Laparoscopic Vesico-Psoas Boari Flap and Ureteroneocystostomy: A Case Report
JS Rajkumar1, Deepa Ganesh2, Anirudh Rajkumar3, Akbar Syed4, Kalicharan Visvanathan5
1 Chief Laparoscopic Surgeon, Department of Minimal Access Surgery, Lifeline Hospital, Chennai, Tamil Nadu, India.
2 Consultant Gynaecologist, Department of Minimal Access Surgery, Lifeline Hospital, Chennai, Tamil Nadu, India.
3 Assistant Surgeon, Department of Minimal Access Surgery, Lifeline Hospital, Chennai, Tamil Nadu, India.
4 Assistant Surgeon, Department of Minimal Access Surgery, Lifeline Hospital, Chennai, Tamil Nadu, India.
5 Medical Student, Department of Minimal Access Surgery, Lifeline Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deepa Ganesh, 47/3, New Avadi Road, Chennai-600010, Tamil Nadu, India.
E-mail: drdeepa@gmail.com
Ureteric injury, a devastating complication of laparoscopic gynaecological surgery, is often managed by endoscopic stent placement. Failure of endoscopic correction will require laparoscopic or open surgical correction to establish uretero-vesicular continuity. We here with present this case report of a Laparoscopic hysterectomy with right ureteric necrosis due to clip/cautery injury, which was managed with a totally laparoscopic ureteric reimplantation, using Boari flap, a psoas hitch, and an uretero-vesical stented anastomosis.
Hysterectomy, Psoas hitch, Re-implanatation, Ureteric injury
Case Report
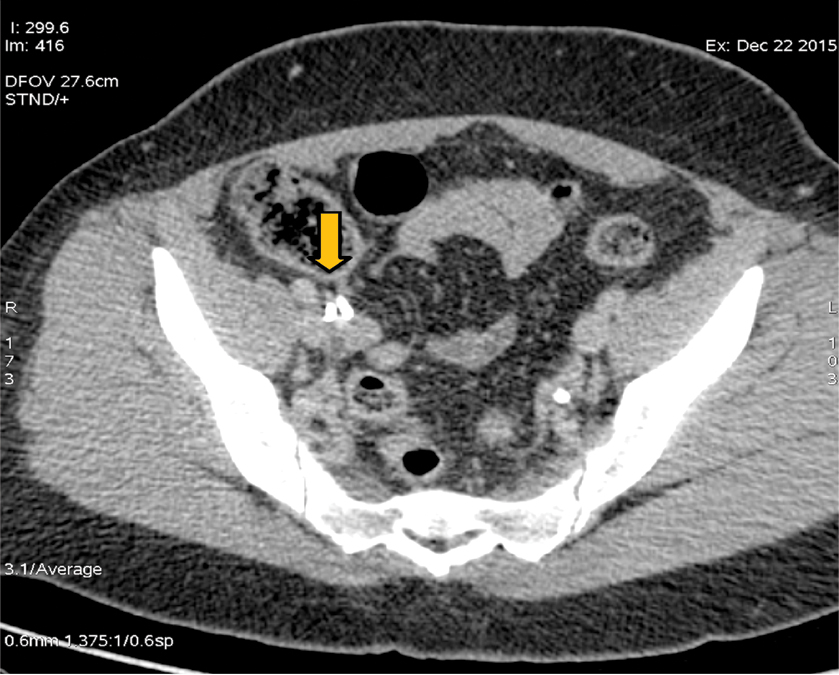
A 35-year-old woman presented with fever, rigor and right loin pain four weeks after she underwent a total laparoscopic hysterectomy for dysfunctional uterine bleeding in another institute. During the laparoscopic procedure, she was found to have brisk bleeding from both uterine arteries, necessitating a serial clipping and hemostasis of the uterine arteries. The procedure was completed laparoscopically, and after a relatively uneventful period of five days, she complained of pain in the right loin. Ultrasound showed significant right-sided hydroureteronephrosis, with the ureter being traced up to the brim of the pelvis and just beyond. Her urea and creatinine levels were normal; there was no elevation of temperature. Her blood count and specifically the white cell count were normal. The patient was relatively asymptomatic. She was followed up for a few weeks, and at the end of four weeks after surgery on Computed Tomography (CT) scan [Table/Fig-1,2] she had significantly enlarged and dilated right sided pelvicalacyeal system and a right ureter and the presence of a clip in relation to the end of the dilated ureter. Around this time, she also started having spikes of temperature and ultrasound showed a small amount of fluid in the pelvis. At this point in time, she was referred to us following an urologist’s referral. He had attempted to stent the right ureter, but the guide wire was not going up beyond 3 cm from the ureterovesical junction. Therefore patient was referred for consideration for open or laparoscopic ureteric reconstruction.
CECT – Showing the dilated right pelvic calacyeal system and right ureter with clip.
