Introduction
Chronic Kidney Disease (CKD) has become a major public health challenge globally. A cause for concern is the increasing burden of its risk factors, the complications of the disease, and their effects on the well-being of the increasing proportion of populations with end stage renal disease worldwide.
Aim
To determine the pattern of risk factors and the correlates of pruritus among patients with CKD.
Materials and Methods
A cross-sectional study was conducted among 124 consecutively diagnosed CKD patients at the nephrology unit of Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria, between December 2014 and May 2015. A proforma was used to collect data on study subjects’ socio-demographic and clinical parameters. Data analysis was done using International Business Machines (IBM) SPSS Version 20.0 statistical computer software package with all levels of significance set at p<0.05.
Results
The mean age of the study subjects was 46.7±14.9 years; out of 124, 103 (82.3%) were aged 21 – 60 years, and most of them were males (79.0%). The most prevalent risk factors of CKD were hypertension (47.6%), chronic glomerulonephritis (22.6%) and obstructive uropathy (13.7%). A larger proportion (54.8%) of the study subjects were haemodialysed. About one-fifth 20 (16.1%) had pruritus and the correlates of pruritus identified were sleep deprivation 55 (44.4%) and suicidal ideation 17 (13.7%).
Conclusion
Hypertension and chronic glomerulonephritis were the major risk factors of CKD identified in this study. Although only a few had pruritus, the correlates of pruritus identified were sleep deprivation and suicidal ideation. In addition to initiating or scaling up interventions, targeting the risk factors of the disease, policymakers and healthcare providers should make routine screening for pruritus and its correlates an essential component of CKD patients’ care.
Introduction
CKD has become a major health concern globally, especially in developing countries with a high burden in sub-Saharan Africa [1,2]. A peculiar feature of the epidemiology of CKD in sub-Saharan African is that it affects mainly young adults aged 20–50 years and is primarily due to hypertension and glomerular diseases, unlike in the developed countries where it presents in middle-aged and elderly patients and is predominantly due to diabetes mellitus and hypertension [3].
In sub-Saharan Africa, a cause for concern is the alarmingly high prevalence of CKD (ranging from 11% to 45.2%) reported in studies conducted among at risk populations and the fact that majority of those affected were largely unaware of the disease, as it is usually asymptomatic in its early stages [4-6].
A major challenge for both the patients presenting at advanced stages of CKD and their healthcare providers is managing the complications of the disease such as anaemia, bone metabolism abnormalities, metabolic acidosis, cardiovascular risk and skin problems, particularly pruritus [7,8].
It has been found that 50%–100% of patients with End-stage Renal Disease (ESRD) have at least one associated cutaneous change [9]. Pruritus (a medical condition characterised by moderate to severe itchy and dry skin) is the most prevalent dermatological abnormality associated with ESRD and it has been found to affect 50% to 90% of patients undergoing peritoneal dialysis or haemodialysis [10].
Several medical conditions, including insomnia, depression and suicidal ideation have been identified as correlates of pruritus, as they are not only associated with pruritus, but the risk of developing them correlates positively with its severity, particularly among patients with ESRD [11-13]. In addition to being a frequent cause of insomnia among patients with ESRD, a direct relationship has been established between pruritus and mortality among patients with ESRD and those with moderate to extreme pruritus were found to have 15%-21% higher mortality compared with those not bothered by pruritus [12].
Depression has become the most common psychological condition among patients with ESRD and they are known to have a risk of depression that is four times higher than the general population [14,15]. Data from studies showed a high prevalence of depression ranging from 21% among patients in various stages of CKD to 41.4% among renal transplant recipients, and with depression being a risk factor for non-compliance with treatment [16-18].
Of serious concern is the fact that suicidal ideation appears to be the inevitable outcome of the interplay of pruritus, insomnia and depression among patients with ESRD. However, reports from several studies identified depression as the psychiatric diagnosis most commonly associated with suicide. Whereas individuals with depression due to various causes were found to have 25 times greater risk of suicide than the general population [19], studies among ESRD patients with depression reported alarmingly higher rates of depression (ranging from 75% to 84%) than the general population [20], and noticeably, the prevalence of suicidal ideation perfectly mirrored that of depression [21].
Most of the studies in sub-Saharan Africa, and Nigeria in particular, had focused principally on the burden of CKD and its risk factors, but enough attention has not been given to determining the burden of the complications of the disease and their effects on the well-being of the increasing population of patients being managed in the various dialysis units across the continent [22-24]. This study was conducted to assess the pattern of risk factors and correlates of pruritus among patients with CKD.
