Temporomandibular (TMJ) disorders and pain has been identified as a major health problem worldwide. It is estimated that about 20%-30% of the adult population worldwide suffer from temporomandibular dysfunction [1]. Craniofacial pain affects approximately 10%-15% of adult population [2]. TMJ disorders present with pain and stiffness which causes functional limitation of the joint which ultimately affect the quality of life of the patient and have an impact on the activities of daily living [3]. Chronic pain can have variable causes like nociceptive, neuropathic, ischemic, and visceral or may even exhibit a combination of different aetiologies. A complex interaction of various intrinsic and extrinsic factors can induce persistent oro-facial muscle pain and TMJ dysfunction [4]. Patients report with varied symptoms including sleep disturbances and disruptions, decreased physical function and productivity, anxiety, depression etc., [5]. There are a number of methods used to diagnose temporomandibular disturbances most of which include a detailed clinical examination and radiographs. Moreover, the most common and reliable symptom of any TMJ disturbance is ‘pain’. But pain is a subjective experience and information about pain, its intensity, and description can only be explained by the patient. Self-reporting scales of pain assessment prove to be extremely useful in such cases [6].
These symptoms have an adverse impact on the specific activities of daily living and general life of the patient. Sheldon was the first to make reference to “Activities of daily living” in the Journal of Health and Physical Education in 1935 [7] and they signify the activities the person undertakes as a part of daily life. They are divided into physical ADL and Instrumental Activities of Daily Living (IADL) [8]. An ADL questionnaire is considered as a simple and fairly reliable tool for pain assessment. A number of rating scales are used to measure pain associated with TMJ and craniofacial pain over the years. Katz S et al., designed an ADL scale primarily to measure the ability to carry out the basic activities of daily living, which was later modified for specific use in patients with TMJ disorders [9]. Clark GT et al., published a Visual Analog Scale (VAS) for jaw pain and function questionnaire in 1989 which consists of 8 questions about pain, 5 about jaw dysfunction and 18 about daily activities [10].
Several serum markers are considered highly sensitive markers of bone metabolism and these have been used to assess bone changes and TMJ disorders [11,12]. Vitamin D (25(OH) D) is known to play an important role in calcium and bone metabolism. Vitamin D deficiency has been linked to poor physical performance, lower muscle strength and ADL disability [13]. Although few studies have been carried out to understand the relationship between TMJ discomfort and serum 25(OH) D [3,14-16] none have explored the relationship in an Indian Population. This study was designed to ascertain the relationship between serum vitamin D 25(OH)D levels and pain and discomfort with respect to TMJ during the ADL amongst controls and vitamin D deficiency patients in an Indian hospital based population in Mumbai, Maharashtra, India.
Materials and Methods
The exploratory study was approved by the Institutional Ethics Committee of Nair Hospital Dental College, Mumbai, Maharashtra, India, and was carried out over a period of 21 months from June 2014 to March 2016. All the participants in the study were explained about the study and written informed consent in the language best known to the patient was obtained before the start of the study. The research has been conducted in full accordance with the World Medical Association Declaration of Helsinki.
The study was conducted on patients who reported to the Department of Oral Medicine and Radiology on an outpatient basis. As no reference was available for such a study in an Indian population, a total of 100 patients were randomly selected for the study. Although, vitamin D deficiency affects the TMJs but recently, the term vitamin D insufficiency has been used to describe suboptimal levels of serum 25(OH) D, which may be associated with various other disease outcomes. Since, a number of factors like race, vitamin D intake, sun exposure, adiposity, age, and physical activity etc. are known to influence 25(OH) D levels, precisely defining the values for vitamin D deficiency or insufficiency is debatable. But the American Journal of Clinical Nutrition in 2006 concluded that most beneficial levels of 25(OH) D start at 30 ng/ml. And so a cut-off value of 30 ng/mL was used in the current study to include the samples in the group [17,18]. Based on this criterion 50 patients were categorized as controls and 50 patients were classified into Vitamin D deficiency.
