Imaging Diagnosis of Metastases to Breast: A Rare Presentation of Carcinoma Gallbladder
Neha Antil1, Shabnam Bhandari Grover2, Amit Katyan3, SP Kataria4, Geetika Khanna Bhattacharya5
1 Senior Resident, Department of Radiology and Imaging, VMMC and Safdarjung Hospital, New Delhi, India.
2 Professor and Head, Department of Radiology and Imaging, VMMC and Safdarjung Hospital, New Delhi, India.
3 Senior Resident, Department of Radiology and Imaging, VMMC and Safdarjung Hospital, New Delhi, India.
4 Professor, Department of Medical Oncology, VMMC and Safdarjung Hospital, New Delhi, India.
5 Professor, Department of Pathology, VMMC and Safdarjung Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shabnam Bhandari Grover, E-81, Kalkaji, New Delhi-110019, India.
E-mail: shabnamgrover@yahoo.com
Breast metastases are extremely rare with a reported incidence of only 0.5-6.6% of all breast malignancies. We report a case of bilateral breast metastases in a 45-year-old lady who presented with an ulcero-proliferative epigastric mass. Imaging features suggested a diagnosis of carcinoma gallbladder as the primary aetiology. The diagnosis was proven by biopsy from the epigastric mass lesion. It is extremely rare to find breast metastases from carcinoma gall bladder and very few similar cases have been reported in the literature.
Breast metastases, Epigastric mass, Imaging features
Case Report
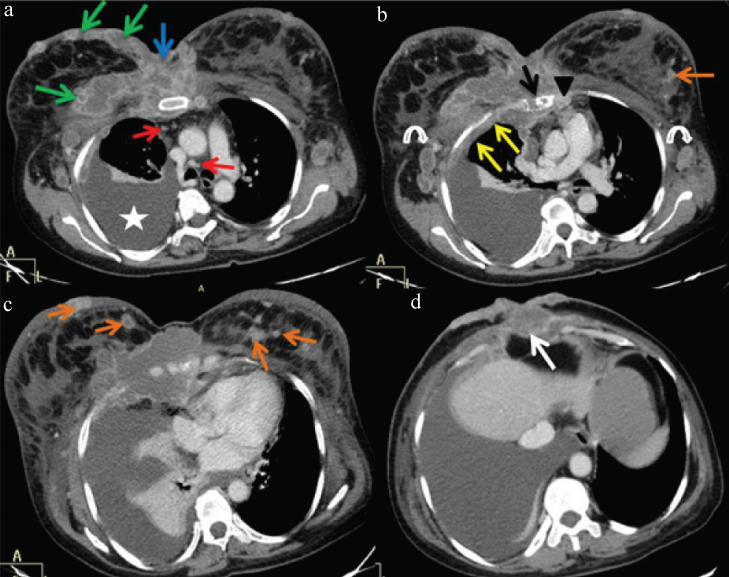
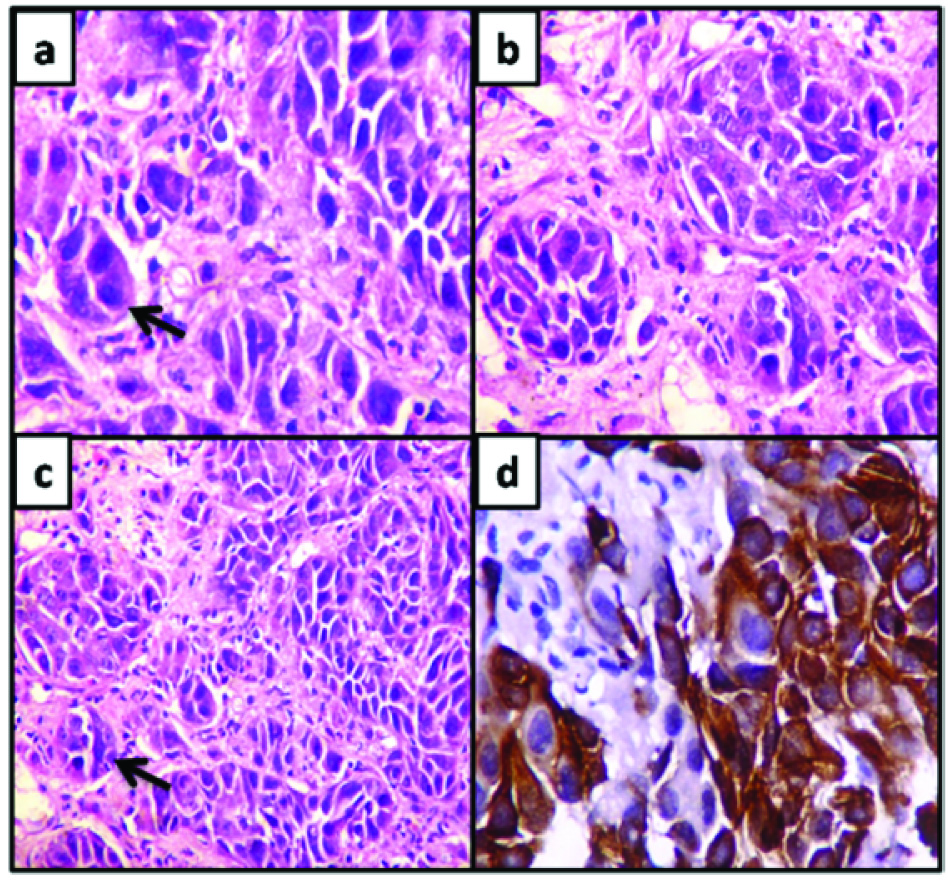
A 45-year-old post-menopausal female, resident of North India, presented with an ulcero-proliferative mass in the epigastric region accompanied by multiple masses in both breasts for the past one year [Table/Fig-1]. On examination, the epigastric ulcero-proliferative mass was seen to extend into the midline chest wall and the right breast. Additionally, multiple nodules of firm consistency were palpable in the skin and subcutaneous tissue of both breasts. On persistent enquiry, the patient submitted a history of laparoscopic cholecystectomy for cholelithiasis, performed two years earlier at some other hospital. However, the previous relevant medical records were not available. The clinical team suspected occult primary malignancy with metastasis. A prompt routine laboratory and radiological evaluation was resquisitioned which included ultrasound of both breasts, CT study of thorax and