Materials and Methods
This cross-sectional study was carried out among patients presenting at the Nephrology unit of Usmanu Danfodiyo University Teaching Hospital (UDUTH), located in Sokoto metropolis, Nigeria, between December 2014 and May 2015. All patients with diagnosis of CKD attending the renal clinic of the hospital and those newly referred from other departments (that were diagnosed with CKD) were considered eligible; those having other chronic diseases including cancers, chronic liver disease and congestive cardiac failure in addition to CKD were excluded. Eligible participants that consented to participate in the study were enrolled consecutively over a period of six months. CKD was defined as Glomerular Filtration Rate (GFR) less than 60 mL/minute/1.73 m2 and/or kidney damage for greater than or equal to three months [25].
A proforma was used to collect data on study subjects’ socio-demographic characteristics, their clinical and laboratory parameters (extracted from their respective case files), and presence of other symptoms such as pruritus, sleep deprivation and suicidal ideation. The serum creatinine level was used in calculating the estimated Glomerular Filtration Rate (eGFR) using the Cockcroft and Gault formula [26], which has been found to have high correlation with measured creatinine clearance in Nigerian patients with chronic kidney disease [27,28]. Staging of chronic kidney disease was done using the National Kidney Foundation’s practice guideline [25].
Institutional ethical clearance was obtained from the Ethical Committee of the University. Permission to conduct the study was obtained from the management of the hospital and the head of Nephrology Unit, informed written consent was also obtained from the study subjects before questionnaire administration.
Statistical Analysis
Data analysis was done using IBM SPSS Version 20.0 statistical computer software package. Frequency distribution tables were constructed; and cross tabulations were done to examine the relationship between categorical variables. The Chi-square test was used to compare differences between proportions. All levels of significance were set at p<0.05.
Results
Majority, 98 (79.0%) of the 124 study subjects were males, and most of them 102 (82.3%) were married. Their ages ranged from 16 to 80 years (mean=46.70±14.92), but majority 102 (82.3%) were aged 21 to 60 years. Although, about half 63 (50.8%) of the 124 study subjects had no formal education, only about a fifth 28 (22.6%) were unemployed [Table/Fig-1].
Socio-demographic profile of study subjects.
| Variables | Frequency (%) n = 124 |
|---|
| Age groups (in years) |
| 20 and below | 7 (5.6) |
| 21-40 | 43 (34.7) |
| 41-60 | 59 (47.6) |
| 61 and above | 15 (12.1) |
| Sex |
| Male | 98 (79.0) |
| Female | 26 (21.0) |
| Marital status |
| Single | 15 (12.1) |
| Married | 102 (82.3) |
| Separated | 2 (1.6) |
| Divorced | 4 (3.2) |
| Widowed | 1 (0.8) |
| Education status |
| None | 8 (6.4) |
| Quranic only | 55 (44.4) |
| Primary | 12 (9.7) |
| Secondary | 33 (26.6) |
| Tertiary | 16 (12.9) |
| Occupation |
| Unemployed | 28 (22.6) |
| Artisan | 16 (12.9) |
| Trading/Business | 31 (25.0) |
| Civil servant | 28 (22.6) |
| Farming | 21 (16.9) |
Prevalence of Risk Factors of CKD among the Study Subjects
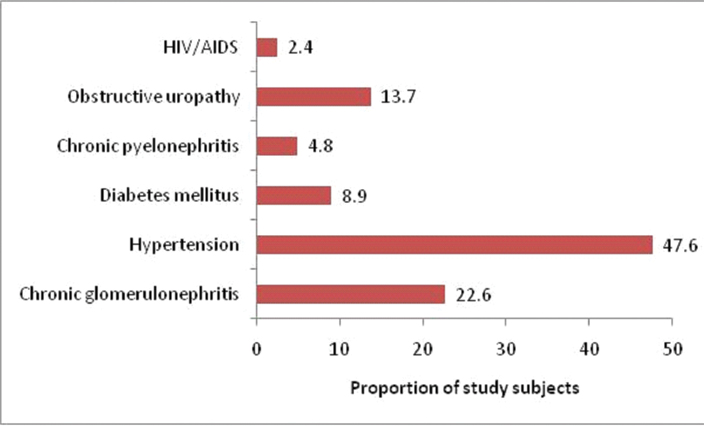
About half, 59 (47.6%) of the 124 study subjects had hypertension. Other prevalent risk factors included chronic glomerulonephritis 28 (22.6%) and obstructive uropathy 17 (13.7%); only a few had diabetes mellitus 11 (8.9%), chronic pyelonephritis 6 (4.8%), and HIV/AIDS 3 (2.4%) as shown in [Table/Fig-2].
