Unintended pregnancies and its consequences are a considerable public health problem. In order to cope with this problem healthcare providers must inform their patients seeking for contraceptive methods effectively. IUD are reversible, safe and effective contraceptive method for most women [1]. Fear of pain and provider dependence may limit the application of this contraceptive method. However, number of studies evaluating pain relief during IUD insertion were conducted by clinicians. Several analgesic methods were used including oral analgesics {Non Steroidal Anti Inflammatory Drugs (NSAIDs), paracetamol, misoprostol} and parenteral injection of local anaesthetic agents (intracervical, intrauterine and paracervical) for this purpose [2-5]. Pain during IUD insertion is rarely severe, because procedure is short and easy. However, reducing the pain with any method during insertion can improve patient comfort and also reduce pain related to vasovagal syncope especially in patients with cervical stenosis [6,7]. Nonopioid analgesics, NSAIDs and paracetamol inhibits the enzyme cyclooxygenase; however, paracetamol is a weak inhibitor and acts in the central nervous system rather than the periphery. Paracetamol also has a good safety profile, passes through the brain barrier easily [8] and is metabolised from liver. Some authors suggested that, as paracetamol has no anti-inflammatory effect, it is unlikely to have a significant analgesic effect on pain induced by prostaglandin release which arise from uterine or cervical distension [7]. In this randomized controlled trial, paracervical block with lidocaine and paracetamol with control group were compared with respect to pain reduction during and after IUD insertion.
Materials and Methods
This prospective randomized controlled study was performed at primary healthcare hospital for a four months period between February 2013 and May 2013. Women who were admitted requesting for insertion of IUD were enrolled to the study. Institutional approval from the Local Research Ethical Committee was obtained prior to conducting this study. All subjects provided written informed consent prior to enrollment.
Patients were excluded from study if they have any contraindication to use IUD (gynaecologic malignancy, pelvic inflammatory disease, unexplained vaginal bleeding and pregnancy). Patients who were in postpartum period and allergic to drug used were also excluded.
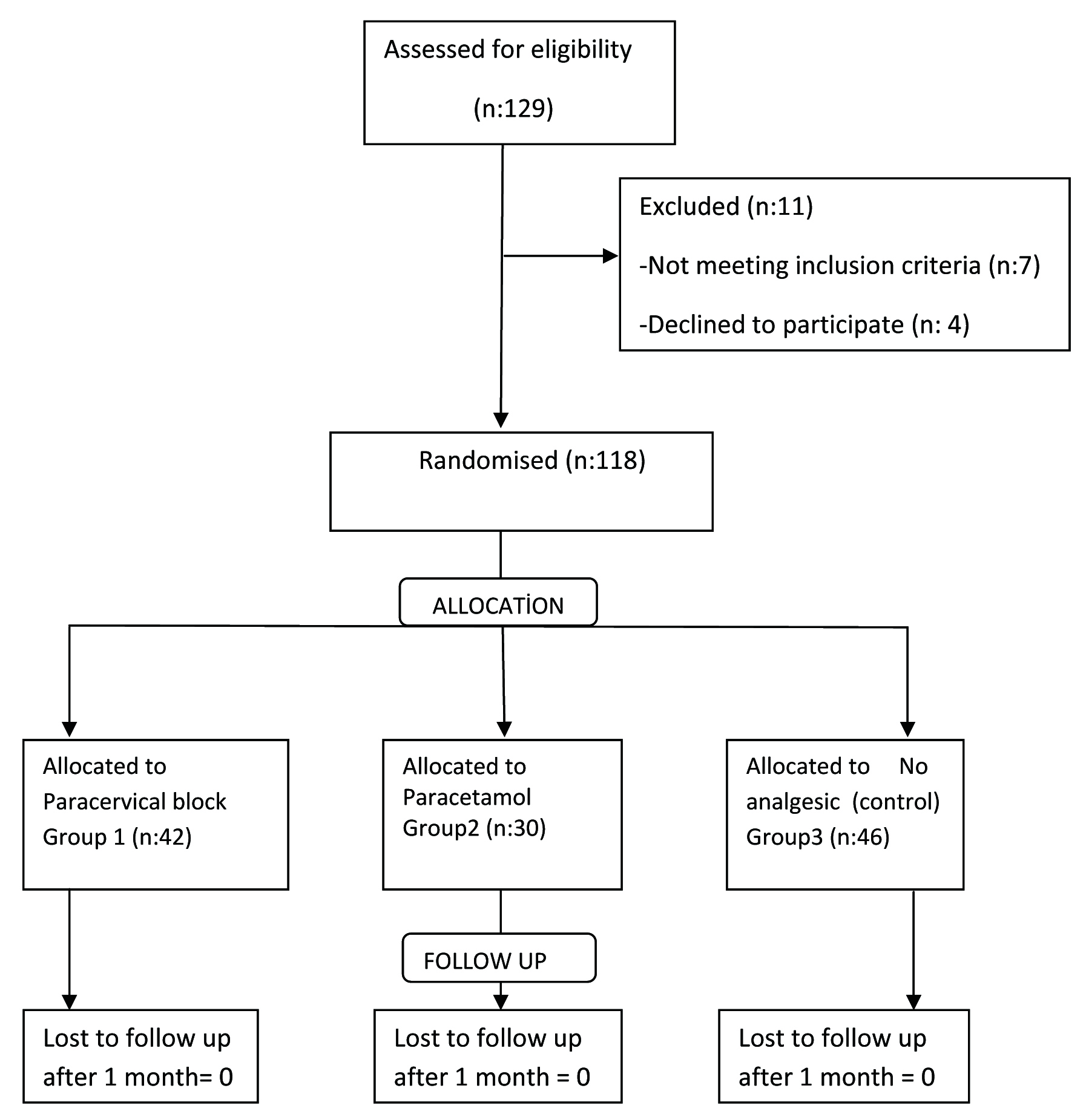
A total of 118 patients were allocated to three groups by closed envelope method of randomization. At the end of randomization, there were 42 patients in paracervical block group (Group 1), 30 patients in paracetamol group (Group 2) and 46 patients in no intervention group (Group 3). Study flow chart is shown on [Table/Fig-1].
