Retroperitoneal Fibromatosis Involving Iliac Vessel: A Rare Case Report
Anil Kumar1, Sanjeev Kumar2, Prashant Kumar Singh3, Subhash Kumar4, Nishant Sahay5
1 Assistant Professor, Department of General Surgery, All India Institute of Medical Sciences, Patna, Bihar, India.
2 Assistant Professor, Department of Cardiothoracic and Vascular Surgery, All India Institute of Medical Sciences, Patna, Bihar, India.
3 Assistant Professor, Department of General Surgery, All India Institute of Medical Sciences, Patna, Bihar, India.
4 Assistant Professor, Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India.
5 Assistant Professor, Department of Anaesthesia, All India Institute of Medical Sciences, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anil Kumar, Type-5, Block-B, Flat-104, AIIMS Residential Complex, Patna-801501, Bihar, India.
E-mail: dranil4@gmail.com
Retroperitoneal Fibromatosis (RPF) is extremely rare. It usually occurs after previous abdominal surgery or trauma. The diagnosis and treatment modality for RPF is a challenging issue because of its rarity and late presentation. It occurs in close relationship with vital structures like vessel, ureter and other structures in the retroperitoneal space. We report a case of RPF presenting as a mass in left iliac fossa, encasing the left common iliac vessel with symptoms of arterial occlusion in a young girl with no significant medical, surgical or trauma history. Excision with aortofemoral bypass is the best way to treat such patient.
Aortofemoral, Desmoids tumour, Polytetrafluoroethylene graft, Young girl
Case Report
A 16-year-old female presented with hard lump, mild pain in the left iliac fossa for more than two years duration. The size of swelling was increasing insidiously. She also complained of crampy pain in left lower limb especially after walking, for last two months. Lower limb pain subsided on hanging her limb slightly lower to the bed. The patient had no history of constitutional symptoms including weight loss, loss of appetite, fever, diarrhoea or vomiting. She had no history of abdominal surgery or trauma.
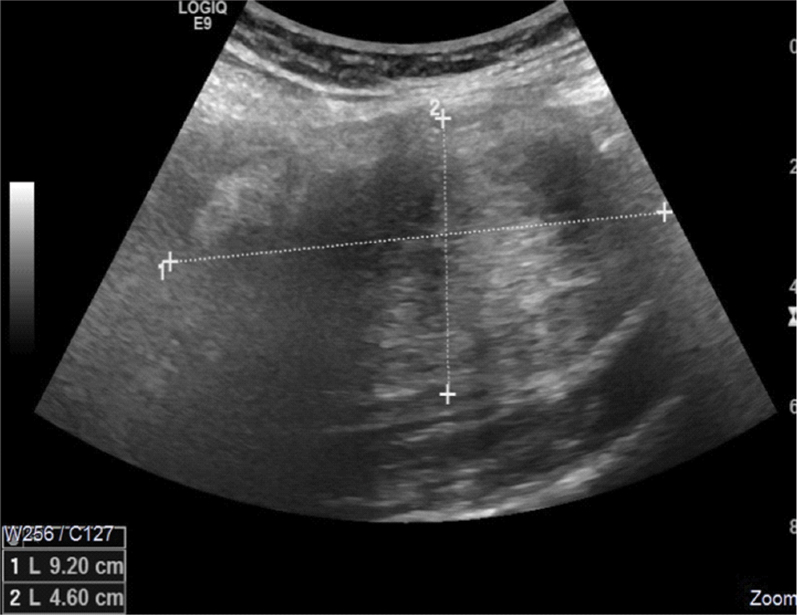
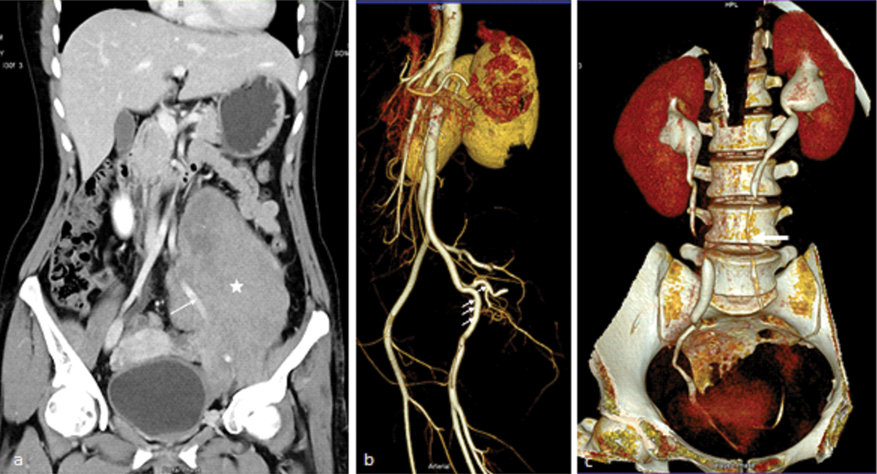
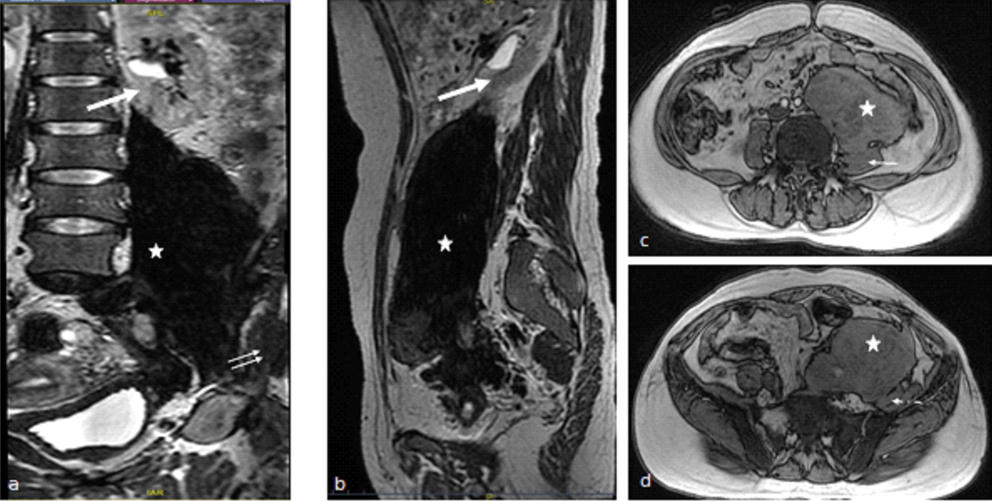