Prevalence of risk factors of CKD among the study subjects.
Stage of CKD and Type of Treatment Received by Study Subjects
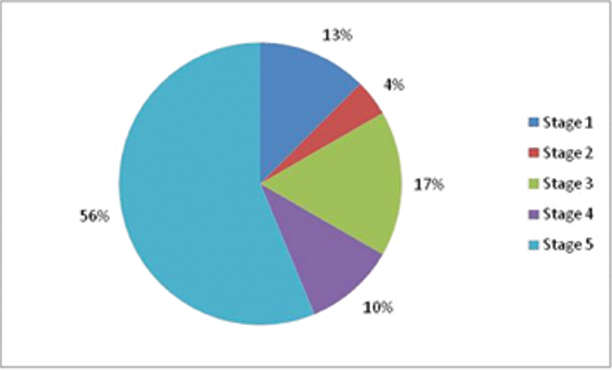
About two-thirds 83 (66.9%) of the 124 study subjects were at advanced stages {i.e., severe CKD (stage 4) and kidney failure (stage 5)} of CKD [Table/Fig-3]. Majority, 68 (54.8%) of the study subjects were haemodialysed (most commonly two to three sessions per week), whereas the remaining 56 (45.2%) were managed conservatively.
Stage of CKD among the study subjects.
Prevalence of Pruritus and its Correlates among the Study Subjects
About one-fifth 20 (16.1%) of the 124 study subjects had pruritus, 55 (44.4%) had sleep deprivation, and 17 (13.7%) had experienced suicidal ideation [Table/Fig-4].
Prevalence of pruritus and its correlates among the study subjects.
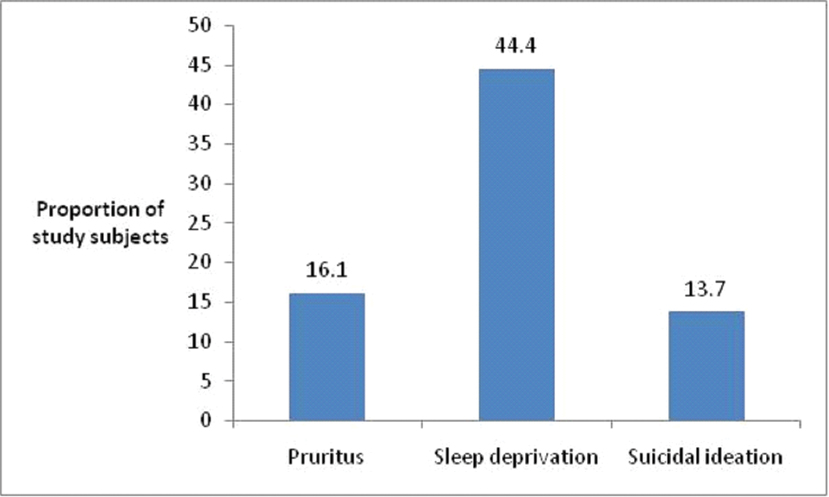
Whereas there was no association between presence of pruritus and any of the socio-demographic variables of the study subjects (p>0.05), pruritus was significantly more prevalent (p=0.008) among the study subjects on haemodialysis (25.0%) compared to those on conservative management (5.4%).
Similarly, there was no association between presence of pruritus and experience of suicidal ideation (p=0.595), pruritus was significantly more prevalent (p<0.001) among study subjects with sleep deprivation (30.9%) compared to those without (4.3%) as shown in [Table/Fig-5].