Inclusion Criteria for Samples
Population from both the sexes.
Patients of 25-70 years with complaint of TMJ pain/discomfort but no known diagnosis that may affect the bones/joints/ TMJ and undergoing routine blood investigations were included.
Exclusion Criteria
Patients below 25 years of age and above 70 years of age.
Patients having relative morbidity in terms of bone neoplasms etc.
All the participants were asked to evaluate the pain and discomfort experienced by them during the ADL. The rating scale used was the scale based on methods elaborated in medical and behavioral science and modified by List T and Helkimo M [19]. The scale was defined as 0 (activity without any pain/discomfort in the TMJ) to 10 (Activity impossible due to pain/discomfort in the TMJ) and the number that best described their level of discomfort was marked.
The questionnaire validated to be used for TMJ [16,19-22] was as follows:
If you feel pain/discomfort in the area of TMJ, are you able to:
(ADL 1): Socialize with family and close friends?
(ADL 2): Perform daily work?
(ADL 3): Perform daily household chores (preparing meals, cleaning, taking care of small children)?
(ADL 4): Sit in a company or participate in other social activities (e.g., parties)?
(ADL 5): Exercise (walk, bicycle, jog, etc.,)?
(ADL 6): Perform hobbies (read, fish, knit, play an instrument)?
(ADL 7): Sleep at night?
(ADL 8): Concentrate?
(ADL 9): Eat (chew, swallow)?
(ADL 10): Talk (laugh, sing)?
(ADL 11): Yawn, open mouth wide?
(ADL 12): How much does the pain/discomfort affect your daily activities?
The biochemical marker 25(OH)D, was assessed to identify and measure the quantitative changes in bone turnover [16]. The values from the reports of the patients who visited the outpatients department were assessed statistically to correlate with age, gender and TMJ discomfort.
Statistical Analysis
Variables were evaluated for statistical differences between male and female groups with ANOVA test. Significance of correlation was tested using Spearman rank correlation coefficient. A level of significance of 0.05 was considered to be significant.
Results
Among the 100 participants in the study, 61 were females and 39 were male. The gender vise distribution in the samples and controls is given in [Table/Fig-1]. The mean age of the participants was 48.98 years, while the mean age in the controls was 52.96 years and in samples was 45.0 years.
Gender wise distribution of the participants (samples and controls).
| GenderDistriburion | Samples | Conrols |
|---|
| Females | Males | Females | Males |
|---|
| Number | 30 | 20 | 31 | 19 |
| Percentage | 60% | 40% | 62% | 38% |
The influence of TMJ discomfort on the activities of daily living among the samples and controls is given in [Table/Fig-2].
[Table/Fig-3] shows the relationship of distribution of significance between ADL data and vitamin D.
Influence of TMJ pain on ADL.