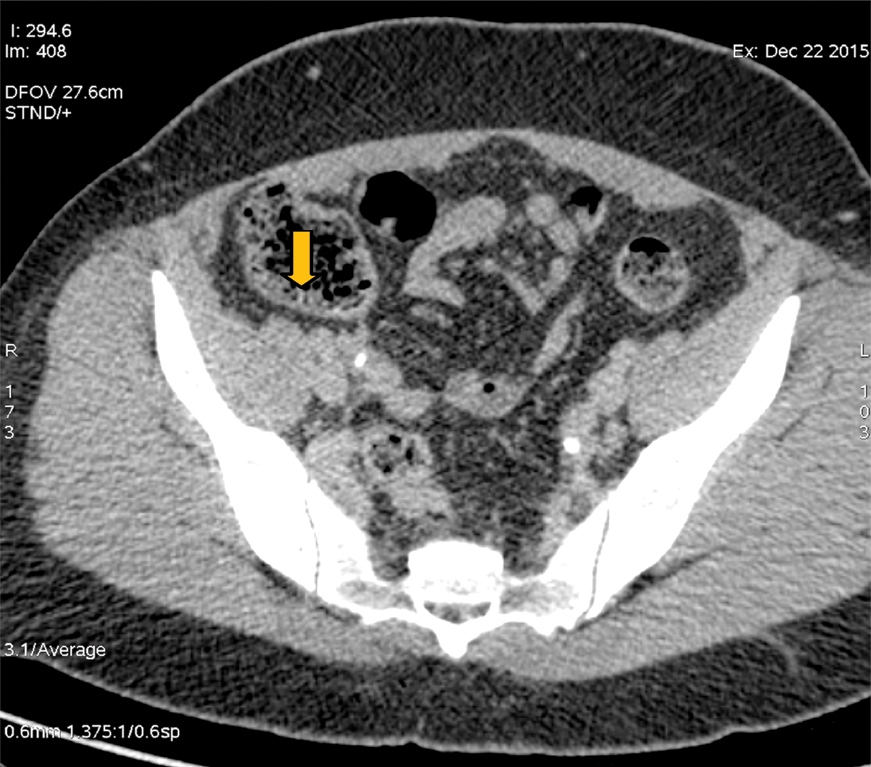
Examination revealed a non-toxic afebrile woman with no remarkable medical findings. Contrast-Enhanced Compted Tomography (CECT) confirmed an abrupt cut-off of the ureter about three to four centimeters from the Ureterovesical Junction (UVJ), with a clip at that point. On this basis, we proceeded with laparoscopic correction of the same.
Technique
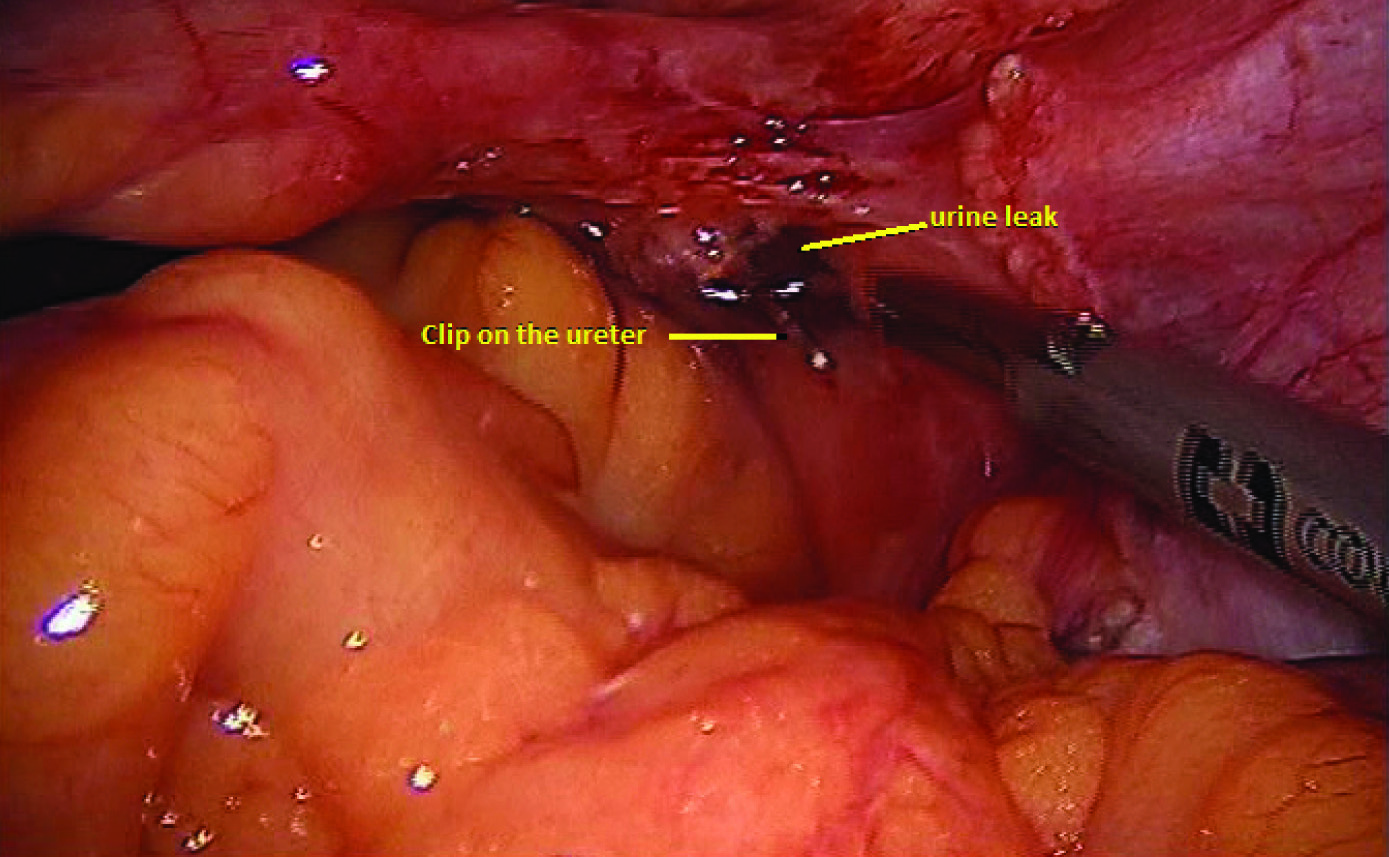
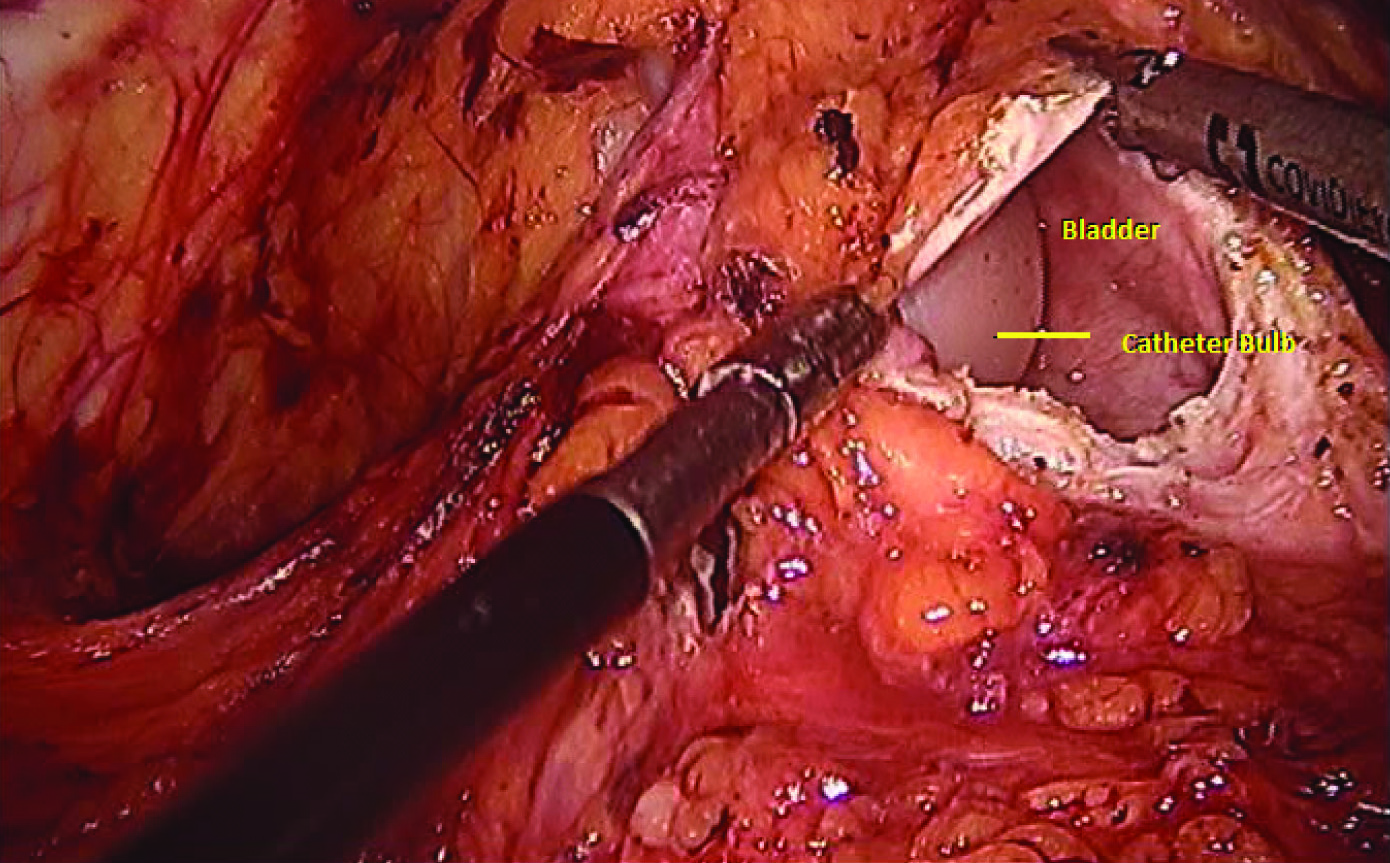
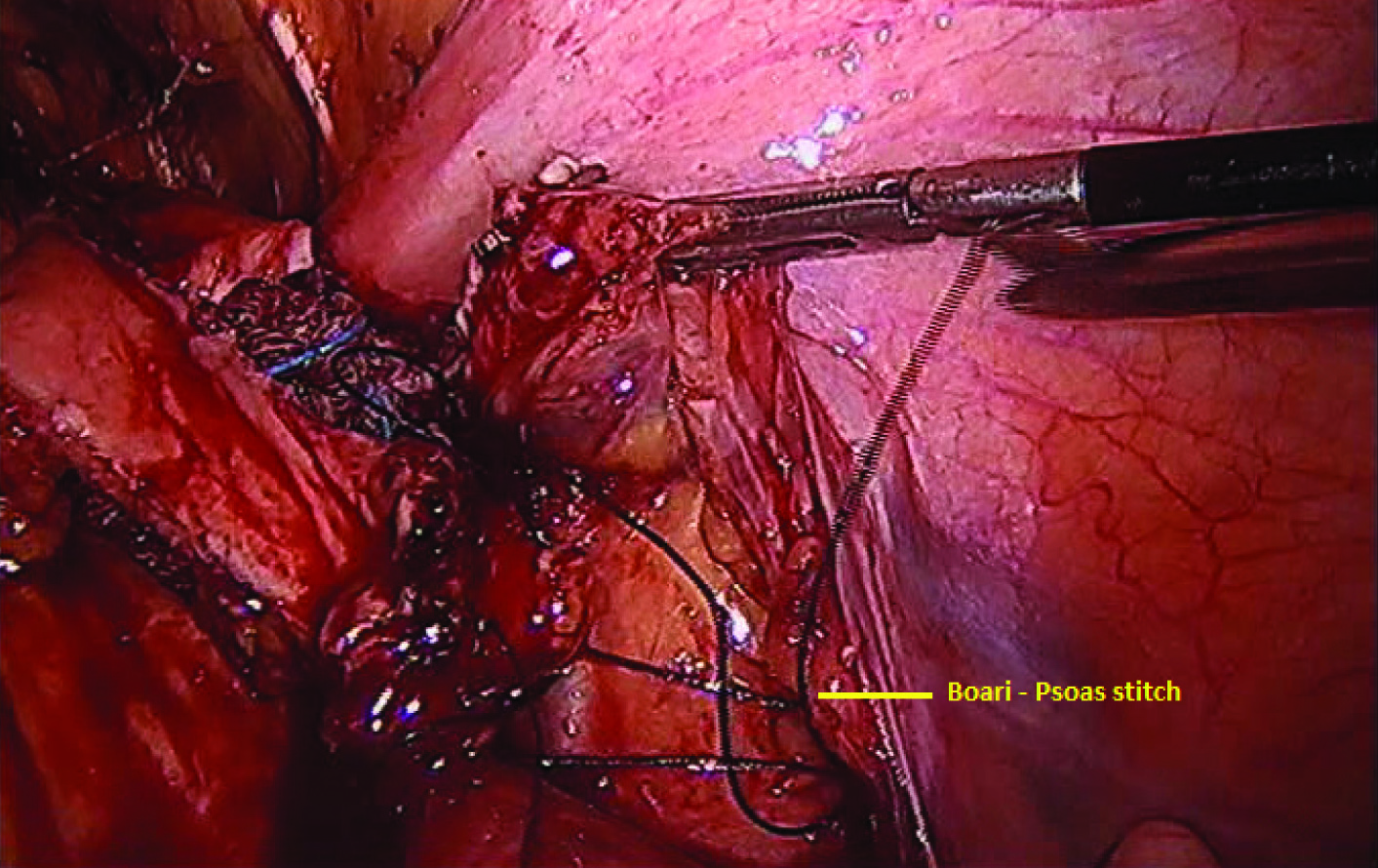
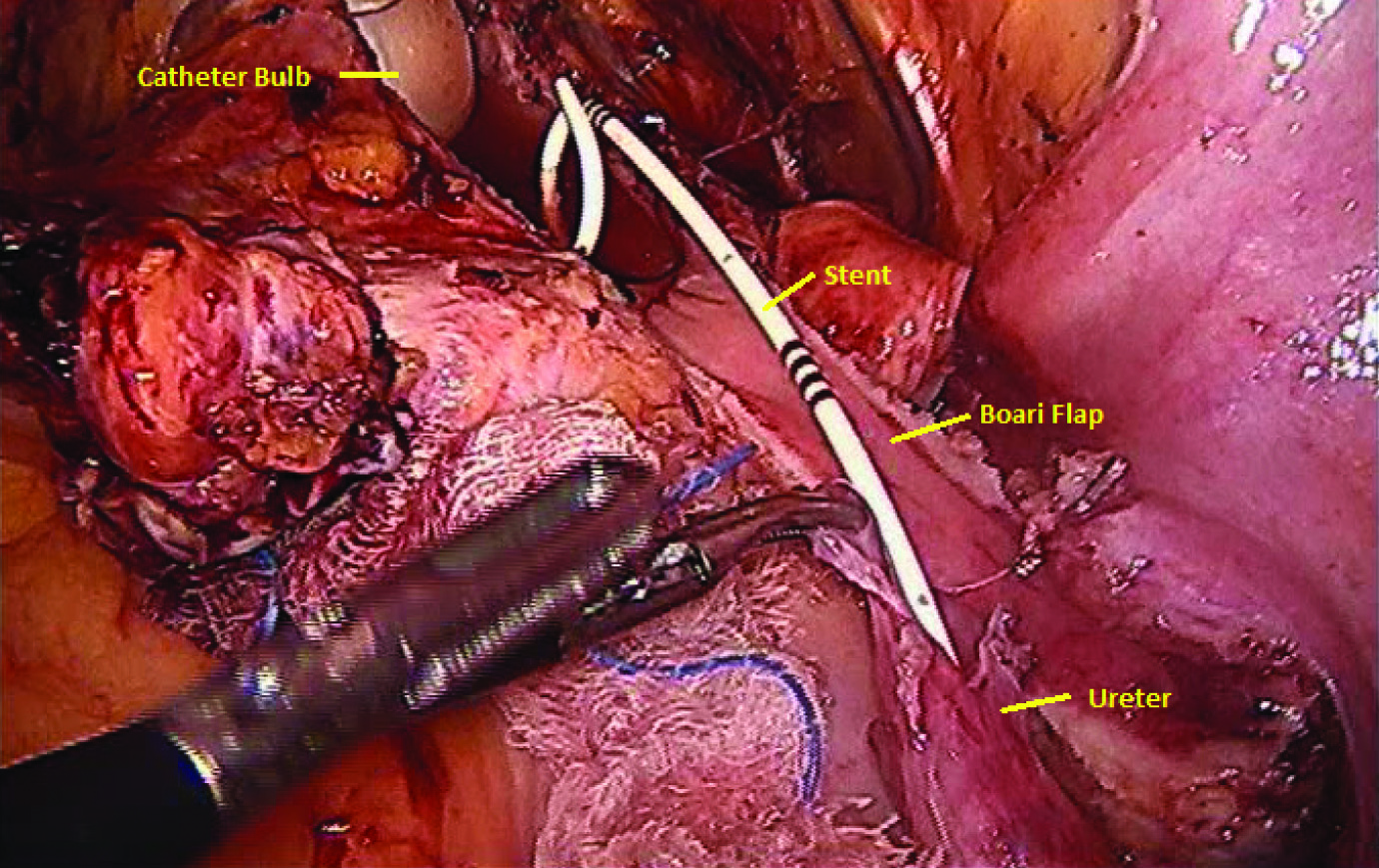
Under Endotracheal Tube General Anesthesia (ETGA), the same four ports of the hysterectomy were used. The patient was kept in a steep head-down tilt