Distribution of pruritus by socio-demographic profile, type of treatment and its correlates among the study subjects.
| Presence of Pruritus (n=124) |
|---|
| Variables | Yes Frequency (%) | No Frequency (%) | Test of Significance |
|---|
| Age group (in years) |
| 20 and below | 1 (14.3) | 6 (85.7) | χ2=0.364 |
| 21 - 40 | 6 (14.0) | 37 (86.0) |
| 41 - 60 | 10 (16.9) | 49 (83.1) | p=0.948 |
| 61 and above | 3 (20.0) | 12 (80.0) |
| Sex |
| Male | 16 (16.3) | 82 (83.7) | χ2=0.013 |
| Female | 4 (15.4) | 22 (84.6) | p=0.908 |
| Marital status |
| Single | 2 (13.3) | 13 (86.7) | χ2=0.126 |
| Married | 17 (16.7) | 85 (83.3) | p=0.939 |
| Separate/Widowed/Divorced | 1 (14.3) | 6 (85.7) | |
| Education status |
| Informal (None/Quranic) | 9 (14.3) | 54 (85.7) | χ2=0.322 |
| Formal (Primary and above) | 11 (18.0) | 50 (82.0) | p=0.571 |
| Occupation |
| Unemployed | 5 (17.9) | 23 (82.1) | χ2=0.080 |
| Employed | 15 (15.6) | 81 (84.4) | p=0.778 |
| Type of treatment |
| Haemodialysis | 17 (25.0) | 51 (75.0) | χ2=6.961 |
| Conservative | 3 (5.4) | 53 (94.6) | p=0.008 |
| Sleep deprivation |
| Present | 17 (30.9)* | 38 (69.1) | χ2=15.961 |
| Absent | 3 (4.3) | 66 (95.7) | p<0.001 |
| Suicidal tendency |
| Present | 2 (11.8) | 15 (88.2) | χ2=0.277 |
| Absent | 18 (16.8) | 89 (83.2) | p=0.595 |
*Statistically significant
Statistical test: Chi-square test
Discussion
Hypertension was the most prevalent risk factor among the study subjects in this study (47.6%), followed by chronic glomerulonephritis (22.6%) and obstructive uropathy (13.7%); and only a few had diabetes mellitus (8.9%). The high prevalence of hypertension and relatively low prevalence of diabetes mellitus among the study subjects perfectly mirror their prevalence in the Nigerian population. In 2008, the prevalence of hypertension in Nigeria was estimated at 42.8%, while that of diabetes mellitus was estimated at 8.5% [29]. A cause for concern is the dual relationship between hypertension and CKD; as hypertension is both a cause and a complication of CKD, and it is also a well-established risk factor for CKD progression [30].
The identification of chronic glomerulonephritis as the second most common risk factor for CKD in this study is consistent with the earlier submission by Barsoum RS and Francis MR on chronic glomerulonephritis and interstitial nephritis being the principal causes of CKD in the developing countries [31], thus reflecting the high prevalence of bacterial, viral and parasitic infections that affect the kidney. The high prevalence of these infectious diseases in the young population in sub-Saharan Africa may therefore be the reason while CKD affects predominantly the young population in the continent. This is further supported by the finding in a recent study from Khartoum State, Sudan [32] that reported glomerulonephritis followed by hypertension as the leading causes of ESRD in patients aged less than 40 years, while hypertension and diabetes mellitus were the leading causes among patients over 40-year-old.
A notable feature of the epidemiology of CKD is the emergence of three disease conditions as the major risk factors for the disease across the globe. Whereas, studies across sub-Saharan Africa, South America, and Australia majorly reported hypertension (closely followed by either glomerulonephritis or diabetes mellitus) as the most prevalent risk factor of CKD, similar to the finding in this study [33-35], studies in Asia majorly reported chronic glomerulonephritis [36,37], while studies in North America and Europe majorly reported diabetes mellitus (closely followed by either hypertension or glomerulonephritis) as the most prevalent risk factors for the disease [38,39]. Prevention and control of CKD in sub-Saharan Africa is therefore contingent on tackling hypertension, diabetes mellitus and chronic glomerulonephritis; and for this to make any meaningful impact, it is necessary to scale up control of bacterial, viral and parasitic diseases that have been identified as major risk factors of CKD across the continent [3-6].
The prevalence of pruritus in this study (16.1%) is lower than the 48% reported in a study among patients on maintenance dialysis in Benin City, Nigeria [40] (which had a smaller sample size compared to this study). However, the significantly higher prevalence of pruritus among patients on haemodialysis (25%) compared to those managed conservatively (5.4%), is almost at par with the 26.7% prevalence obtained in a study among patients with chronic renal failure in Nigeria [41]. While these findings are consistent with those reported in studies elsewhere, they bring to the fore the high burden of pruritus among patients with ESRD across Nigeria, and the need to accord its treatment top priority in the care of these patients [7-10]. This is imperative in view of the increasing prevalence of CKD in Nigeria and the devastating effects of pruritus on patients’ quality of sleep, well-being and survival [42,43].
