Laser Assisted Excision of a Sizable Mucous Extravasation Cyst
Lohith Mandadi1, Shreya Lingamaneni2, Vinay Ram Kaipa3, Nishanth Palakurthi4
1 Postgraduate Student, Department of Periodontics, Sri Sai College of Dental Surgery, Hyderabad, Telangana, India.
2 Postgraduate Student, Department of Periodontics, Sri Sai College of Dental Surgery, Hyderabad, Telangana, India.
3 Postgraduate Student, Department of Periodontics, Mamata Dental College, Khammam, Telangana, India.
4 Assistant Professor, Department of Oral Pathology, Sri Sai College of Dental Surgery, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shreya Lingamaneni, D-601, Nagarjuna Residency, Opposite NASR Boys School Gachibowli. Hyderabad-500032, Telangana, India.
E-mail: shreya.l.88@gmail.com
Diode laser, Minor salivary gland, Mucocele, Mucous retention cyst
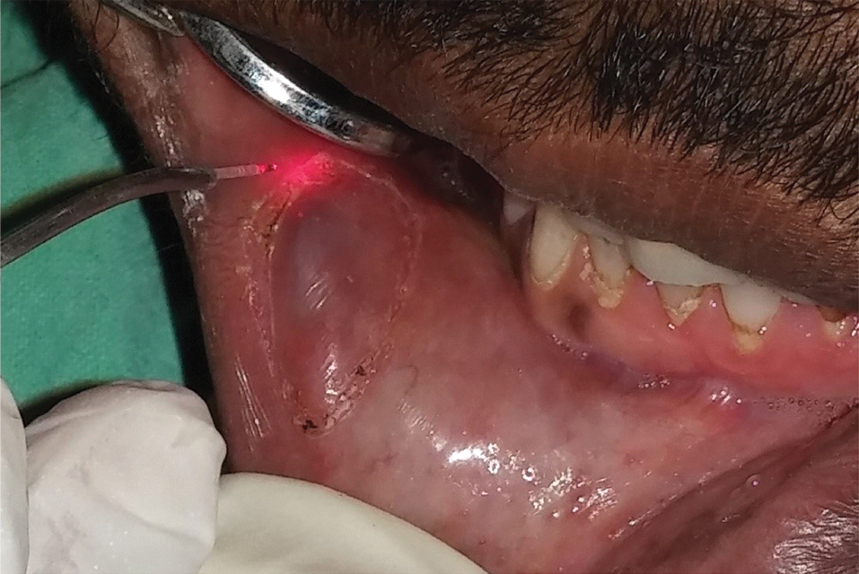
A systemically healthy 27-year-old male patient came with a chief compliant of swelling in lower right labial mucosal region opposing the canine and first premolar [Table/Fig-1]. He gave history of remission and re-occurrence of the lesion periodically for every two to three months. On clinical examination, the lesion was an ill demarcated painless swelling measuring approximately 2.5x2 cm in size with a bluish hue which on palpation is soft, fluctuant, without any fixity to underlying tissues.
Soft, fluctuant swelling with bluish hue measuring approximately 2.5x2 cm size in lower right labial mucosal region opposing the canine and first premolar.

Based on the clinical examination and patient’s history, a provisional diagnosis of mucocele was derived and after excision it was confirmed as the same with histological report. Surgical excision of the lesion with diode laser was planned. A written informed consent was taken from the patient. Laser excision (Picasso, AMD Laser Technologies, USA; wavelength of 810 nm) was done under local anaesthesia (2% lignocaine with1:80000 epinephrine), using 300 μm diameter tip at 1.3 W. Initially the boundaries of the lesion were marked using the laser. Excision was started at one end of the lesion and continued till the depth of lesion [Table/Fig-2,3,4 and 5].
Based on the visual and physical findings, the border of the lesion was demarcated with laser.
Using to-and-fro motion, the fiber tip was used in contact mode. Burrowing of the lesion was done from one end until the depth of the lesion.

