| N | 112 | 45 | 42 |
|---|
| Age of the Patient (in years) | 45.2 (±13.12) | 45.2 (±13.48) | 41.0 (±11.35) | 0.176 |
| Age Distribution(in years) | <30 | 15 (13.4%) | 6 (13.3%) | 7 (16.7%) | 0.725 |
| 31-40 | 33 (29.5%) | 15 (33.3%) | 18 (42.9%) |
| 41-50 | 28 (25.0%) | 10 (22.2%) | 9 (21.4%) |
| 51-60 | 22 (19.6%) | 9 (20.0%) | 4 (9.5%) |
| >60 | 14 (12.5%) | 5 (11.1%) | 4 (9.5%) |
| Sex of the Patients | M | 28 (25.0%) | 8 (17.8%) | 8 (19.1%) | 0.532 |
| F | 84 (75.0%) | 37 (82.2%) | 34 (81.0%) |
| Body Mass Index (kg/m2) | 24.5 (±2.38) | 24.3 (±1.75) | 24.4 (±1.53) | 0.735 |
| Type of Hernia | Epigastric | 5 (4.7%) | 3 (6.7%) | 4 (9.5%) | 0.771 |
| Paraumbilical | 35 (31.3%) | 14 (31.1%) | 17 (40.5%) |
| Umbilical | 32 (28.6%) | 13 (28.9%) | 9 (21.4%) |
| Incisional | 40 (35.7%) | 15 (33.3%) | 12 (28.6%) |
| Size of the Defect (in cm) | 3.9 (±0.82) | 3.8 (±0.68) | 3.7 (±0.67) | 0.388 |
| Comorbidities | Diabetes | 13 (11.6%) | 3 (6.7%) | 0 | 0.057 |
| Hypothyroidism | 1 (0.9%) | 1 (2.2%) | 2 (4.8%) | 0.311 |
| COPD | 2 (1.8%) | 2 (4.4%) | 2 (4.8%) | 0.514 |
| Hypertension | 4 (3.6%) | 3 (6.7%) | 0 | 0.241 |
*Independent Student t-test for continuous variables and Chi-square test for categorical variables were used to test statistical significance. p < 0.05 was considered statistically significant.
Mean operative time, pain scores, incidence of SSO and duration of hospital stay for the various operative groups are given in [Table/Fig-4]. A significant difference in time taken for surgery (p<0.001) was noted when comparing retrorectal (59.0min; SD±15.47min) and preperitoneal (64.5min; SD±16.00min) repairs with onlay repair (48.8min; SD±8.63min), whereas difference between retrorectal and preperitoneal repairs was not (p=0.091). There was no significant difference in pain scores between the treatment groups (p=0.571) even after excluding potentially confounding factors such as SSO (p=0.492).
The different modalities of repair performed and their surgical outcomes.
| Type of Repair Performed | p-value |
|---|
| Onlay | Retrorectal | Preperitoneal |
|---|
| N | 112 | 45 | 42 |
|---|
| Operating Time (in minutes) | 48.8 (±8.63) | 59.0 (±15.47) | 64.5 (±16.00) | <0.001 |
| Drain insertion | 95 (84.8%) | 21 (46.7%) | 16 (38.1%) | <0.001 |
| Pain Score on Day 5 | 3.5 (±1.07) | 3.1 (±0.83) | 3. 3 (±0.91) | 0.571 |
| Complications | SSO* | 33 (29.5%) | 5 (11.1%) | 4 (9.5%) | 0.005 |
| Seroma | 15 (13.4%) | 1 (2.2%) | 2 (4.8%) | 0.048 |
| Haematoma | 4 (3.6%) | 2 (4.4%) | 1 (2.4%) | 0.872 |
| SSI** | 15 (13.4%) | 2 (4.4%) | 1 (2.4%) | 0.050 |
| Hospital Stay (in days) | 6.0 (±1.81) | 4.5 (±1.75) | 4.4 (±1.58) | <0.001 |
| Follow-up Period (in months) | 16.2 (±8.30) | 16.4 (±7.69) | 14.7 (±9.39) | 0.580 |
| Recurrence (as % of N) | 12 (10.7%) | 1 (2.2%) | 2 (4.8%) | 0.142 |
| Mean Time before Recurrence (in months) | 13.0 (±3.69) | 18.0 (-) | 22.5 (±2.12) | 0.012 |
| Recurrence Range (in months) | 6-18 | - | 21-24 | |
*SSO – Surgical Site Occurrences
**SSI – Surgical Site Infections
Independent Student t-test for continuous variables and Chi-square test for categorical variables were used to test statistical significance. p < 0.05 was considered statistically significant.