position in order to allow the small bowel to fall from the pelvic cavity. The adhesions of the omentum and small bowel to the pelvis were first lysed, and the area was exposed. This revealed a clip across the ureter about 4-5 cm from the UVJ, with a stricture and necrosed ureter with about 200-300 cc of urine in the pelvis [Table/Fig-3]. This was sucked out and the ureter was dissected free from the retroperitoneal structures. The clip was removed, the distal ureter was clipped and the proximal ureter was dissected beyond the brim of the pelvis and up till the iliac vessels, with the periureteric tissues (to avoid devascularisation of the ureter). The bladder was next exposed by opening up the peritoneum, and intraoperative distension of the bladder allowed us to get to the wall of the bladder comfortably [Table/Fig-4]. To bridge a 3-4 cm gap of necrosed and strictured ureter, we opted for the Boari flap to reduce anastomotic tension. A tongue-shaped flap (the Boari flap) was made on the fundus of the bladder, which was then flipped backwards and upwards to meet the end of the ureter. We fixed the apex of this Boari flap to the sheath of the psoas with two sutures of Polydioxanone (PDS) [Table/Fig-5]. Then the distal tip of the ureter was freshened and spatulated [Table/Fig-6]. An interrupted anastomosis using 3.0 PDS was fashioned between the spatulated ureter and the apex of the Boari flap. Then the Boari flap was closed upon itself with a continuation of the interrupted sutures of the same PDS. Using a percutaneous approach, with a Venflon cannula, a fine french stent was passed into the peritoneal cavity, and on the guide wire, a five french guide wire was passed through a Venflon cannula, percutaneously inserted suprapubically into the peritoneal cavity, and this was then inserted proximally into the open end of the ureter, halfway through the anastomosis. The stent-pusher was used and the stent was railroaded onto the guidewire, and inserted up into the kidney, and confirmed by a plain X-ray, by C-arm. Then, the distal part of the stent was pushed into the bladder [Table/Fig-7].