| ADL | Samples | Controls |
|---|
| Female | Male | Female | Male |
|---|
| Median | IQR | % | Median | IQR | % | Median | IQR | % | Median | IQR | % |
|---|
| ADL 1 | 0 | 2 | 31.43 | 0 | 0 | 19.05 | 0 | 0 | 6.45 | 0 | 0 | 0.00 |
| ADL 2 | 0 | 3 | 34.29 | 0 | 0.5 | 23.81 | 0 | 0 | 12.90 | 0 | 0 | 0.00 |
| ADL 3 | 0 | 4 | 31.43 | 0 | 0 | 19.05 | 0 | 0 | 12.90 | 0 | 0 | 0.00 |
| ADL 4 | 0 | 3 | 31.43 | 0 | 0 | 14.29 | 0 | 0 | 6.45 | 0 | 0 | 0.00 |
| ADL 5 | 0 | 4 | 28.57 | 0 | 0 | 19.05 | 0 | 0 | 9.68 | 0 | 0 | 0.00 |
| ADL 6 | 0 | 5 | 31.43 | 0 | 0.5 | 23.81 | 0 | 0 | 3.23 | 0 | 0 | 0.00 |
| ADL 7 | 0 | 5 | 45.71 | 0 | 2 | 33.33 | 0 | 1 | 25.81 | 0 | 0 | 21.05 |
| ADL 8 | 0 | 4 | 42.86 | 0 | 1.5 | 33.33 | 0 | 0 | 19.35 | 0 | 0 | 5.26 |
| ADL 9 | 0 | 5 | 48.57 | 1 | 4 | 57.14 | 0 | 0 | 9.68 | 0 | 0 | 5.26 |
| ADL10 | 0 | 5 | 48.57 | 1 | 3 | 57.14 | 0 | 0 | 9.68 | 0 | 0 | 0.00 |
| ADL11 | 2 | 6 | 60.00 | 2 | 3 | 85.71 | 0 | 1 | 29.03 | 0 | 1 | 26.32 |
| ADL12 | 1 | 5 | 60.00 | 2 | 2.5 | 80.95 | 0 | 0 | 12.90 | 0 | 0 | 0.00 |
IQR: Interquartile range
ADL Scale: 0-12 where 0=activity without any pain/discomfort and 12 = activity impossible
%=percentage of observation exceeding 0
Distribution of significance between ADL data and vitamin D.
(p): Distribution of significance
ADL: Activities of Daily Living