Beta-HCG was performed in all patients before procedure and all were negative. All insertion procedures were performed by the same experienced clinician. Hence, provider was not blinded. An interview was performed before the procedure regarding the knowledge of patients medical and reproductive history including age, gravidity, parity, level of education, mode of prior delivery, time from last delivery, breastfeeding status, day of the menstrual cycle at procedure, prior contraception method (recent IUD usage or past IUD experience due to possible difference of pain perception). CuT380A IUD (ParaGard®) was used in all patients. Clinician placed speculum after bimanual examination, cleaned vagina and cervix with povidone iodine.
In Group 1, two sided (4-8 o’clock) paracervical block was performed five minutes before the procedure with using 10 mL 2% lidocaine (Jetokain®; Adeka, Turkey). Patients in Group 2 received 500 mg oral paracetamol, 20 minutes before the procedure. Patients in Group 3 did not receive any analgesic method before IUD insertion. Ring forceps was used for cervical manipulation during insertion. Cervical dilatation was not performed before insertion. IUD was placed with standardised technique.
Pain scores were measured with a 10-point VAS which was graded 0 (no pain) to 10 (worst pain). Patients were asked to indicate their pain level during insertion (VAS1) and five minutes after the procedure (VAS2). Five minute VAS score was set similar to a previous study [9].
Position of IUD was verified by pelvic ultrasonography after pain scores were recorded. Complications related with the procedure (vasovagal symptoms, vasovagal syncope, bleeding, immediate expulsion or mispositioning, uterine perforation) were recorded at follow up visits one month later.
Two out of ten on VAS was determined as to be clinically significant by the help of previous studies [10,11]. To detect a mean difference between groups of two out of ten on VAS with 80% power, 20 women for each group was chosen.
The primary end point was to determine the pain scores using VAS, according to different analgesic intervention methods.
Statistical Analysis
Statistical analysis was performed with SPSS statistical software (version 22.0; SPSS, Chicago, IL). Baseline characteristics of the study group were compared using Pearson Chi-square test for dichotomous variables and one way ANOVA test for quantitative variables. VAS scores were also compared with one way ANOVA test. Data were reported as mean with standard deviation and percentiles. A p-value less than 0.05 was considered to indicate statistical significance.