abdomen. Laboratory parameters were found to be within normal limits. Ultrasound of both breasts revealed multiple well-circumscribed hypoechoic masses with size ranging from 5 mm to 5 cm visualized in the skin, subcutaneous plane and the parenchyma of both the breasts. These masses had fine lobulations and distinct echogenic rim [Table/Fig-2]. On colour Doppler, these breast masses showed peripheral and central vascularity [Table/Fig-2]. CT examination of thorax and upper abdomen corroborated the ultrasound observations of bilateral multiple subcutaneous and parenchymal breast masses with bilateral axillary lymphadenopathy. A heterogeneously enhancing mass lesion was seen at the laparoscopic port site involving skin, subcutaneous tissue and abdominal wall muscles. No recurrent tumour was seen in the gall bladder fossa. The port-site mass lesion was seen to extend cranially into the midline of the chest wall with associated sternal destruction. There was contiguous extension of the port-site lesion into the right breast, anterior mediastinum and right anterior costal pleura. Mediastinal lymphadenopathy along-with massive right sided pleural effusion was also observed [Table/Fig-3]. Based on imaging observations, a diagnosis of gall bladder carcinoma with port site recurrence showing contiguous spread to chest wall, mediastinum and right breast with non-contiguous metastasis to breast, axillary and mediastinal lymph nodes was made. Ultrasound guided trucut biopsy of the epigastric mass lesion was obtained. The histopathological and immunohistochemistry analysis revealed primary moderately differentiated adenocarcinoma of gallbladder with Pan cytokeratin and CK7 positivity [Table/Fig-4]. Patient was managed with palliative radiotherapy and chemotherapy; however, she succumbed to her disease within six months.
Clinical photograph shows multiple ulcero-proliferative lesions involving the epigastric region, midline chest wall with multiple skin nodules in both breasts.

Ultrasound of the right breast shows multiple hypoechoic breast masses with heterogenous internal echotexture. The margins of these lesions show fine, well defined echogenic lobulations (red arrows). There is no spiculation, architectural distortion or posterior acoustic shadowing. Colour Doppler imaging demonstrates peripheral and central vascularity within these mass lesions.

