Massive Squamous Cell Carcinoma of the Orbit: A Rare Case Report
Smriti Nagpal Gupta1, Sushil Kumar2, Ruchi Goel3, Charu Sagar4, Okram Birbala5
1 Senior Resident, Department of Ophthalmology, Guru Nanak Eye Centre, New Delhi, India.
2 Director Professor, Department of Ophthalmology, Guru Nanak Eye Centre, New Delhi, India.
3 Professor, Department of Ophthalmology, Guru Nanak Eye Centre, New Delhi, India.
4 Junior Resident, Department of Ophthalmology, Guru Nanak Eye Centre, New Delhi, India.
5 Junior Resident, Department of Ophthalmology, Guru Nanak Eye Centre, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Smriti Nagpal Gupta, Senior Resident, Department of Ophthalmology, Guru Nanak Eye Centre, Maulana Azad Medical College, Maharaja Ranjit Singh Marg, New Delhi-110055, India.
E-mail: smriti_nagpal@hotmail.com
Squamous Cell Carcinoma (SCC) is the second most common eyelid malignancy worldwide. SCC is an aggressive tumour, with the ability to cause significant morbidity, mortality and the risk of rapid spread. Hence, urgent diagnosis and management is essential. SCC may mimic other benign and malignant lesions. Its definite diagnosis is generally done by biopsy and immunohistochemistry. Orbital invasion warrants treatment by orbital exenteration. There are chances of incomplete tumour clearance and recurrence, with a five year survival Rate of about 60%. Herein, we describe a young male patient with a massive tumour engulfing the entire orbit, and spilling over to the surface and periocular skin. There was a fungating, multilobulated mass of about 10 X 10 cm in size, with areas of necrosis and secondary infection. The tumour had invaded and destroyed all the orbital structures. However, the nasal cavity and maxillary sinus was free of tumour and there was no evidence of metastasis.
The patient underwent surgical debulking of the tumour via orbital exenteration, followed by adjuvant radiotherapy. Histopathology revealed, well differentiated SCC. On follow up, the patient was systemically well, with no evidence of metastasis and the surgical site appeared healthy.
Exenteration, Orbital SCC, Squamous cell tumour
Case Report
A 30-year-old male patient presented to our Oculoplastic clinic with complaints of a large, fungating, foul-smelling, painless mass in left orbit, progressively increasing in size for the past 8 months. There was history of blood-stained and purulent discharge from the mass. There was no history of trauma or any other swellings in the body and no history of any past surgical intervention. He was a recently diagnosed case of Hepatitis B and was on tablet entecavir 0.5 mg OD.
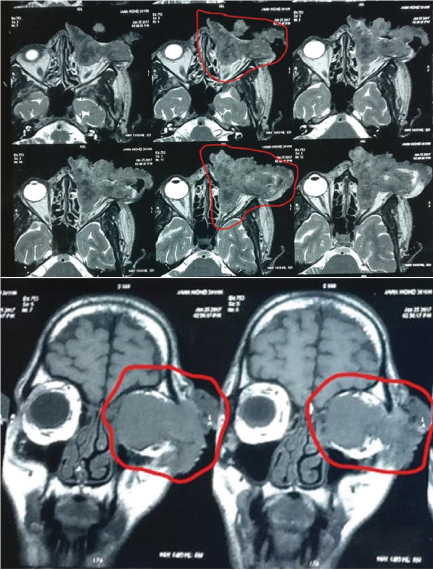
On general physical examination, the patient was anaemic. His right eye was within normal limits. On the left side, there was a fungating, multi-lobulated mass of about 10 X 10 cm in size with areas of necrosis and secondary infection [Table/Fig-1]. No orbital structure was visible separate from the tumour. The mass spilled over onto the skin of forehead, bridge of nose and left cheek. Multiple prominent feeder vessels were seen. Patient underwent clinical examination, chest X-ray, and ultrasound neck, abdomen and pelvis. There was no regional lymphadenopathy and no evidence of distant metastasis. Contrast enhanced MRI of brain and bilateral orbits were done. It revealed an infiltrating lobulated soft tissue lesion measuring approximately 85X79X75 mm occupying almost whole of left orbit involving the globe and extra-ocular muscles extending into lateral extra-orbital soft tissues [Table/Fig-2a,b]. Maxillary sinus, nasal cavity and cranial cavity were free of tumour. Systemic examination and haematological investigations were within limits with preoperative haemoglobin of 9 gm%. As per the AJCC guidelines, the patient had stage IIIC tumour (T4N0M0).