Results
A total of 129 patients were admitted to the clinic with the request of IUD insertion. Eleven patients were excluded from the study (seven according to study exclusion criterias, four declining to participate). Remaining 118 patients were enrolled into the study and randomized. Paracervical block was performed in 42 patients (Group 1), 30 patients received paracetamol (Group 2) and 46 patients did not receive any analgesic (Group 3). The baseline characteristics of the study groups were comparable regarding mean age, gravidity and parity. Also, the ratio of elementary school graduation, IUD use in last three months, prior IUD use in any time, vaginal birth as a mode of prior delivery, time interval from last delivery being > one year and the follicular phase insertion were comparable between three groups [Table/Fig-2]. None of the patients were in the breastfeeding mothers.
Baseline characteristics of patients.
| Variables | Group 1Paracervical block (n:42) | Group 2Paracetamol(n:30) | Group 3No intervention (n:46) | p-value |
|---|
| Age (years) | 33.1 (±7.3) | 31.2 (±8.1) | 33.0 (±8.3) | NS |
| Gravidity | 2.9 (±1.3) | 2.4 (±0.9) | 2.8 ±1.2) | NS |
| Parity | 2.6 (±1.0) | 2.4 (±0.8) | 2.7 (±1.0) | NS |
| Educational status, elementary school % | 33 (78.5) | 20 (66.7) | 33 (71.7) | NS |
| IUD usage in last three months (%) | 26 (11) | 35.7 (10.28) | 34.8 (16) | NS |
| Prior IUD usage (%) | 59.5 (25) | 64.3 (18.28) | 60.9 (28) | NS |
| Mode of prior delivery, vaginal birth (%) | 64.3 (27) | 78.6 (22.28) | 78.3 (36) | NS |
| Time interval from last birth, > one year (%) | 64.9 (24.37) | 73.6 (22.28) | 56.8 (25.44) | NS |
| Early follicular phase insertion (%) | 73.6 (14.19) | 50.0 (10.20) | 73.6 (14.19) | NS |
NS:non significant
In this table Pearson Chi-square test for dichotomous variables and one-way ANOVA test for quantitative variables were used for statistical analysis.
Mean VAS1 and VAS2 scores of groups were 3.69±1.6 and 3.02±0.1 for Group 1; 3.73±0.8 and 3.0±0.7 for Group 2; 4.37±1.4 and 3.83±1.2 for Group 3 respectively. There were no significant difference between VAS1 of the three groups. However, VAS2 scores were significantly different between Group 3 and both Group 1 (p< 0.001) and Group 2 (p<0.001). Neither VAS1 scores (p=0.9) nor VAS2 scores (p=0.5) were different between Group 1 and 2 [Table/Fig-3].
Pain scores of patients on 10 point VAS.
| Pain score | Group 1Paracervical block (n:42) | Group 2Paracetamol (n:30) | Group 3No intervention (n:46) | p-value |
|---|
| VAS1(range){during procedure} | 3.69±1.6 (3-10) | 3.73±0.8 (4-6) | 4.37±1.4 (3-8) | 0.1 *0.05 **0.9 *** |
| VAS2 (range){5 minutes after procedure} | 3.02±0.1 (3-4) | 3.00±0.7 (3) | 3.83±1.2 (3-8) | <0.001 *<0.001 **0.5 *** |
Values are mean ± standard deviation, range (minimum-maximum),
*Group 1-3,**Group 2-3,***Group 1-2
VAS: visual analogue scale, VAS scores were compared with one way ANOVA test
In this table Pearson Chi-square test for dichotomous variables and one way ANOVA test for quantitative variables were used for statistical analysis.
Also, mean VAS1 and VAS2 scores did not change significantly among recent or previous IUD users in three groups (data not shown). All patients had successful IUD insertion at first attempt. Procedural complications such as vasovagal symptoms and syncope, bleeding, immediate expulsion or mispositioning and uterine perforation did not occur.
Discussion
Female reproductive system is innervated by two main pathways, symphatetic fibers from T10-L2 and parasympathetic fibers from S2-S4. While symphathetic fibers innervate uterine fundus via inferior hypogastric plexus and ovarian plexus, parasymphathetic fibers uses different pathway through uterine vessels at 3 o’clock and 9 o’clock and innervate cervix, lower uterine segment and upper vagina [12]. Pain from cervical dilatation, is carried by parasympathetic fibers that accompany the uterine vessels and cardinal ligament while pain from contraction or cramping is transmitted with sympathetic fibers which travels in the uterosacral ligament [8]. In this study, we evaluated the effects of lidocaine and paracetamol on pain originating from IUD insertion.
