Nonfunctional Cystic Hepatic Paraganglioma Mimicking Hydatid Cyst
Preeti Balkisanji Agrawal1, Gaurav Wadhawan2, Kailashchandra Vyas3, Sashi Sujanani4
1 Associate Professor, Department of Pathology, Pacific Medical College and Hospital, Udaipur, Rajasthan, India.
2 Assistant Professor, Department of Surgery, Pacific Medical College and Hospital, Udaipur, Rajasthan, India.
3 Professor and Head, Department of Surgery, Pacific Medical College and Hospital, Udaipur, Rajasthan, India.
4 Professor and Head, Department of Pathology, Pacific Medical College and Hospital, Udaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Preeti Balkisanji Agrawal, House No. 174 A, P Road, Bhupalpura, Udaipur-313001, Rajasthan, India.
E-mail: preetibagrawal79@gmail.com
An extra-adrenal pheochromocytoma is also known as a paraganglioma. We are reporting the case of a 68-year-old female patient with an extremely rare primary nonfunctioning hepatic paraganglioma without any clinical signs and symptoms. A CECT scan of whole abdomen was done which showed a huge well defined peripherally enhancing fluid density cystic lesion measuring 14 cm × 14 cm × 12 cm with internal enhancing septations and few foci of calcification involving V to VIII segments of right lobe of liver which was compressing and displacing portal vein, its right branch, common bile duct, gall bladder. Mass was also compressing and displacing right kidney inferiorly. Laparotomy was done and sample of cyst wall sent for histopathology. After immunohistochemistry a diagnosis of paraganglioma was confirmed.
Benign, Immunohistochemistry, Liver, Pheochromocytoma
Case Report
A 68-year-old female was admitted to Pacific Medical College and Hospital in Surgery Department with complaints of dull aching pain and swelling in abdomen since two to three months. Patient was known diabetic since 12 years. She was taking Metformin 500 mg tablet twice daily. Her random blood sugar was 104.1 mg/dL and her HbA1c was 7%. On clinical examination a mass was present in right hypochondria, sized 5 cm. After investigation, her liver function tests and complete blood count were within normal limit. An ultrasound revealed a 14.6 cm × 12.9 cm cystic mass with internal echoes in right lobe liver which was speculated to be a liver abscess.
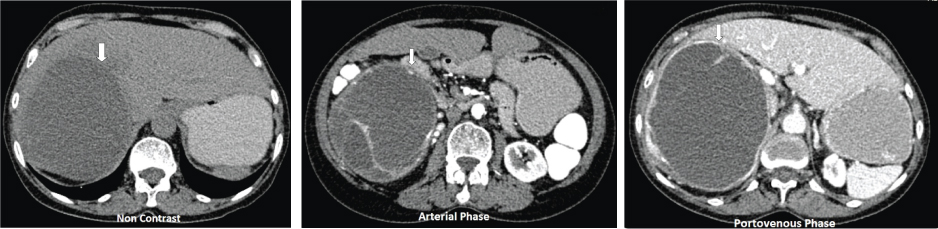
A CECT scan of whole abdomen was done which showed a huge well defined peripherally enhancing fluid density cystic lesion measuring 14 cm × 14 cm × 12 cm with internal enhancing septations and few foci of calcification involving V to VIII segments of right lobe of liver which was compressing and displacing portal vein, its right branch, common bile duct and gall bladder. Mass was also compressing and displacing right kidney inferiorly [Table/Fig-1a-c]. ELISA for Echinococcus IgG antibody was positive (Result 33 IU/mL, positive > 15 IU/mL).
a) Axial CECT scan (non contrast phase) showing cystic paraganglioma occupying whole of the right lobe of liver; b) Axial CECT scan (Arterial phase) showing cystic paraganglioma occupying whole of the right lobe of liver; c) Axial CECT scan (portovenous phase) showing cystic paraganglioma occupying whole of the right lobe of liver.
With this investigative workup a preoperative probable diagnosis of hydatid cyst of liver was established.