Preoperative clinical photograph.

MRI showing the large infiltrating soft tissue mass.
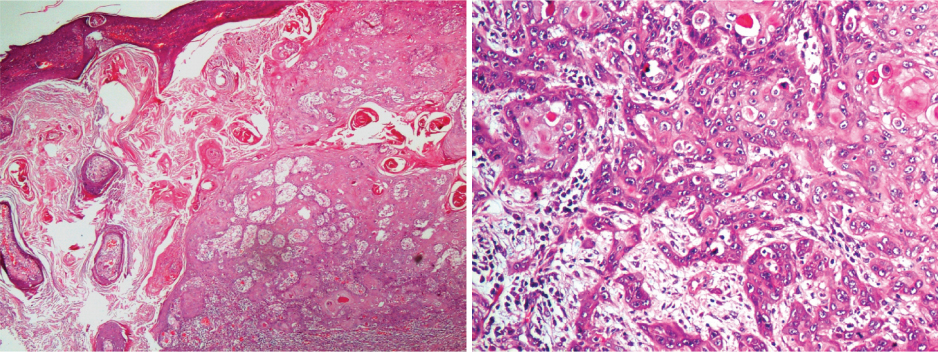
Given the large size of the lesion and the considerable morbidity caused by it, it was decided to directly go for surgical debulking via orbital exenteration under general anaesthesia, under universal precautions. Tumour clearance was incomplete, with multiple sites of bone erosion noted per-operatively, especially on the orbital roof and medial wall [Table/Fig-3]. Haemostasis was achieved and the cavity was packed with antibiotic impregnated gauze. The excised tumour tissue was sent for histopathological assessment (Paraffin preparation, Haematoxylin and eosin staining and Immunohistochemistry). Due to the large size and extensive vascularity of the lesion, there was excessive blood loss and the patient received two units packed cells and two units of fresh frozen plasma perioperatively. Postoperatively, the patient received intravenous ceftriaxone 1 gm iv BD for seven days, tablet ibuprofen 400 mg TDS for three days and tablet ethamsylate 250 mg TDS for three days. Tab entecavir was continued and the patient was on high protein diet and dietary supplements to help in recovery. Antiseptic dressing was done every three days and the wound was allowed to heal by secondary intention by granulation. Histopathology using paraffin preparation and immunohistochemistry (markers used- cytokeratin 5/6, Epithelial Membrane Antigen) revealed well differentiated squamous cell carcinoma involving all four skin margins and just 2 mm from the deep resection margin [Table/Fig-4a,b]. The patient was referred for adjuvant radiotherapy to deal with the residual tumour tissue. Radiotherapy was started three weeks after surgery.
Postoperative day 1. Multiple areas of bone necrosis are seen (arrows).

Histopathology (H&E stained slides) 4X and 20X of the tumour tissue.
At one month follow up, the patient was systemically well, his haemoglobin was 7.9 gm% and the wound appeared healthy. There was no evidence of metastasis or recurrence. The patient was advised twice weekly follow up for regular wound dressing for the initial three months, or until the socket is epithelized. Following this, follow up interval is gradually increased depending on the patient’s condition. The patient was counselled and need for life long follow up was explained.
Discussion
SCC is the second most common eyelid malignancy worldwide [1]. It is an aggressive tumour of epithelial origin. SCC is more common in males and more common in sun exposed sites, other risk factors being UV radiation, immunosuppressive drugs and certain genetic skin disorders [2,3]. Although, classically seen in 6th to 7th decade, it has been described in younger patients also. It may arise de novo, or from pre-existing pre-malignant lesions like, actinic keratosis, Bowen’s disease, keratoacanthoma etc. Albeit relatively rare in the orbit [4], it has the potential to spread rapidly, causing significant morbidity and mortality. SCC of the eyelid needs to be differentiated from benign lesions like seborrheic keratosis, nevi and squamous papilloma and from other malignancies including basal cell carcinoma and sebaceous gland carcinoma. Mixed lesions may also occur. Definitive diagnosis is usually done by histopathological examination of the biopsy sample with the use of immunohistochemical markers.
Poor prognostic factors include-advanced tumour due to delayed diagnosis and inadequate treatment, large tumour size, immunocompromised patient and poorly differentiated aggressive histological subtype [3,5]. Regional lymph node metastasis may be seen in 5-6% of cases [5]. Neuroimaging and metastatic work up should be done in all such cases to determine the complete extent of the lesion and presence of any systemic metastasis. 2-4% of eyelid tumours invade the orbit [6]. Classically, such tumours were managed by orbital exenteration. Nowadays, it is preferred to give a trial of neo-adjuvant therapies to decrease the tumour size and try and preserve the eye. In our case, the tumour was quite large and causing significant morbidity with no chance of globe preservation possible. Hence, no trial of neo-adjuvant therapy was given and surgery was the primary modality of treatment.