Axial CECT thorax and upper abdomen; a-b) shows a large heterogeneously enhancing mass lesion in the midline chest wall (blue arrow), right breast (green arrows), mediastinum (black arrowhead) and anterior costal pleura (yellow arrows) along with erosions of bilateral lateral edges of sternum (black arrow). Additional note is made of mediastinal lymphadenopathy (red arrows), bilateral axillary lymphadenopathy (white curved arrows) and right sided massive pleural effusion (white star); c) shows noncontiguous multiple well circumscribed heterogeneously enhancing bilateral breast metastasis in the skin, subcutaneous plane and parenchyma (orange arrows); d) shows a large heterogeneously enhancing mass lesion arising at the laparoscopic port site (white arrow).
Histopathology study (a,b,c) show atypical epithelial cells arranged in clusters with multiple foci of glandular pattern (black arrows). The cells show marked pleomorphism, moderate basophilic cytoplasm and prominent nucleoli (H&E; 200x). Immuno-histochemical analysis; (d) reveals a moderately differentiated adenocarcinoma with Pan cytokeratin and CK 7 positivity (H&E; 200x).
Discussion
Breast is the most common site for primary cancers in adult females; however, it is an extremely rare site for metastases from extramammary primary malignancies. The incidence of breast metastasis is extremely low accounting for 0.5%-6.6% of all breast malignancies [1]. We report a rare case of metastases to the breast from a primary carcinoma of the gallbladder. Gall bladder malignancy characteristically spreads in a contiguous manner into the loco-regional structures. A PUBMED search of primary gall bladder carcinoma with distant metastasis to breast, revealed a few such clinical reports [1-4].
The breast is largely composed of fibro-fatty glandular tissue with relatively poor blood supply. This explains the rarity of occurrence of metastases to breast which occurs through haematogenous or lymphatic route [5]. Breast metastases carry a dismal prognosis with most cases showing an average survival of only 10-12 months, with a 100% mortality rate within 3 years [2]. There is a huge diversity of extramammary primary malignancies metastasizing to the breast which in order of decreasing frequency are lymphoma, melanoma, rhabdomyosarcoma, lung tumours, ovarian tumours and carcinoma stomach [1]. Uncommonly, primary carcinoid tumour, hypernephroma, carcinoma of liver, tonsil, pleura, pancreas, cervix, perineum, endometrium and urinary bladder has also been reported [4]. Gall bladder carcinoma is an extremely rare primary site for metastases to breast [1-4].
Current epidemiological studies showed gall bladder to be the sixth common cancer of the gastrointestinal system in the world and represents 80-95% of biliary tract cancers worldwide [2,6]. Asia is a high risk continent with increased frequency of carcinoma gallbladder in north Indian females [6]. Our patient was also a resident of North India. Primary adenocarcinoma of gall bladder spreads by extension and metastases, the former occurring earlier, with liver being the most common site of direct extension and accounting for 60%-90% of cases [1]. Other organs which can be contiguously involved are duodenum, stomach, colon, pancreas, omentum, abdominal wall, bile ducts and portal vein. Metastases occur via haematogenous route, most frequently to the liver (76%-86%) and via lymphatic/transcoelomic route to the regional lymph nodes in about 60% of cases. Extra-abdominal metastases from gall bladder carcinoma are rare and lung is the most frequently reported site. Rare sites of metastasis from malignancy of the gall bladder include the heart, orbit, central nervous system, skin, bone, scalp, cervix, kidney, thyroid, and hernia sac [1]. However port site recurrence of gall bladder malignancy has a relatively higher incidence of 14-30% after laparoscopic cholecystectomy for gallbladder cancer and this incidence is believed to be even higher if gall bladder malignancy remains undetected [7,8]. It is postulated by few authors that Laparoscopic surgery provides a potential site for tumour seeding [7-9].