The relatively low prevalence of suicide ideation in this study (13.7%) compared to the findings in studies conducted in other places [21,44], also reflects its low prevalence compared to sleep deprivation (44.4%) in this study. This could be related to both the long standing cultural values and beliefs that resist suicidal behavior as a problem solving alternative among Africans [45] and the prevalent social support often extended to individuals with social and health problems in the African culture. Social support from families provides patients with practical help and buffers the stresses of living with illness. Evidence from studies suggests that higher levels of social support are associated with better treatment adherence, improved clinical outcomes, reduced symptomatology and the adaptation of beneficial lifestyle activities [46,47].
On the other hand, the relatively low prevalence of self-reported suicidal ideation in this study could also be due to under reporting in view of the fact that while several countries and jurisdictions across the globe have repealed their legal statutes criminalising suicide attempts, it remains a crime in several African countries including Nigeria [48]. Whereas, other studies [11-13] had also established an association between pruritus and sleep deprivation as obtained in this study, an association was also established between pruritus and mortality in those studies, in contrast to the absence of association between pruritus and suicidal ideation in this study. However, this could be due to the very low self-reported prevalence of suicidal ideation by the study subjects. Even though a relatively low prevalence of suicidal ideation was obtained in this study, the high burden of pruritus and sleep deprivation obtained suggest the need for policymakers and healthcare providers to make routine screening for pruritus and its correlates an essential component of CKD patients’ care.
Limitation
The main limitation in this study was deliberate misinformation by the study subjects, particularly regarding suicidal ideation, in view of the criminalisation of suicide in several African countries including Nigeria, and its stigmatisation worldwide. These could serve as potent disincentives to disclosure of suicidal ideation among patients that have experienced it.
Conclusion
Hypertension and chronic glomerulonephritis were the major risk factors of CKD identified in this study. Although, only a few of the CKD patients had pruritus, a substantial proportion of them suffer from its correlates including sleep deprivation and suicidal ideation. Routine screening for pruritus and its correlates should be made an essential component of CKD patients’ care, in addition to initiating or scaling up interventions targeting the risk factors of the disease.
[1]. Naicker S, End-stage renal disease in sub-Saharan AfricaEthn Dis 2009 19:S1-13. [Google Scholar]
[2]. Alebiosu CO, Ayodele OE, The global burden of chronic kidney disease and the way forwardEthn Dis 2005 15(3):418-23. [Google Scholar]
[3]. Arogundade FA, Barsoum RS, Chronic kidney disease prevention in sub-Saharan Africa; a call for governmental, non-governmental and community supportAm J Kidney Dis 2008 51:515-23. [Google Scholar]
[4]. Sumaili EK, Cohen EP, Zinga CV, Krzesinski JM, Pakasa NM, Nseka NM, High prevalence of undiagnosed chronic kidney disease among at-risk population in Kinshasa, the Democratic Republic of CongoBMC Nephrology 2009 10:18 [Google Scholar]
[5]. Afolabi MO, Abioye-Kuteyi EA, Arogundade FA, Bello IS, Prevalence of chronic kidney disease in a Nigerian family practice populationSA Fam Pract 2009 51:132-37. [Google Scholar]
[6]. Kaze FF, Halle MP, Mopa HT, Ashuntang G, Fouda H, Ngogang J, Prevalence and risk factors of chronic kidney disease in urban adult Cameroonians according to three common estimators of glomerular filteration rate: a cross-sectional studyBMC Nephrology 2015 16:96 [Google Scholar]