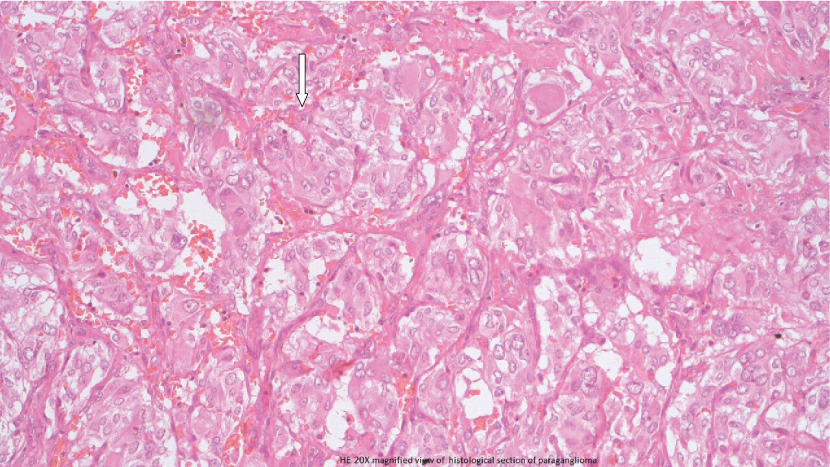
Laparotomy was done and sample of cyst wall was sent for histopathology. Two cystic walls were received in pathology department; larger measuring 6 cm × 3.5 cm × 1.5 cm and smaller measuring 2 cm × 0.5 cm. After tissue processing, Haematoxylin and Eosin stained sections showed vascular channels, surrounded by highly atypical cells with hyperchromatic and pleomorphic nuclei with prominent nucleoli at places. Extensive areas of necrosis and haemorrhage were also present.
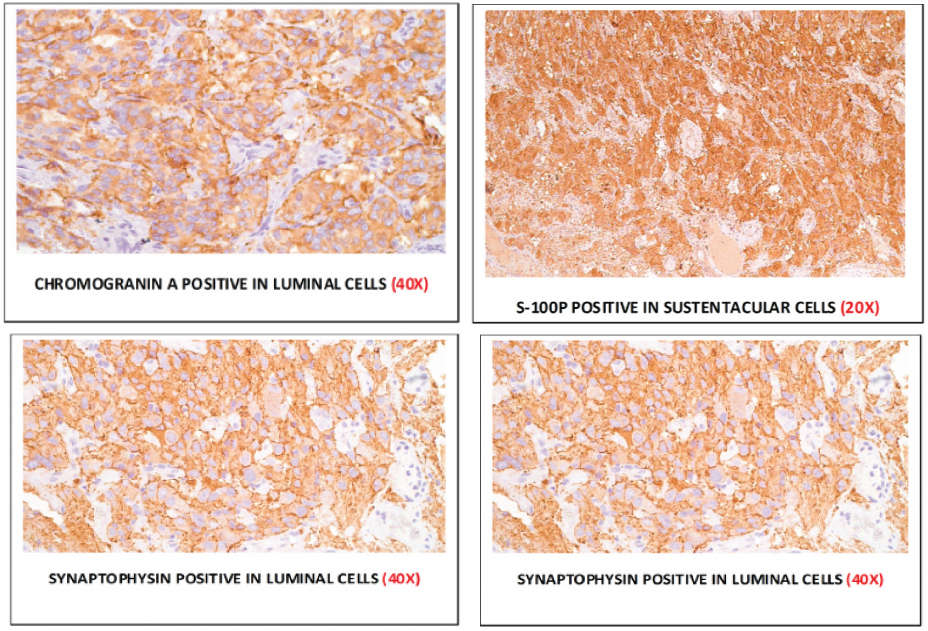
We gave a differential diagnosis of angiosarcoma and poorly differentiated hepatocellular carcinoma and sent blocks for immunohistochemistry. CD31 and CD34 were negative and Epithelial Membrane Antigen (EMA) and Alpha Fetoprotein (AFP) were negative for angiosarcoma and hepatocellular carcinoma respectively. Few of these slides showed a typical Zellballen pattern [Table/Fig-2] and having ruled out the above, IHC markers of Paraganglioma were done at higher centre. Vimentin, S100 were positive in sustentacular cells, Synaptophysin and Chromogranin were positive in luminal cells [Table/Fig-3]. Finally a diagnosis of Paraganglioma was established. After retrospective questioning surgeon told us that there were no fluctuation of blood pressure of patient on operating table and patient’s BP was 166/98 mm Hg.
Zellballen arrangement of cells characteristics of paraganglioma (H&E 40X).
Immunohistochemistry showed positivity for chromogranin (IHC 40X), S100 (IHC 20X), synaptophysin (IHC 40X), and vimentin (IHC 20X).