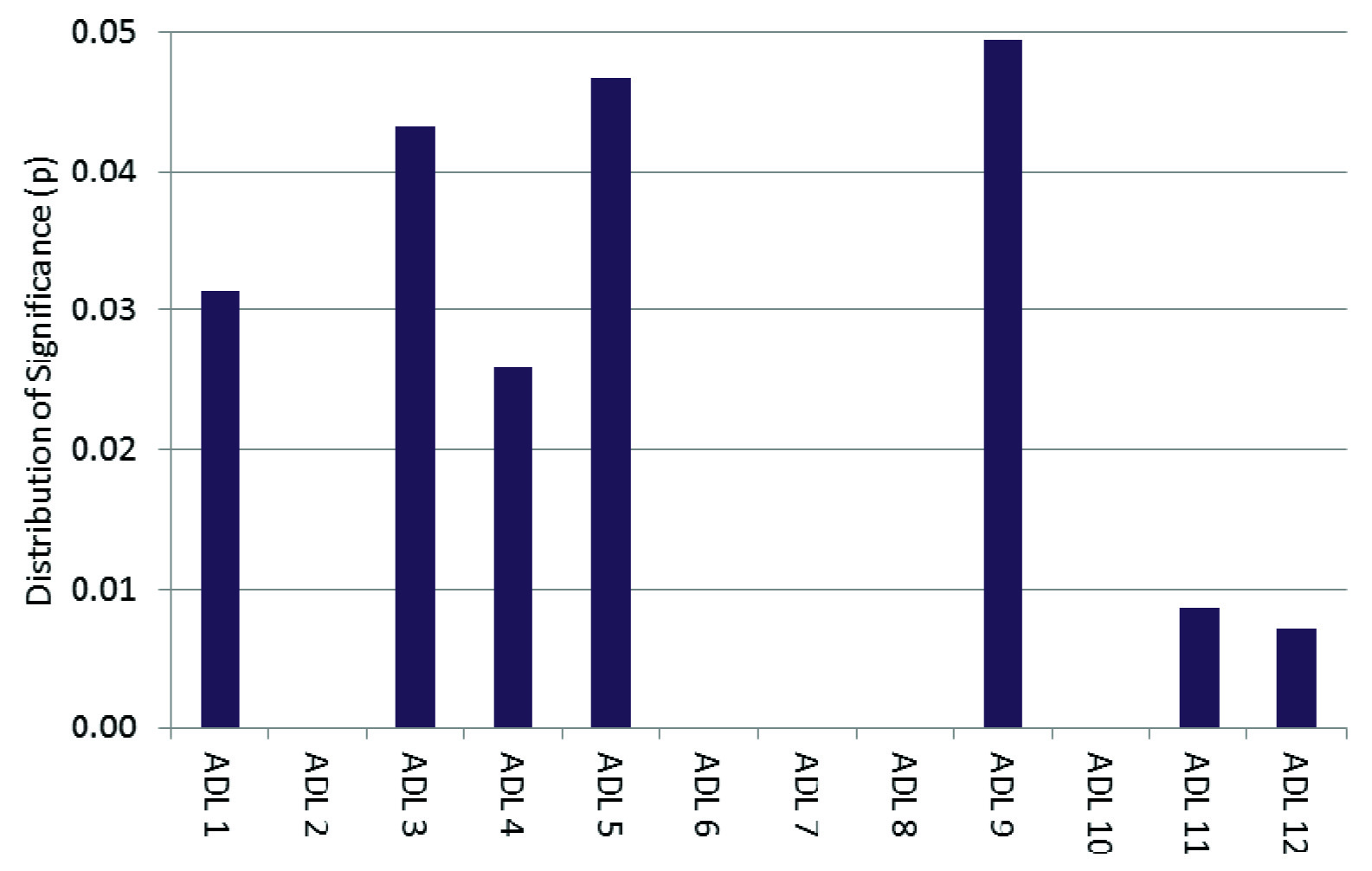
The values of distribution of significance (p) of individual ADL and vitamin D levels determined by Spearman correlation statistical test is seen in [Table/Fig-4] shows that the p-value was significant for ADL 1, ADL 3, ADL 4, ADL 5, ADL 9, ADL 11 and ADL 12.
Spearman correlation test p-values for individual ADL questions.
| ADL QUESTIONS | ADL 1 | ADL 2 | ADL 3 | ADL 4 | ADL 5 | ADL 6 | ADL 7 | ADL 8 | ADL 9 | ADL 10 | ADL 11 | ADL 12 |
|---|
| p-values | 0.031 | 0.142 | 0.043 | 0.026 | 0.047 | 0.115 | 0.099 | 0.066 | 0.049 | 0.068 | 0.009 | 0.007 |
[Table/Fig-5] Represents the distribution of serum vitamin D in the samples and controls and the variations seen in the gender.
Serum levels of vitamin D (nmol/L) in the studied population.
| Gender | Samples | Control |
|---|
| Median | IQR | Median | IQR |
|---|
| Female | 17.39 | 13.05 | 37 | 15.62 |
| Male | 16.60 | 16.04 | 37.50 | 33.43 |
IQR: Interquartile range
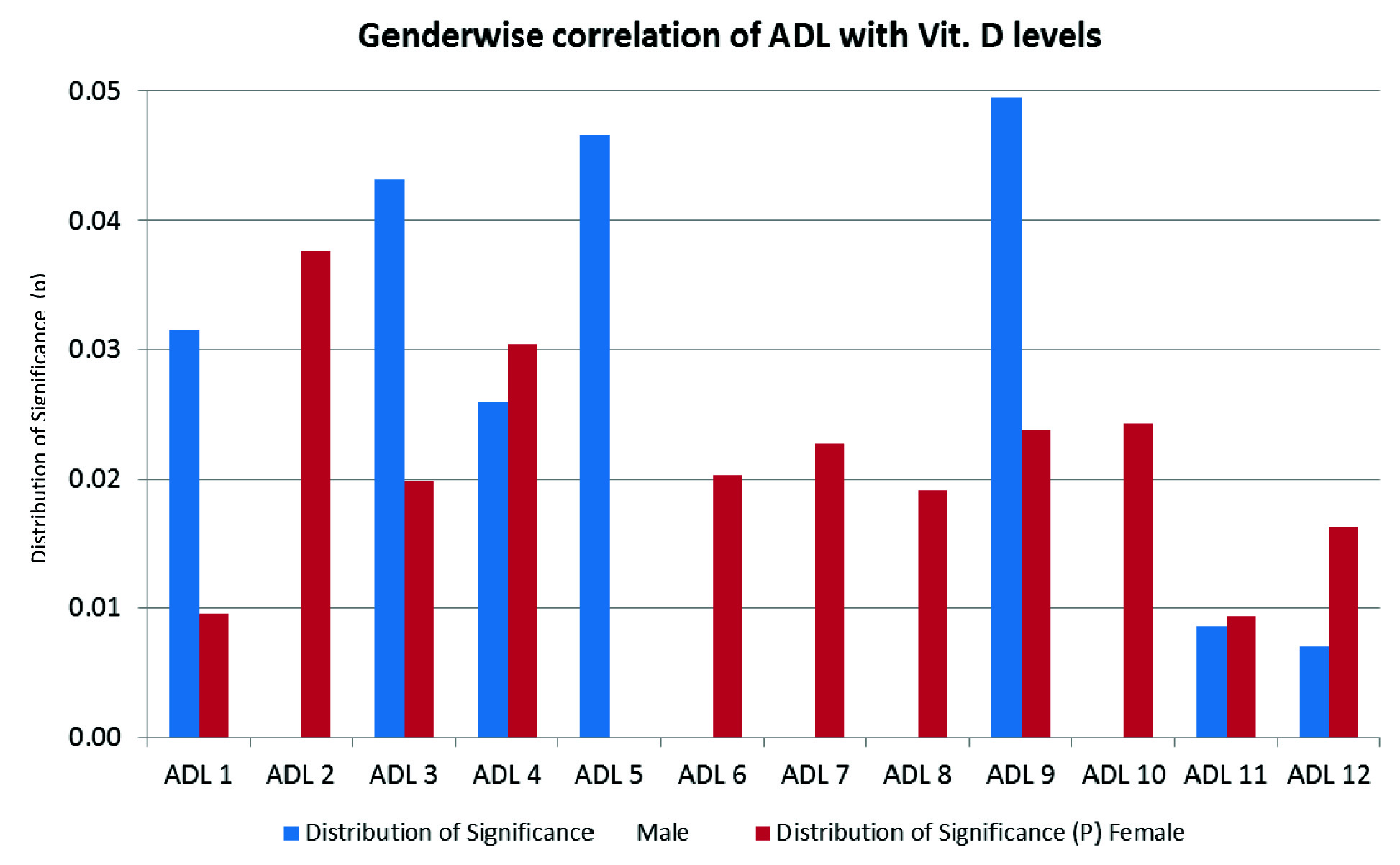
The vitamin D levels and ADL scores showed significant difference in the sexes that are represented in [Table/Fig-6]. These differences can be attributed to a number of socioeconomic and socio-cultural factors such as a more indoor lifestyle in women in developing countries etc.
Gender wise correlation between vitamin D levels and ADL.
Discussion
This population based exploratory study was carried out over a period of 21 months in the city of Mumbai. The results of our study demonstrated that low serum vitamin D levels were associated with TMJ pain and/or discomfort, which had a significant negative impact on the various ADL of the participants.
TMJ pain and disorders have been identified to be caused by a complex interplay of multifactorial factors. Physical occlusal interferences, psychological factors, habitual activities, work, interpersonal activities, psychological state and mental health of the patient, psychological disturbances like notable depression, somatisation, psychological distress and even general nutrition and health is also known to have an effect on the TMJ [23-26].
The serum 25(OH)D levels of the participants were evaluated as vitamin D or serum 25(OH)D is a biological marker that provide an accurate quantitative as well as qualitative indicator of bone metabolism and health [15,16, 27-29]. In the current study, the vitamin D levels in women, both in samples and controls were lower than the male participants. A number of studies indicate that vitamin D3 deficiency predisposes the individual to TMJ disorders and musculoskeletal pain which has a definitive effect on the quality of life [15,27].