On physical examination of the left iliac fossa, a hard, firm and fixed mass of size 13x9 cm was palpable. The lump was non tender on palpation with irregular margin. All laboratory tests were within normal limits. Fine Needle Aspiration Cytology (FNAC) was done two times with non conclusive results. Sagittal B mode sonography image of left psoas region showed a heterogeneous mass with hyperechoic areas and hypoechoic areas with acoustic shadowing [Table/Fig-1]. For evaluation of this palpable mass, Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) were performed. The CT scan revealed an extensive left side retroperitoneal soft tissue mass extending between the psoas muscles, pelvic bone, vertebrae and reaching upto the left inguinal region. The mass was engulfing the left iliac vessels from its origin to inguinal ligament [Table/Fig-2a] that caused tortuosity and deviation of iliac artery [Table/Fig-2b] and pushed the left ureter towards midline with mild prominence of left pelvis as compared to right side [Table/Fig-2c]. On MRI, there was a hypointense mass involving the left psoas, extending from the level of lower kidney into the pelvis and upto the inguinal region [Table/Fig-3a,b], showing the mass to have irregular margins, significantly involving the psoas and partially involving the iliacus [Table/Fig-3c,d].
Sagittal B mode sonography image of left psoas region showing a heterogeneous mass with hyperechoic areas and hypoechoic areas with acoustic shadowing.
a) CECT abdomen study, coronal image, soft tissue window, showing a large isodense mass (star) in left abdomen and pelvis, reaching upto the inguinal region, engulfing the left iliac vessels (single arrow); b) 3D VRT, arterial phase image, showing tortuosity and deviation of the iliac arteries (multiple small arteries); however, the calibre of the arteries was normal; c) 3D VRT of delayed phase, showing medially deviated left ureter (single thick arrow), and mild prominence of left pelvis as compared to right side.
a,b) Unenhanced MRI scan images a) oblique coronal reformatted 3D T2 CUBE image (TR/TE:6000/113.6 ms) and, Sag T2 image (TR/TE: 6000:110.6 ms) showing a hypointense mass (star) involving the left psoas, extending from the level of lower kidney (thick arrow), into the pelvis and up to the inguinal region (double thin arrow); c,d) Ax LAVA (TR/TE:6.7/1.4 ms) at aortic bifurcation level, and Ax LAVA (TR/TE:6.7/1.4 ms) at upper pelvis level, showing the mass to have irregular margins, significantly involving the psoas in cross-section (single thin arrow), and partially involving the iliacus (single dashed arrow).