Care was taken not to nick the cyst wall to prevent seepage of the mucus. Any additional tissue involving minor salivary glands was removed.
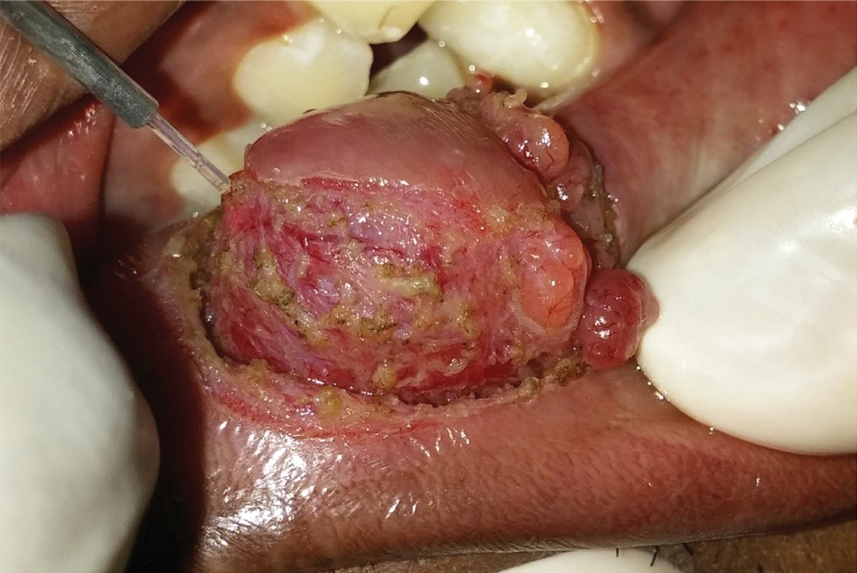
Suturing was not required. The ensuing wound was allowed to heal by secondary intention.

Smoke evacuation was done using high-speed suction. Postoperative medication included analgesics but antibiotics were not prescribed. Patient was advised to use a topical anaesthetic gel in case of discomfort and was asked not to eat spicy food for 24 hours. To establish the definitive diagnosis, the specimens fixed in 10% formalin solution were sent to the laboratory for histopathological analysis [Table/Fig-6].
Excised lesion sent for histopathological analysis.

Mucoceles are largely self-limiting with slow to rapid onset and varying sizes. They usually appear as soft, fluctuant, single or multiples bulges with colour ranging from mucosal colour to deep blue [1]. The bluish discolouration is mainly due to the vascular congestion and cyanosis of the tissue present above the fluid accumulation [2]. Apart from conventional surgical excision, cryosurgery, micro-marsupialisation, intra-lesional injections using corticosteroids, lasers have also been used. Conventional treatment includes surgical excision using two techniques, the Circumferential Incision Technique (CIT) for small cysts and the Mucosal Preservation Technique (MPT) for large sizable deep seated cysts [3,4]. Entire removal of the cyst along with the feeder gland is advocated to prevent reoccurrence.
Lasers cause less trauma, facilitate improved healing with faster recovery time when compared with other conventional methods. They are proven to be effective in treating oral soft tissue lesions. Previously several lasers including diode, KTP, CO2, Nd:YAG, Er,Cr:YSGG, Argon were used for the treatment of mucocele. Diode laser wavelengths are highly absorbed by pigmented tissues especially melanin and are deeply penetrated with rapid haemostasis. These innate properties help to precisely incise and rapidly coagulate the soft tissues [5,6]. Lasers also cause lesser wound contraction because of the fewer number of myofibroblasts formed during the healing phase.
Reasons for reoccurrence commonly include incomplete excision of the lesion, improper correction of the factors causing trauma. Care should be taken while suturing, not to damage the minor salivary glands, to prevent reoccurrence [3]. The three month postoperative follow-up showed complete healing without any wound contraction [Table/Fig-7]. No adverse effects were reported.
Three month postoperative view of the treated area. The patient was followed up for one year and the lesion did not show recurrence.

[1]. Jani DR, Chawda J, Sundaragiri SK, Parmar G, Mucocele-A study of 36 casesIndian J Dent Res 2010 21(3):337-40. [Google Scholar]
[2]. Chaitanya P, Praveen D, Reddy M, Mucocele on lower lip: A case seriesIndian Dermatol Online J 2017 8(3):205-07. [Google Scholar]
[3]. Baurmash HD, Mucoceles and RanulasJ Oral Maxillofac Surg 2003 61(3):369-37. [Google Scholar]
[4]. Kopp WK, St Hilaire H, Mucosal preservation in the treatment of mucocele with CO2 laserJ Oral Maxillofac Surg 2004 62(2):1559-61. [Google Scholar]
[5]. Coluzzi DJ, Fundamentals of dental lasers: Science and instrumentsDent Clin North Am 2004 48(4):751-70. [Google Scholar]
[6]. Ramkumar S, Ramkumar L, Malathi N, Suganya R, Excision of mucocele using diode laser in lower lipCase reports in Dentistry 2016 :01-04. [Google Scholar]