Goldberg RA et al., have reported incomplete tumour clearance in 38% patients of total exenteration [7]. Furthermore, Ben Simon GJ et al., have described complications like fistula formation, infection, chronically exposed bone, tissue necrosis, pain and CSF leak in upto 23.5% of their patients post exenteration [8]. In our patient also tumour clearance was incomplete with small localized sites of bone necrosis.
Post exenteration surgery, the bare area may be covered by a primary split skin graft or a musculocutaneous flap or may be left to heal by granulation [9,10]. Some authors avoid thick flaps, and advocate healing by secondary intention, since they believe these may hide early recurrences. Nowadays, techniques of microsurgical tissue transfer allow for coverage of larger defects and these may be superior in cases in which infectious or post-radiation complications are anticipated. Careful attention to hygiene and proper wound dressing is important for good healing of the orbit.
While the overall five year survival of such SCC patients is believed to be in 55-65%, it is believed to be significantly worse in patients with perineural spread [9,10]. Among patients with residual tumour, Bartley GB et al., report a one year survival of 55% and a five year survival of just 25.8% [11]. SCC patients are at a high risk of recurrence or a 3-fold greater risk of new tumours and hence, they should be on life long follow up.
Conclusion
SCC is an aggressive tumour with a potential to grow and metastasize rapidly. Hence, rapid diagnosis is of utmost importance and treatment is by complete excision with histological examination to ensure margin control. Orbital invasion by the tumour warrants treatment by orbital exenteration. Although, newer techniques of radiotherapy, chemotherapy and immunotherapy are increasingly being used to decrease tumour extent and preserve function. Exenteration still remains the only alternative for extensive tumours, to rapidly decrease the tumour mass and prevent metastasis, with adjuvant therapies for additional control. Importance of good postoperative care and regular follow up needs to be underlined.
[1]. Reifler DM, Hornblass A, Squamous cell carcinoma of the eyelidSurv Ophthalmol 1986 30:349-65. [Google Scholar]
[2]. Maclean H, Dhillon B, Ironside J, Squamous cell carcinoma of the eyelid and the acquired immunodeficiency syndromeAm J Ophthalmol 1996 121:219-21. [Google Scholar]
[3]. Donaldson MJ, Sullivan TJ, Whitehead KJ, Williamson RM, Squamous cell carcinoma of the eyelidsBr J Ophthalmol 2002 86(10):1161-65. [Google Scholar]
[4]. Gupta Y, Gahine R, Hussain N, Memon MJ, Clinico-pathological spectrum of ophthalmic lesions: an experience in Tertiary Care Hospital of Central IndiaJ Clin Diagn Res 2017 11(1):EC09-EC13. [Google Scholar]
[5]. Soysal HG, Markoç F, Invasive squamous cell carcinoma of the eyelids and periorbital regionBr J Ophthalmol 2007 91(3):325-29. [Google Scholar]
[6]. Howard GR, Nerad JA, Carter KD, Whitaker DC, Clinical characteristics associated with orbital invasion of cutaneous basal cell and squamous cell tumours of the eyelidAm J Ophthalmol 1992 113:123-33. [Google Scholar]
[7]. Goldberg RA, Kim JW, Shorr N, Orbital exenteration: results of an individualized approachOphthal Plast Reconstr Surg 2003 19(3):229-36. [Google Scholar]
[8]. Ben Simon GJ, Schwartz RM, Douglas R, Fiaschetti D, McCann JD, Goldberg RA, Orbital exenteration: one size does not fit allAm J Ophthalmol 2005 139:11-17. [Google Scholar]
[9]. Tyers AG, Orbital exenteration for invasive skin tumoursEye (Lond) 2006 20(10):1165-70. [Google Scholar]
[10]. Savage RC, Orbital exenteration and reconstruction for massive basal cell and squamous cell carcinoma of cutaneous originAnn Plast Surg 1983 10(6):458-66. [Google Scholar]
[11]. Bartley GB, Garrity JA, Waller RR, Henderson JW, Ilstrup DM, Orbital exenteration at the Mayo Clinic 1967-1986Ophthalmology 1989 96(4):468-73. [Google Scholar]