[7]. Okparavero A, Foster MC, Tighiouuart H, Gudnasin V, Indridason O, Gudmumdsdottir H, Prevalence and complications of chronic kidney disease in a representative elderly population in IcelandNephrol Dial Transplant 2016 31(3):439-47. [Google Scholar]
[8]. Akhyani M, Ganji M, Samadi N, Khamesan B, Daneshpazhooh M, Pruritus in haemodialysis patientsBMC Dermatology 2005 5:07 [Google Scholar]
[9]. Sanad EM, Sorour NE, Saudi WM, Elmastry AM, Prevalence of cutaneous manifestations in chronic renal failure patients on regular haemodialysis: a hospital based studyEgypt J Dermatol Venerol 2014 34:27-35. [Google Scholar]
[10]. Narita I, Iquchi S, Omori K, Geiyo F, Uremic pruritus in chronic haemodialysis patientsJ Nephrol 2008 21(2):161-65. [Google Scholar]
[11]. Zucker I, Yosipovivitch G, David M, Gafter U, Buner G, Prevalence and characteristics of uremic pruritus in patients undergoing haemodialysis: uremic pruritus is still a major problem for patients with end-stage renal diseaseJ Am Acad Dermatol 2003 49:842-46. [Google Scholar]
[12]. Pisoni RL, Wikstrom P, Elder SJ, Akizawa T, Asano Y, Keen ML, Pruritus in haemodialysis patients: international results from the Dialysis Outcome and Practice Pattern Study (DOPPS)Nephrol Dial Transplant 2006 21:3495-505. [Google Scholar]
[13]. Wikstrom B, Itchy skin- a clinical problem of haemodialysis patientsNephrol Dial Transplant 2007 22(Suppl 5):v3-v7. [Google Scholar]
[14]. Kimmel PL, Depression in patients with chronic renal disease: what we know and what we need to knowJ Psychosomatic Research 2002 53(4):951-56. [Google Scholar]
[15]. Hedayati SS, Bosworth HB, Briley LP, Sloane RJ, Pieper CF, Kimmel PL, Death or hospitalization of patients on chronic dialysis is associated with a physician based diagnosis of depressionKidney Int 2008 74(7):930-36. [Google Scholar]
[16]. Hedeyati SS, Minhajuddin AT, Afshar M, Toto RD, Trivedi MH, Rush AJ, Association between major depressive episodes in patient with chronic kidney disease, and initiation of dialysis, hospitalization, or deathJAMA 2010 303:1946-53. [Google Scholar]
[17]. Tsunoda T, Yamashita R, Kojima Y, Takahara S, Risk factors for depression after kidney transplantationTransplant Proc 2009 42:1679-81. [Google Scholar]
[18]. Dimatteo MR, Lepper HS, Croghan TW, Depression is a risk factor for non-compliance with medical treatmentArch Intern Med 2000 160:2101-07. [Google Scholar]
[19]. American Society of Suicidology. Depression and suicide risks. Available at: https://www.suicidology.org/portals/14/docs/resources/factsheets/2011/ [Google Scholar]
[20]. Kurella M, Kimmel PL, Young BS, Chertow GM, Suicide in the United States End-stage Renal Disease programJASN 2005 16(3):774-81. [Google Scholar]
[21]. Chen CK, Tsai YC, Hsu HJ, Wu IW, Sun CY, Chou CC, Depression and suicide risk in haemodialysis patients with chronic renal failurePsychosomatics 2010 51(6):5288 [Google Scholar]
[22]. Odubanjo MO, Oluwasola AO, Kadiri S, The epidemiology of end-stage renal disease in Nigeria: the way forwardInt Urol Nephrol 2011 43(3):785-92. [Google Scholar]
[23]. Pakasa S, Sumaili E, The nephrotic syndrome in the Democratic Republic of CongoN Engl J Med 2006 354:1085-86. [Google Scholar]
[24]. Gerntholtz TE, Goetsch SJW, Katz I, HIV-related nephropathy: a South African perspectiveKidney Int 2006 69:1885-91. [Google Scholar]
[25]. National Kidney Foundation. KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. NKF 2002. National Kidney Foundation Inc 2002. Available at: https://www2.kidney.org/professionals/KDOQI/guidelines.ckd/ [Google Scholar]
[26]. Cockcroft DW, Gault MH, Prediction of creatinine clearance from serum creatinineNephron 1976 16:31-41. [Google Scholar]
[27]. Agaba EI, Wigwe CM, Agaba PA, Tzamaloukas AH, Performance of the Cockcroft-Gault and MDRD equation in adult Nigerians with chronic kidney diseaseInt Urol Nephrol 2009 41:635-42. [Google Scholar]
[28]. Abefe SA, Abiola AF, Olubunmi AA, Adewale A, Utility of predicted creatinine clearance using MDRD formula compared with other predictive formulas in Nigerian patientsSaudi J Kidney Dis Transpl 2009 20:86-90. [Google Scholar]