A significantly higher incidence of SSO was observed in the onlay repair group (p=0.005). This was due to significant increase in incidence of seroma formation (p=0.048) and surgical site infection (p=0.05). Differences in haematoma formation were insignificant between the groups (p=0.872). A significantly longer duration of hospital stay was noted in the onlay group (p<0.001).
Females were significantly more likely to develop surgical site infection (p=0.009) but, not seromas or haematomas. Obesity was associated with significantly longer operating times (p=0.01), higher incidence of SSO excluding haematoma formation (p<0.001), postoperative pain (p<0.001) and duration of hospitalization (p<0.001). In diabetics, risk of seroma formation (p=0.043) and SSI (p=0.008), pain (p=0.011) and prolonged hospital stay (p<0.001) was significantly more.
Incisional hernia repair, irrespective of the type of surgical modality used, was associated with significantly longer operating time (p<0.001), greater pain scores (p=0.005), SSO rates (p=0.035) and duration of hospital stay (p<0.001) [Table/Fig-5].
Surgical Site Occurrences for the types of sugery and types of hernia.
Mean follow-up period was 15.9 months (range 3–36 months; SD±8.39 months). During this period, 15 patients (7.5%) developed recurrence.
Discussion
Ventral hernias represent a heterogeneous variety of entities, each with unique clinical and pathophysiological characteristics. The tendency to affect individuals irrespective of age, gender and ethnicity, frequently in the setting of multiple comorbidities, their negative impact on quality of life and the considerable morbidity and mortality associated with complications, necessitate a comprehensive understanding of these conditions.
In this study, most ventral hernias were noted to arise in the economically productive age group of 31-50 years which is comparable with existing literature [18,19]. This has far-reaching implications, especially in developing countries, wherein disease-related morbidity and negative surgical outcomes add to healthcare costs and overall economic burden, adversely affecting productivity and quality of life. Moreover, age over 80 years has been observed to be an independent predictor of overall morbidity and mortality following repair [20].
Although, a female predominance was observed, this distribution was not significant with regard to hernia type. These results are in agreement with present data [21,22]. Although, older literature suggests a significantly higher prevalence of umbilical and incisional hernias in females and epigastric hernias in males, analyses of current data on ventral hernias reveal a growing trend towards male predominance [5]. An increasing incidence of obesity in men, reduced parity in women and a longer life expectancy are possible explanations [4].
Lack of a unifying, comprehensive hernia classification system has hindered advances in our understanding of these diverse disorders. The European Hernia Society classification and, more recently, the ventral hernia staging system are attempts in this direction [16,23]. Stratifying these hernias based on factors affecting surgical outcomes permits comparison between treatment options. In this study, no significant difference in age, gender, presence of major comorbidities, ventral hernia type or defect size was noted between the repair groups, ensuring comparability.
Among the operative parameters considered, mean operative time was significantly lower in the onlay group. This is in agreement with current literature: creation of subcutaneous planes in onlay repair entails less time compared to the extensive dissection associated with underlay repairs [22,24]. There was no significant difference in time taken for retrorectal and preperitoneal repairs.