CECT – Showing the dilated right pelvic calacyeal system and right ureter with clip.
Titanium clip seen on the right ureter.
The psoas hitch between the boari flap and psoas sheath.
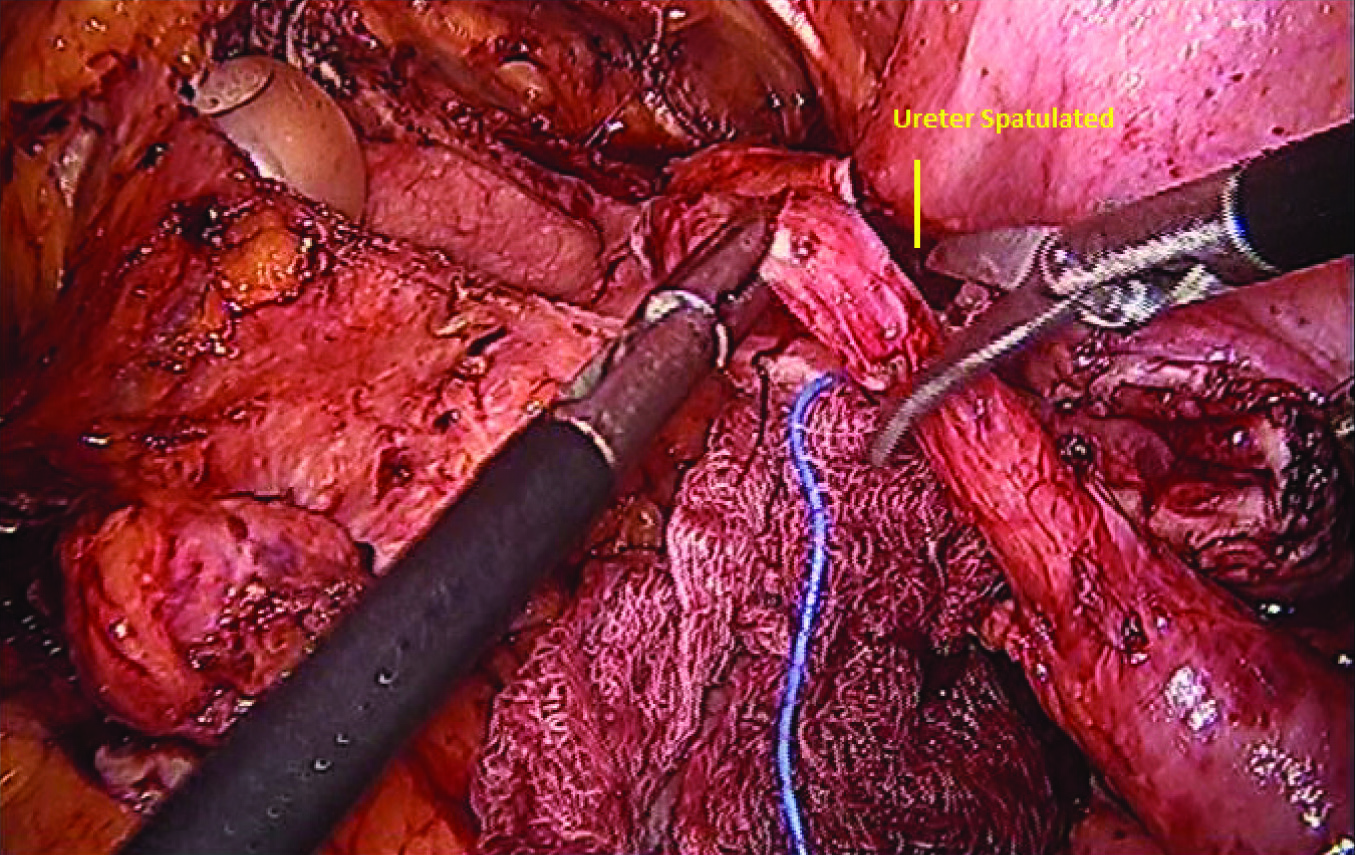
Double-J stent being placed in ureter and the bladder.