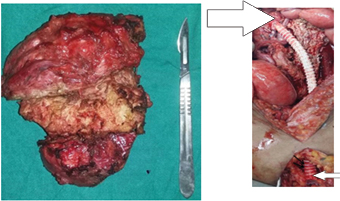
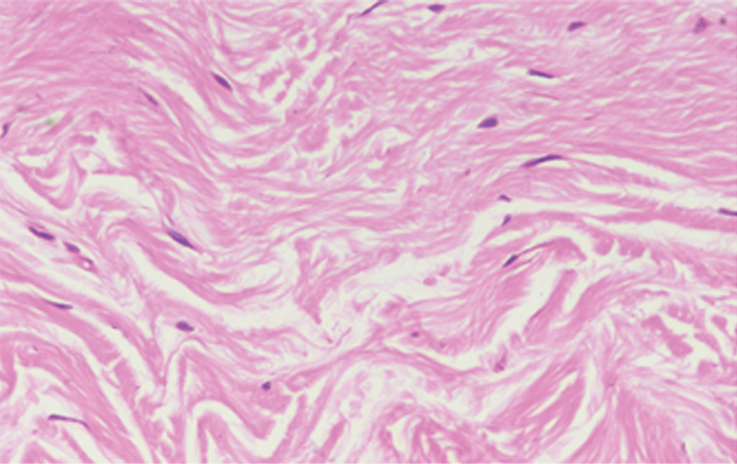
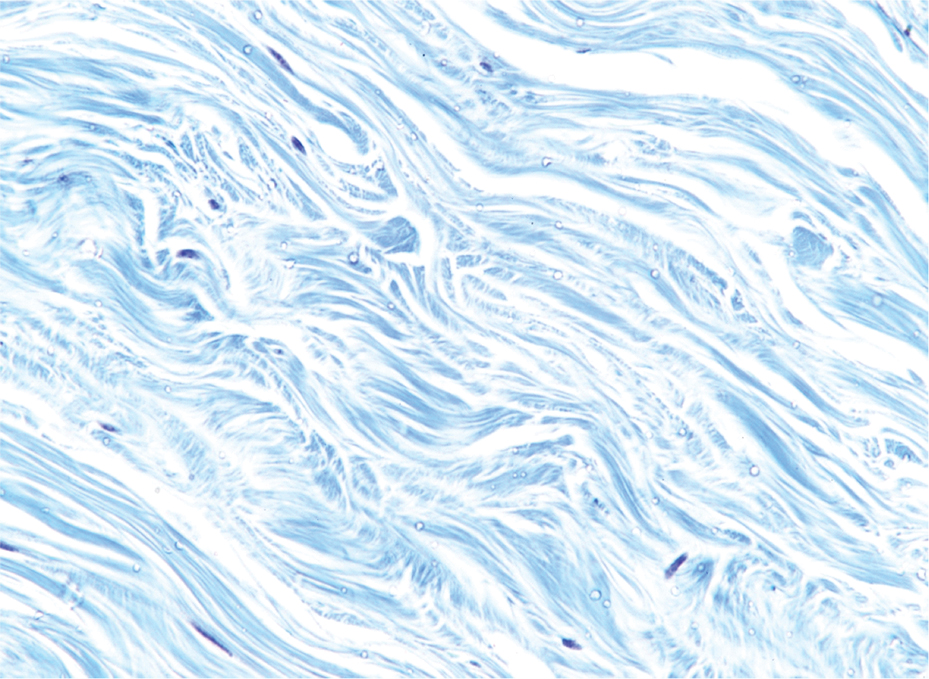
In the surgical field, the mass was hard, that encased the left common iliac vessel and approached towards left ureter, left kidney, spleen and was fixed to the left side of pelvic bone. A large retroperitoneal mass measuring (10 × 5 × 5) cm, along with left iliac vessel was removed [Table/Fig-4a]. Repair of the left common iliac artery was performed by aortofemoral bypass using Polytetrafluoroethylene (PTFE) graft [Table/Fig-4b] and all the accompanying veins were tied. Microscopically, the tumour showed cluster of spindle cells which were separated by collagenous stroma [Table/Fig-5a] and spindle shaped fibroblast with no atypia [Table/Fig-5b]. Finally, the tumour was confirmed as fibromatosis on the basis of the histopathological examination. Patient was not given any type of chemotherapy or radiotherapy because of many reasons and limitations. The patient is doing well and symptom free at eight months follow up after the operative procedure.
a) Excised tumour measuring (10x5x5) cm with left iliac vessel; b) aortofemoral bypass using PTFE graft showing side to side anastomosis at lower end of aorta (thick arrow) and at femoral vessel (thin arrow).
Showing spindle cells separated by collagenous stroma.
Special stain Masson’s Trichrome (MT Stain) show predominantly collagenous stroma with few embedded spindle cells (MT Stain, 400X).
Discussion
Fibromatosis is a benign tumour characterised by absence of cytological and clinical features of malignancy or inflammatory features. Histologically, it consists of fibroblasts with an infiltrative growth [1-3]. These tumours usually occur in females of childbearing age preferably in the third and fourth decades of life [4]. Fibromatosis or desmoids tumour may be of primary or secondary types. In the secondary type, there must be certain causes like history of trauma, drugs, surgery or hereditary diseases. The primary form (Ormond’s disease) is extremely rare [5,6]. In our case, the disease occurred in early age (16 years) without any history of surgery or injury, drugs, Familial Adenomatous Polyposis (FAP) or Gardner’s syndrome.