Pain scores calculated on the fifth postoperative day were not significant between the groups. Due to the frequent use of preemptive anaesthesia in the study population, pain severity was not assessed earlier. Currently, data regarding pain outcomes are conflicting [9,19]. Extent of dissection involved in underlay repairs has been cited as the cause of higher pain scores in this group. However, extensive tissue undermining and the resulting devitalization of tissues and wound-related complications can be a cause for pain in patients undergoing onlay repair [18].
The term SSO was coined by the Ventral Hernia Working Group, and encompasses all perioperative wound events including infection (cellulitis and SSI), sterile fluid collections (seromas and haematomas), wound dehiscence, and enterocutaneous fistulae [25].
Seromas are common complications following ventral hernia repair. The incidence varies in literature with studies quoting figures of 14% for onlay and 2% for underlay [26,27]. Although the majority resolves spontaneously, 30-35% may be symptomatic, requiring percutaneous aspiration [28]. Compression dressings in the immediate postoperative period are known to reduce seroma incidence.
Skin necrosis is a complication almost unique to onlay repairs. Extensive tissue handling involved in flap dissection has been known to disrupt perforating vessels, compromising the vascularity of overlying skin. Excision of necrosed margins and serial debridement under antibiotic cover facilitates closure by secondary intention [29].
SSI rates range from 7-13% for onlay and 4-11% for underlay [19,26,27]. Incidence of mesh infection in ventral hernia repair has been reported to be under 1%, with older age, obesity and diabetes being recognized risk factors [28,30]. Macroporous prostheses are associated with lesser infection rates and increased mesh salvage rates in open repair [31].
In this study, a significantly higher SSO rate, specifically regarding seroma formation and SSI, were observed in the onlay group. These results are in accordance with other studies [15,22].
Most surgical site infections were superficial and resolved with antibiotics, percutaneous drainage and regular dressing. In the onlay group, one case of deep SSI was encountered which responded to conservative management and did not require mesh removal.
Skin necrosis was noted in five patients in the onlay group. There was no evidence of fistula formation in any of the patients in the postoperative period. Duration of hospital stay was reflective of the incidence of early postoperative complications and response to treatment.
Generally, recurrence rates tend to be lower with underlay (0-5%) compared to onlay repairs (12-15%) [19,27]. However, these figures are highly variable and depend on patient age, presence of risk factors, type of hernia, and history of prior repair. Surgery-related factors include choice of improperly sized prostheses, inadequate overlap of the fascial margins and failure to identify and correct occult hernias [28]. Longer periods of follow-up are advantageous in determining the true efficacy of a surgical repair. In a prospective study, 67% of recurrences following open repair occurred within one year of surgery and 77% within the second year [21].
Recurrence was observed in 15 patients of whom 12 had undergone onlay repair. Of these, six recurred within one year and the rest within two years. Incidence could not be calculated for this study as a significant proportion of patients were lost to follow-up. Loss of ≥20% has been shown to reduce the validity of observed results in prospective studies [32].
Retrorectal and preperitoneal repairs were similar with respect to operative parameters and surgical outcomes. These findings suggest that the ideal position for prosthesis placement is underlay (either retrorectal or preperitoneal). Onlay involves extensive tissue undermining and superficial mesh placement (facilitating bacterial colonization), which results in higher SSO rates. Moreover, pressure required to dislodge the mesh from an onlay position is less when compared to underlay (Pascal’s law), predisposing for higher recurrence rates [7]. Depth of the retrorectal space and greater vascularity accelerate tissue ingrowth, preventing infection [12,33].
Nevertheless, onlay repair may be one of the few options available in cases where multiple previous surgeries or a hostile abdomen preclude retrorectal or preperitoneal dissection. Moreover, the procedure is simple, operative time shorter and direct contact with the bowel is avoided, aspects which prove advantageous especially in elderly and seriously ill patients [7].
Prevention by controlling modifiable risk factors has assumed greater importance in recent times.