Patient was followed with ultrasound and Liver Function Tests (LFT’s) every three months and CT scan every year. She remained asymptomatic without any radiological evidence of recurrence at one year of follow up.
Discussion
Paragangliomas, also known as extra-adrenal pheochromocytomas, are rare neuroendocrine tumours [1]. Although paragangliomas are usually benign, at least 15%-35% of abdominal paragangliomas are malignant. Distant metastasis such as in liver, lungs, and or bones should be present to call paraganglioma as malignant. However, clinical, biochemical, and radiological features do not distinguish benign from malignant lesion [1].
Patient can present with signs and symptoms of catecholamine excess, including paroxysmal hypertension, headache, palpitation and sweating or may be completely asymptomatic [1]. Few unusual sites have been reported including the gallbladder, billiary ductal system, larynx, lung, and urinary bladder [2].
Primary hepatic site is extremely rare and very few cases have been reported to date [3-8]. To the best of our knowledge single case of periadrenal paraganglioma mimicking hydatid cyst has been reported in literature [9].
In absence of characteristic clinical symptoms of catecholamine excess and nonspecific radiological findings, hepatic paraganglioma was not considered as a possible differential diagnosis in this patient by the surgeons preoperatively. As cyst was present in liver and ELISA for Echinococcus IgG was positive, a preoperative diagnosis of hydatid cyst of liver was taken into consideration. ELISA IgG for Echinococcus have sensitivity of 94.2% and specificity of 81.6%. As sensitivity is high false positive results may occur in setting of infection with other helminths, or in patients with chronic immune disorders [10].
The current case study reported was an extremely rare case as: 1) It was primary hepatic paraganglioma; 2) It was cystic; 3) It was presented without signs and symptoms of catecholamine excess. This case indicates that though hepatic paraganglioma is rare it should be considered in differential diagnosis of any cystic mass in liver.
In our case though we followed case only for three years and so far the patient remained asymptomatic, long term follow up of paraganglioma is recommended due to potential malignant nature of this tumour and likelihood of occult primary lesions.
Conclusion
We report extremely rare case of nonfunctional cystic hepatic paraganglioma which we misdiagnosed on radiology as hydatid cyst. Though paraganglioma is rare, it should be considered in differential diagnosis of cystic hepatic mass.
[1]. You Z, Deng Y, Shrestha A, Li F, Cheng N, Primary malignant hepatic paraganglioma mimicking liver tumour: A case reportOncology letters 2015 10:1176-78. [Google Scholar]
[2]. Khan MR, Raza R, Jabbar A, Ahmed A, Primary non-functioning paraganglioma of liver: a rare tumour at an unusual locationJ Pak Med Assoc 2011 61(8):814-16. [Google Scholar]
[3]. Chang H, Xu L, Mu Q, Primary functioning hepatic paraganglioma: a case reportAdv Ther 2006 23:817-20. [Google Scholar]
[4]. Rimmelin A, Hartheiser M, Gangi A, Welsch M, Jeung MY, Jaeck D, Primary hepatic pheochromocytomaEur Radiol 1996 6:82-85. [Google Scholar]
[5]. Corti B, D’Errico A, Pierangeli F, Fiorentino M, Altimari A, Grigoni WF, Primary paraganglioma strictly confined to the liver and mimicking hepatocellular carcinomaAm J Surg Pathol 2002 26:945-49. [Google Scholar]
[6]. Reif MC, Hanto DW, Moulton JS, Alspaugh JP, Bejarano P, Primary hepatic pheochromocytoma?Am J Hypertension 1996 9:1040-43. [Google Scholar]
[7]. Kang YS, Kuhlman JE, Fishman EK, Zerhouni EA, Nonfunctional paraganglioma of the liverClin Imaging 1991 15:216-19. [Google Scholar]
[8]. Roman SA, Sosa JA, Functional paragangliomas presenting as primary liver tumoursSouth Med J 2007 100:195-96. [Google Scholar]
[9]. Tuncel A, Aslan Y, Han O, Horasanli E, Sekins S, Atan A, Laparoscopic resection of Periadrenal paraganglioma mimicking an isolated adrenal hydatid cystJSLS 2010 14:279-82. [Google Scholar]
[10]. Sadjjadi SM, Sedaghat F, Hosseini SV, Sarkari B, Serum antigen antibody detection in Echinococcosis: application in serodiagnosis of human hydatidosisKorean J Parasitol 2009 47:153-57. [Google Scholar]