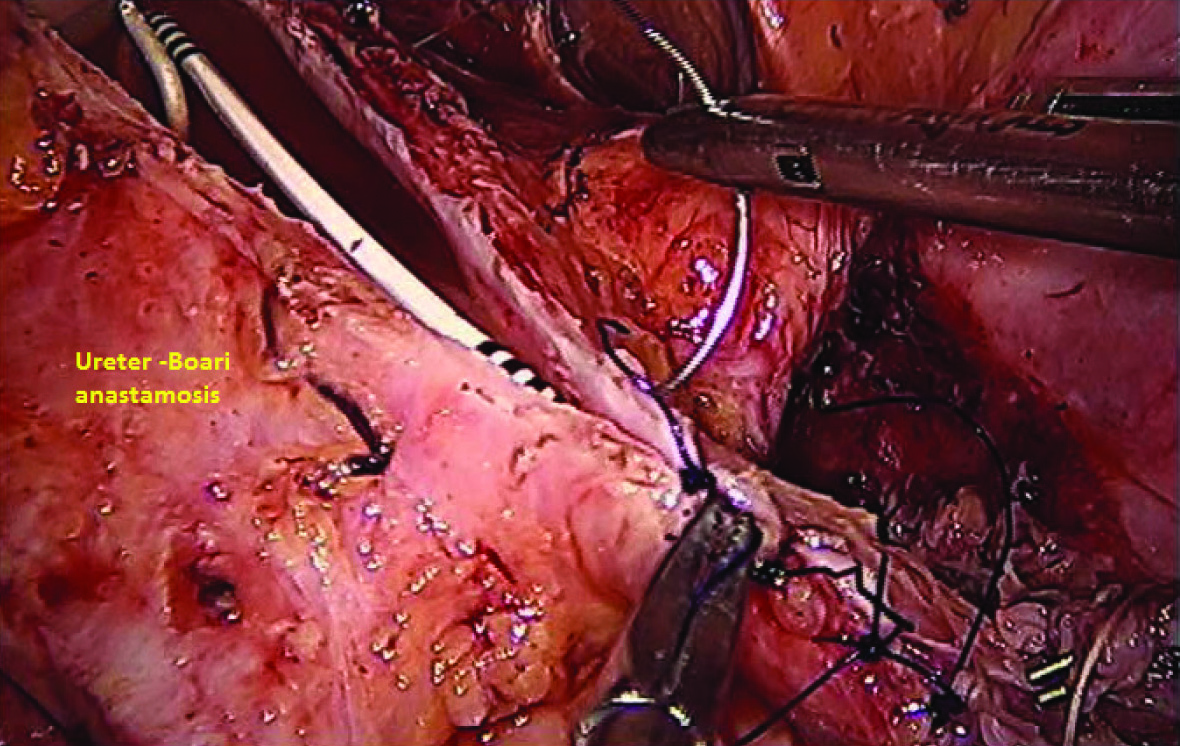
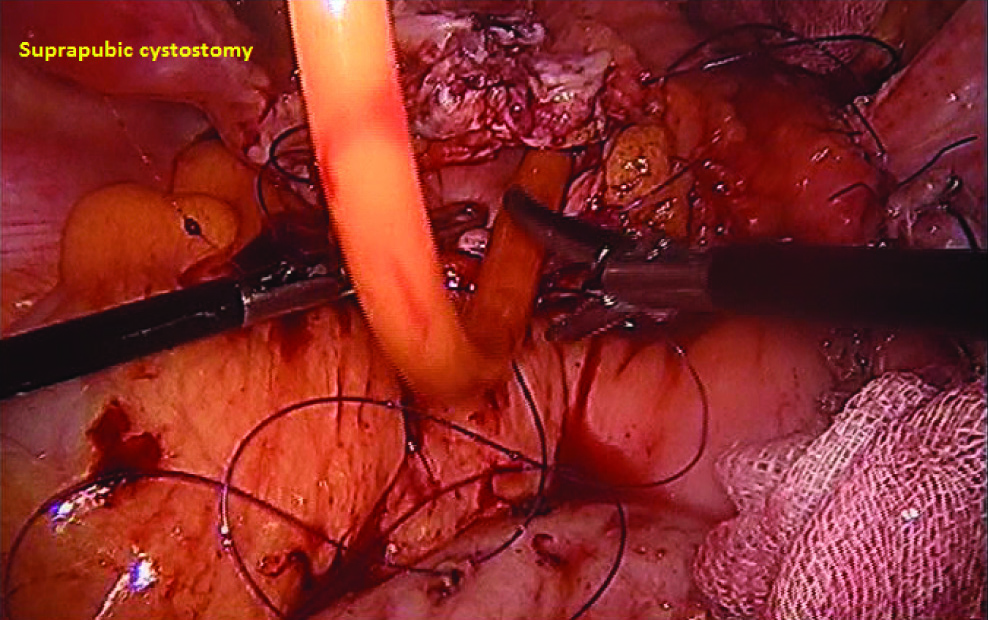
The anastomosis was completed by 3.0 PDS interrupted sutures and neocystostomy was completed [Table/Fig-8]. Then a supra-pubic cystostomy was performed directly through the suprapubic area [Table/Fig-9], and a retropubic drain was also kept.