Lidocaine is the most commonly used amine group local anaesthetic due to lower risk of allergic reaction and lower cost. Paracervical block with lidocaine has been used for many gynaecologic procedure effectively. But, an important dilemma is that paracervical block itself causes some level of discomfort [13]. Paracervical injection of local anaesthetics block nerve fibers at 3 o’clock and 9 o’clock position and reduces mostly cervical manipulation related pain (dilatation, passage etc.,) [12].
Tenaculum is used for decreasing uterine anteflexion and increasing comfort during linear passage of uterine cavity. Tenaculum placement is also an important cause of pain during office manipulations. Gentle manipulation of cervix with ring forceps rather than tenaculum in our study eliminated the wrong pain perception originating from tenaculum. Also, procedures were performed by the same provider thus provider dependent pain perception was also eliminated. After tenaculum placement, uterine sounding, insertion of device and myometrial contractions after insertion were the other steps stimulating pain signals. Nulliparity, longer time interval between last menstruation and last pregnancy, age greater than 30 year, dysmenorrhea, no breastfeeding status are the risk factors for increasing pain perception during IUD insertion [14-17]. In our study, none of the patients were nulliparous, mean age for all groups was above 30, none of the patients were breastfeeding. Time interval from last pregnancy and last menstruation of population is also homogeneous.
Also, in some studies [18], paracetamol was found to be an inferior choice of NSAIDs for uterine pain, however, it is an alternative choice for women who cannot tolerate NSAIDs [18]. Additionally, in our study, oral paracetamol group had a lower mean VAS1 scores than no intervention group and p-value was statistically significant (p>0.05). The lower VAS2 scores of both intervention group showed that paracervical block with 1% lidocaine and oral paracetamol is both effective in reducing pain after IUD insertion.
Moreover to our knowledge, this is the first study showing the effectiveness of oral paracetamol in pain reduction during IUD insertion. These findings and our pain scores are consistent with published literature [9,16]. Allen RH et al., conducted a cochrane review, analysing a variety of interventions for pain reduction during IUD insertion. The authors concluded that NSAIDs were not effective in reducing pain from IUD insertion [17]. In the randomized trial by Mody SK et al., a paracervical block also did not show a statistically significant decrease in pain with IUD insertion [9]. In the study by Hubacher D et al., which analysed the effect of 400 mg ibuprofen 45 minute before the procedure statistical significant difference was not observed between placebo and ibuprofen [16]. In 2015, Lopez LM et al., reassessed the pain reducing interventions for IUD insertion in a cochrane review. They concluded that currently most NSAIDs were not effective, but some lidocaine formulations, naproxen and tramadole had some effect on pain reduction during IUD insertion [14]. So far, there is no study analysing effect of paracetamol on IUD insertion.
Various VAS scores were reported in different published series [9,16]. In the study by Mody SK et al., median pain score was 62 point and in the study by Hubacher D et al. the score was 10 point according to 100 point VAS [9,16]. Our scores were relatively lower but close to the study of Hubacher D et al., [16]. These dissimilar findings are attributable to the effect of cultural difference and heterogeneity of the study populations in terms of confounding factors of pain perception. However, our study population was homogeneous for the distribution of possible factors previously discussed above.
Limitation
There are some limitations in our study. Provider was not blinded and postprocedural late pain (after 4-6 hours) was not recorded. Also, the same person assessed the VAS1 and VAS2 scores which could have created a bias. Moreover, the presence of a group without any pain medication for IUD insertion could be criticised. But, there are no established guidelines regarding the appropirate use of analgesics in IUD insertion. In a study comparing ibuprofen and placebo, there was no difference with the use of NSAID during IUD insertion [19].
However, to our knowledge, this is the first study comparing paracetamol and paracervical block in IUD insertion. And one of the strengths of the study is its prospective randomized study.
Conclusion
This study supports the use of analgesic method for IUD insertion. However, the mode of analgesic does not differ, paracetamol and paracervical block are both effective methods in relieving pain after insertion.
NS:non significant
In this table Pearson Chi-square test for dichotomous variables and one-way ANOVA test for quantitative variables were used for statistical analysis.
Values are mean ± standard deviation, range (minimum-maximum),
*Group 1-3,**Group 2-3,***Group 1-2
VAS: visual analogue scale, VAS scores were compared with one way ANOVA test
In this table Pearson Chi-square test for dichotomous variables and one way ANOVA test for quantitative variables were used for statistical analysis.