The Spearman’s correlation coefficient was calculated, to find a correlation between TMJ discomfort using ADL scale, and the levels of serum vitamin D. vSimilar results were seen in few other studies [30,31]. Jagur O et al., reported significant relationships between all the ADL questions except ADL 10 as it was omitted in the study in the population of Estonia in 2012 [3]. Voog U et al., in their study reported that TMJ involvement in patients suffering from rheumatoid arthritis had a serious impact on the activities of daily living and the quality of life [20].
In the current study, highest significance was seen with respect to ADL 11(yawn, open mouth wide). Participants of both genders reported maximum discomfort while yawing or opening mouth wide; however, more significant results were seen in the female participants. This finding was also in accordance to the study by Jagur O et al., [3]. This was followed by the ADL 2 and ADL 4 which signifies and emphasises how TMJ pain and discomfort affects the social life and ability of the patients to socialise. These findings were also in accordance with a number of studies carried out worldwide [3,20].
Significant differences were also noted when the ADL scores were compared between both the genders. Correlation between low serum vitamin D levels and ADL were found to be more in females as compared to males. The correlation of vitamin D levels in females was found to be significant with all ADLs except ADL 5 (p>0.05). The high significance in women while performing daily chores {ADL 3} was in contrast to the values reported by Jagur O et al., and can be linked to the lifestyle of the female population in India [3]. In the current study the female population also showed a high significance in ADL 6 {Perform hobbies (read, fish, knit, play an instrument)}and ADL 7 {Concentrate}, while the male participants showed a significant correlation in ADL 1, ADL 3, ADL 4, ADL 5, ADL 9, ADL 11 and ADL 12. This was in accordance to the study by Bagis B et al., which also showed a higher incidence of TMJ pain and disorders in women [32].
The incidence of craniofacial pain disorders is seen to be 1.5 to 2 times higher in women than in men [3,33,34]. The differences in the TMJ discomfort can not only be related to vitamin D levels, but also to the qualitative differences in endogenous pain inhibitory systems, the influence of gonadal hormones [35] and also to some psychological factors like sex role beliefs, pain coping strategies, pain related expectations etc [36].
Although, the participants’ age could not be correlated significantly to the ADL questions, but the rating scores were found to be much higher in middle aged participants especially middle age women. This could be attributed to the fact that with progressing age (post 45 years of age) remodeling of bone and arthritis can lead to TMJ changes which can also cause symptoms like pain and negatively affect the quality of life [37-39].
Limitation
The current study was carried out on a small sample size and further studies with more sample size would substantiate the findings. In the current study, the sampling technique used was not age and sex matched for the samples and controls.
Strength
It is a pioneering study in the field of understanding TMJ discomfort and first of its kind to be carried out in an Indian urban population.
Future Recommendation of Study
Along with vitamin D, the relationship of other serum parameters, enzyme linked proteins, genetic markers and bone markers can be explored with TMJ discomfort and ADL. Post supplementation studies can be carried out to ascertain the influence of vitamin D on the TMJ and ADL.
Conclusion
The results of this study indicate that vitamin D {serum 25(OH) D} level has a significant impact on the TMJ pain/discomfort. Although self-reporting questionnaires cannot replace the evaluation of patient’s medical history, physical examinations, radiographs and other laboratory tests, it provides a reliable insight into the patient’s pain experiences and state of well-being.
It was also noted that the serum 25(OH)D levels reported in females were much lesser in comparison to the male participants and the TMJ pain/discomfort noted through the ADL questionnaire was more significantly correlated to the serum vitamin D levels in females than in males. Finally, it can be noted that the experience of TMJ pain and discomfort significantly affect the patient’s ADL and have a negative impact on the social and personal life of patients and can also affect the psychological status of the individual.
IQR: Interquartile range
ADL Scale: 0-12 where 0=activity without any pain/discomfort and 12 = activity impossible
%=percentage of observation exceeding 0
IQR: Interquartile range