[29]. WHO. Non-communicable Diseases, Country Profiles 2011. WHO Library Cataloguing-in-Publication Data. Geneva: World Health Organization; 2011. Available at: https://www.who.int/nml/publications/ncd_profiles_reports.pdf [Google Scholar]
[30]. National Kidney FoundationK/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney diseaseAm J Kidney Dis 2004 43(5 Suppl 1):S1-290. [Google Scholar]
[31]. Barsoum RS, Francis MR, Spectrum of glomerulonephritis in EgyptSaudi J Kidney Dis Transpl 2000 11:421-29. [Google Scholar]
[32]. Banaga ASI, Mohammed EB, Siddiq RM, Salama DE, Elbashir SB, Khojali MO, Causes of end-stage renal failure among haemodialysis patients in Khartoum State/SudanBMC Res Notes 2015 8:502 [Google Scholar]
[33]. Ulasi II, Ijoma CK, The enormity of chronic kidney disease in Nigeria: the situation in a tertiary hospital in South-East NigeriaJ Trop Med 2010 2010:501957 [Google Scholar]
[34]. Ghonemy TA, Farcg SE, Soliman SA, El-okely A, El-hendy Y, Epidemiology and risk factors of chronic kidney disease in the El-Sharka Governorate, EgyptSaudi J Kidney Dis Transplant 2016 27(1):111-17. [Google Scholar]
[35]. AIHW. Cardiovascular disease, diabetes and chronic kidney disease-Australian facts: risk factors. Cardiovascular, diabetes and chronic kidney disease series no. 4. Cat. No. CDK 4. Canberra: Australian Institute of Health and Welfare; 2015. Available at: https://www.aihw.gov.au/getmedia/Od8f3064-5dte-4508-868a-53c9ccfd3f6a/18550.pdf [Google Scholar]
[36]. Zuo L, Wang M, Current status of maintenance haemodialysis in Beijin, ChinaKidney Int 2011 3(2):167-69. [Google Scholar]
[37]. Badheeb AM, Causes of chronic renal failure in haemodialysis unit: a single center experience in YemenSaudi J Kidney Dis Transpl 2006 17(1):66-69. [Google Scholar]
[38]. Bommer J, Prevalence and socio-economic aspects of chronic kidney diseaseNephrol Dial Transplant 2002 17:08-12. [Google Scholar]
[39]. Zoccali C, Kramer A, Jager KJ, Chronic kidney disease and end-stage renal disease – a review produced to contribute to the report “the status of health in the European Union: towards a healthier Europe”NDT Plus 2010 3(3):213-24. [Google Scholar]
[40]. Odonmeta BA, Unuigbe E, Otene CI, Pruritus in patients on maintenance haemodialysis in Benin City, Edo state, NigeriaJ Integr Nephrol Androl 2016 3:114-17. [Google Scholar]
[41]. Falodun O, Ogunbiyi A, Salako B, George AK, Skin changes in patients with chronic renal failureSaudi J Kidney Dis Transplant 2011 22(2):268-72. [Google Scholar]
[42]. Elder SJ, Pisoni LR, Akinzawa T, Fissel R, Andreucci VE, Fukuhara S, Sleep quality predicts quality of life and mortality risk in haemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS)Nephrol Dial Transpl 2008 23(3):998-1004. [Google Scholar]
[43]. Erturk IE, Arican O, Omurla IK, Sut N, Effects of the pruritus on the quality of life: a preliminary studyAnn Dermatol 2012 24(4):406-12. [Google Scholar]
[44]. Macaron G, Fahed M, Matar D, Bon-Khalil R, Kazour E, Nehme-Chlela D, Anxiety, depression and suicidal ideation in Lebanese patients undergoing haemodialysisCommunity Ment Health 2014 50(2):235-38. [Google Scholar]
[45]. Walker RL, Lester D, Joe S, Lay theories of suicide: an examination of cultural relevant suicide beliefs and attributions among African Americans and European AmericansJ Black Psychol 2006 32(3):320-34. [Google Scholar]
[46]. Strom JL, Egede Le, The impact of social support on outcomes in Adult patients with Type 2 diabetes: a systematic reviewCurr Diab Rep 2013 12(6):769-81. [Google Scholar]
[47]. Miller TA, DiMatteo MR, Importance of family/social support and impact on adherence to diabetic therapyDiab Metab Syndr Obes 2013 6:421-26. [Google Scholar]
[48]. Adinkrah M, Anti-suicide laws in nine African countries: criminalization, prosecution and penalizationAfr J Crim Justice Stud 2016 9(1):279-92. [Google Scholar]