Ureter to boari flap anastomosis.
Suprapubic cyctostomy being placed.
The patient made a smooth postoperative recovery. We checked the intravenous urogram, which showed a normal pelvicalyceal system, and a normal ureterovesical anastomosis with no leak, when the dye test was performed three weeks after surgery. At follow-up, she remains asymptomatic and comfortable.
Discussion
Gynaecological surgeries carry a risk of intraoperative ureteral damage. Immediate treatment involves drainage and urinary diversion with a combination of urethral catheter, retropubic drainage, ureteric stent or a Percutaneous Nephrostomy (PCN) to decompress the obstructed urinary system. Generally these are treated by means of laparoscopy or ureteroneocystostomy. However, when the distal ureter is of insufficient length to enable anastomoses without stress, the Boari flap technique may be resorted to in an ureteroneocystostomy.
A technically challenging procedure, it is common none the less, feasible in the hands of an experienced team of laparoscopic surgeons with adequate urological and radiological backup. The technique of ureterovesical anastomosis followed is the same as we have done in the open situation, and the reflection of the Boari flap is identical to the open approach.
In a patient, who has already faced the impact of an intraoperative technical complication, adding a major open surgery is a concern. On the other hand, minimal access surgery, with all its manifest advantages, especially when done through the same port sites as the primary operation, the hysterectomy, will alleviate the misery of a second operative procedure in the patient’s mind considerably. Most of the cases reported in literature especially from North America are of robotically anastomosed ureteroneocystostomy. The laparoscopic boari flap and ureteroneocystostomy was reported by Ramalingam M et al., (3 cases) in which technical feasibility was explored [1]. Modi P et al., published the first case report of laparoscopic boari flap with a successful outcome [2]. Two of these first four cases were secondary to ureteric injury during gynaecological surgery. Fairly comprehensive write-up on robot assisted laparoscopic boari flap, comments on technically ease using the robots increased manipulative ability. However, it is almost certain that all the nuances of the surgery are feasible with laparoscopic surgery alone, without the need for a robot assisted [1-3].
Interestingly, this patient was in extremely fine-fettle as far as her state of mind was concerned, and her return to normal activities after the second operation was quite amazing.
Although ureteric injuries can be managed endoscopically in the vast majority of cases, when there is necrosis and stricturing of the ureter (as there was in our case), endoscopic stent placement becomes impossibility. It should be reiterated that a PCN is an excellent ’bailout option’ especially in the sick patients with an obstructed system. In such a case, a primary ureteric implantation is, indeed, the Hobson’s choice of surgery. The surgical insult of ureteroneocystostomy is considerable, and if this can be brought down remarkably by the judicious use of minimal access surgery and with the right operating team, the patient’s postoperative period will be mercifully smooth as indeed was the case in our patient.
Apart from the standard intraperitoneal direct anastomosis technique that we adopted, there is an alternative. The extra vesical Lich-Gregoir technique in laparoscopic ureteral reimplantation has shown variable results [4].
The clinical feasibility and safety of this technique has been demonstrated by Ehrlich RM et al., [5], and later by Reddy PK and Evans RM [6]. At a more recent date, Lakshmanan and Fung reported no postoperative persistent reflux or obstruction in 71 laparoscopic extra vesical reimplantations, 23 of which were unilateral and 24 were bilateral [4]. Laparoscopic bladder (Boari) flap ureteroneocystostomy in a porcine model were reported by Fergany AF et al., [7].
Conclusion
Laparascopic ureteroneocystostomy is a viable alternative to open ureteral repair and anastomosis for ureteric injury during hysterectomy.
[1]. Ramalingam M, Senthil K, Ganapathy Pai M, Laparoscopic boari flap repair: report of 3 casesJ Laparoendosc Adv Surg Tech A 2008 18(2):271-75. [Google Scholar]
[2]. Modi P, Goel R, Dodia S, Case report: laparoscopic boari flapJ Endourol 2006 20(9):642-45. [Google Scholar]
[3]. Minh D, Panagiotis K, Hasan Q, Robot-assisted technique for boari flap ureteral reimplantation: is robot assistance beneficial?J Endourol 2014 28(6):679-85. [Google Scholar]
[4]. Lakshmanan Y, Fung LC, Laparoscopic extravesicular ureteral reimplantation for vesicoureteral reflux: recent technical advancesJ Endourol 2000 14(7):589-93. [Google Scholar]
[5]. Ehrlich RM, Gershman A, Fuchs G, Laparoscopic vesicoureteroplasty children: initial case reportsUrology 1994 43(2):255-61. [Google Scholar]
[6]. Reddy PK, Evans RM, Laparoscopic ureteroneocystostomyJ Urol 1994 152(6pt1):2057-59. [Google Scholar]
[7]. Fergany AF, Samee AA, Kaouk JH, Laparoscopic porcine bladder flap (Boari) ureteric reimplantationJ Urol 2001 166(5):1920-23. [Google Scholar]