Most of the reports of metastases to the breast highlight the clinical and pathological aspects. Imaging features which distinguish primary malignancy from secondary deposits in breast are less frequently discussed in the literature. Few investigators have reported the X-ray mammogram and ultrasound features of breast metastasis. On mammography, breast metastases are reported to be present without spiculations and can therefore be confused with a benign breast lesion especially in the absence of a known clinical setting. Sonographic features of breast metastases are reported to be well defined masses with a surrounding echogenic rim, usually devoid of architectural distortion, calcifications and posterior acoustic shadowing [5]. These masses are seen to show rapid increase in size on serial imaging. In our patient, we found similar ultrasound features revealing multiple, round to oval shaped, well circumscribed hypoechoic masses with fine lobulations and surrounding echogenic rim. There was no architectural distortion, calcifications and posterior acoustic shadowing. These masses were located in parenchyma, skin and subcutaneous tissue of both breasts. Features of primary breast malignancy such as spiculations, calcifications, architectural distortion and skin edema were conspicuous by their absence.
Although clinical reports of port site recurrence of gall bladder malignancy are abundantly reported in literature [1,4]. The reports on imaging features of this entity are sparse. Winston CB et al., have reported the CT appearances of port site recurrence as enhancing abdominal wall masses majority of which had subjacent omental fat involvement [9]. In our patient, multiple enhancing abdominal wall masses were seen without the involvement of omental fat but with contiguous spread to chest wall, costal pleura and mediastinum. The presence of these masses are characteristically located at a laparoscopic port site which clinched the diagnosis in favor of primary gall bladder malignancy seeding into laparoscopic port tract. Imaging evaluation was therefore valuable not only in documenting the primary site of malignancy as the gall bladder, but also in depicting the extent of malignant disease.
Our report highlights a rare entity, bilateral multiple breast metastases from an unusual primary aetiology for metastasis at this site. The imaging appearances seen in our patient add to the literature on this aspect of the disease which has so far remained rather infrequent.
Conclusion
Metastases to breast from a primary gallbladder carcinoma are rare and our report adds to the literature, another case of this rare entity. The vital role of imaging in unveiling and documenting the primary site as gall bladder is obvious from our report. We also highlight the imaging features for differentiating multiple breast metastases from multiple benign masses. Furthermore, the potential route for metastatic seeding at laparoscopic port site in an occult gallbladder carcinoma as seen in our patient definitely suggests a necessity to review and redefine stringent criteria against the rampant use of laparoscopic cholecystectomy.
[1]. Shukla P, Roy S, Tiwari V, Mohanti BK, Unusual presentation of metastatic gall bladder cancerJ Can Res Ther 2014 10:397-98. [Google Scholar]
[2]. Kumaran D, Anamalai M, Velu U, Nambirajan A, Julka PK, Carcinoma of gall bladder with distant metastasis to breast parenchyma. Report of a case and review of literatureJ Egyptian Nat Cancer Inst 2016 28:263-66. [Google Scholar]
[3]. Malik AA, Wani ML, Wani SN, Malik RA, Malik TR, Breast metastasis from carcinoma of gall bladderInt J Health Allied Sci 2013 2:35-36. [Google Scholar]
[4]. Kallianpur AA, Shukla NK, Deo SV, Singh M, Subi TS, Kapali A, A rare case of gallbladder carcinoma metastases to the breast treated with curative intentTropical Gastroenterology 2012 33:155-58. [Google Scholar]
[5]. Mun SH, Ko EY, Han B-K, Shin JH, Kim SJ, Cho EY, Breast metastases from extramammary malignancies: typical and atypical ultrasound featuresKorean Journal of Radiology 2014 15(1):20-28. [Google Scholar]
[6]. Hundal R, Shaffer EA, Gallbladder cancer: epidemiology and outcomeClin Epidemiol 2014 6:99-109. [Google Scholar]
[7]. Paolucci V, Port site recurrences after laparoscopic cholecystectomyJournal of Hepato-Biliary-Pancreatic Surgery 2001 8:535-43. [Google Scholar]
[8]. Kanthan R, Senger JL, Ahmed S, Kanthan SC, Gallbladder Cancer in the 21st CenturyJournal of Oncology 2015 2015:967472 [Google Scholar]
[9]. Winston CB, Chen JW, Fong Y, Schwartz LH, Panicek DM, Recurrent gallbladder carcinoma along laparoscopic cholecystectomy port tracks: ct demonstration1Radiology 1999 212:439-44. [Google Scholar]