Fibromatosis usually occur in a an operated case from anterior abdominal wall, paravertebral musculature, retroperitoneum or pelvis [1,2]. Retroperitoneum is most commonly affected by malignant tumour. Fibromatosis are extremely rare in the retroperitoneum. In our case, left common iliac vessel was encased completely and pushed the left ureter towards the midline. Das CJ et al., also reported a similar case of RPF in the right side simulating a tumour in a young girl [7].
In the present case, patient was admitted in the surgery department because of a hard lump in left iliac fossa along with cramping pain in left lower limb after a short walk. We resected the tumour along with left common iliac artery and reconstructed it using PTFE interposition graft in order to restore blood flow to the lower limb. The iliac vein was tied at both the ends. Reconstruction of the iliac artery using PTFE graft has been reported by a number of groups [8]. PTFE or other reinforced vascular graft is commonly used for reconstruction of vessel [9].
The reported recurrence rate after resection of fibromatosis is in the range of 39-79% [2]. Radiotherapy provides a high local control rate in the postoperative setting and in unresectable tumours [10,11]. However, it was not performed in the present case. Low dose methotrexate and anthracycline containing regimen appear to be associated with a higher response rate especially in non-operable cases [12,13].
Conclusion
The RPF with iliac vessel encasement is an extremely rare and late presentation. Such cases are best evaluated by CT and MRI as FNAC may be non conclusive. Complete surgical resection with aortofemoral bypass with PTFE graft is the best option to restore the circulation for lower limb as well as to excise the tumour completely alongwith the involved vessel.
[1]. Brooks AP, Reznek RH, Nugent K, Farmer KC, Thomson JP, Phillips RK, CT appearances of desmoid tumours in familial adenomatous polyposis: further observationsClin Radiol 1994 49(9):601-07. [Google Scholar]
[2]. Ooi BS, Lee CN, Ti TK, Chachlani N, Chua ET, Retroperitoneal fibromatosis presenting as acute duodenal obstructionANZ J Surg 2001 71(1):74-76. [Google Scholar]
[3]. Casillas J, Sais GJ, Greve JL, Iparraguirre MC, Morillo G, Imaging of intra and extra abdominal desmoids tumoursRadiographics 1991 11(6):959-68. [Google Scholar]
[4]. Lopez R, Kemalyan N, Moseley HS, Dennis D, Vetto RM, Problems in diagnosis and management of desmoids tumoursAm J Surg 1990 159(5):450-53. [Google Scholar]
[5]. Maconi G, Cristaldi M, Vago L, Rovati M, Elli M, Sampietro GM, Clinical, ultrasonographic and tomographic features on the natural evolution of primary mesenteric fibromatosis: a case reportHepatogastroenterology 1998 45(23):1663-66. [Google Scholar]
[6]. Efthimiopoulos GP, Chatzifotiou D, Drogouti M, Zafiriou G, Primary asymptomatic Desmoid tumour of the mesenteryAm J Case Rep 2015 16:160-63. [Google Scholar]
[7]. Das CJ, Sharma R, Jain TP, Ravi V, Chumber S, Das AK, Unusual appearance of retroperitoneal fibromatosis simulating a tumourThe British Journal of Radiology 2006 79(946):e137-39. [Google Scholar]
[8]. Schweitzer EJ, Bartlett ST, Simultaneous PTFE reconstruction of the external iliac artery with kidney transplantationClin Transplant 1993 7(2):179-82. [Google Scholar]
[9]. Magee TR, Niblett PG, Campbell WB, Reinforced vascular grafts: a comparative studyEur J Vasc Surg 1992 6(1):21-25. [Google Scholar]
[10]. Ergen ŞA, Tiken EE, Öksüz DÇ, Dinçbaş FÖ, Dervişoğlu S, Mandel NM, The role of radiotherapy in the treatment of primary or recurrent desmoids tumours and long-term resultsBalkan Med J 2016 33(3):316-21. [Google Scholar]
[11]. Micke O, Seegenschmiedt MH, Radiation therapy for aggressive fibromatosis (desmoids tumours): Results of a national pattern of care studyInt J Radiat On Col Biol Phys 2005 61(3):882-91. [Google Scholar]
[12]. Yoon G, Kim JD, Hakchung S, The analysis of treatment of aggressive fibromatosis using oral methotrexate chemotherapyClin Orthop Surg 2014 6(4):439-42. [Google Scholar]
[13]. Garbay D, Le Cesne A, Penel N, Chevreau C, Marec-Berard P, Blay JY, Chemotherapy in patients with desmoids tumours: A study from the French sarcoma group (FSG)Ann Oncol 2012 23(1):182-86. [Google Scholar]