A number of co-morbid conditions can predispose to ventral hernia formation and influence surgical outcomes. Foremost among these are advanced age, obesity, chronic pulmonary disease, diabetes mellitus, ascites and multiparity [5,34]. These conditions coupled with a history of multiple procedures, wound infection and impaired healing give rise to incisional hernias [2,6].
Obesity has been implicated in a number of studies both as a risk factor for hernia occurrence as well as for recurrence after repair. Excessive fat deposition raises the intra-abdominal pressure, separates muscle bundles and weakens aponeurosis. Obese individuals are also at higher risk of developing cardiopulmonary, surgical site and mesh-related complications and chronic pain in the postoperative period [35]. Poor vascularity, impaired wound healing and altered biomechanics are likely explanations [36]. Weight reduction prior to surgery has been shown to minimize procedure-related morbidity in the short-term as well as decrease recurrence rates. All patients undergoing hernia repair should be counselled regarding the potential complications associated with obesity [37]. Laparoscopic hernia repair is an accepted alternative in this subset of patients [35,36,38].
In this study, obesity and diabetes were associated with significantly higher incidence of SSO, seroma formation and SSI possibly accounting for the higher postoperative pain scores, duration of hospital stay and recurrence rates observed in these patients. Obesity and diabetes as significant predictors of morbidity in patients undergoing elective repair have been observed in multiple studies [34,39].
Incisional hernia repairs had significantly longer operating time, more postoperative pain, wound-related complications and duration of hospitalization, irrespective of surgical technique. Eleven of the 15 patients who developed recurrence had been operated for incisional hernia. Significantly greater age and larger defect size compared to primary hernias could explain these findings. Thus, prior surgery can be considered a negative prognostic factor in terms of surgical outcomes. Sound surgical technique and the use of a 4:1 suture-to-wound length ratio have been shown to significantly reduce incidence of incisional hernias [40]. Its relevance, especially in other surgical specialties, is evident in this study wherein 67.2% of incisional hernias were secondary to gynaecological procedures [19].
Thus, a one-size-fits-all approach to patients with ventral hernias may not suffice in achieving desired results. Relevant procedure-related factors including optimal anatomical approach need for prosthesis, the ideal material and the location for placement need to be considered.
Patient-related factors which have a bearing on surgical outcomes include age, presence of comorbidities, and history of prior repairs, hernia characteristics and presence of complications.
Outcomes fall below expectations when all factors are not taken into consideration.
The reconstructive options for ventral hernias are diverse. The surgeon should be familiar with several techniques and tailor the procedure according to patient-specific requirements.
Limitation
A limitation of this study was the variable follow-up period. A significant proportion of our patients were lost to follow-up. Incidence of chronic pain and impact on quality of life were not assessed.
Conclusion
Today, prosthetic repairs have significantly reduced recurrence rates when compared to primary tissue repairs and are indicated in all but the smallest of ventral hernias. In this study, underlay repair was associated with significantly lower wound-related complications compared to onlay repair. Obesity, diabetes and previous surgery were important risk factors adversely affecting surgical outcomes. Thus, in the setting of small, uncomplicated ventral hernias, the underlay repair, with acceptable SSO and recurrence rates, may be considered the procedure of choice compared to other open techniques. However, a one-size-fits-all approach cannot be applied to all patients with ventral hernias. An in-depth knowledge of the various surgical options, approaches and meshes available matched by a thorough understanding of patient comorbidities and hernia characteristics is crucial in selecting the right operation for the right patient and achieving satisfactory surgical outcomes.
*Independent Student t-test for continuous variables and Chi-square test for categorical variables were used to test statistical significance. p < 0.05 was considered statistically significant.
*SSO – Surgical Site Occurrences
**SSI – Surgical Site Infections
Independent Student t-test for continuous variables and Chi-square test for categorical variables were used to test statistical significance. p < 0.05 was considered statistically significant.