Nasopharyngeal Pleomorphic Adenoma: A Difficult Surgical Proposition
Champion Venkateshalu Srinivas1, A. Mahesh2, Swati Nair3
1 Associate Professor, Department of Ear, Nose and Throat, Dr. BR Ambedkar Medical College and Hospital, Bengaluru, Karnataka, India.
2 Associate Professor, Department of Surgery, Dr. BR Ambedkar Medical College and Hospital, Bengaluru, Karnataka, India.
3 Junior Resident, Department of Ear, Nose and Throat, Dr. BR Ambedkar Medical College and Hospital, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Swati Nair, 504, A Block, Favourite elegance, Shampura Main Road, Kavalbyrasandra, Bengaluru-560032, Karnataka, India.
E-mail: nairswati.304@gmail.com
Salivary gland tumours of the nasopharynx are rare and when present, tend to be malignant. Here, we report an unusual case of benign pleomorphic adenoma of the minor salivary gland arising from the nasopharynx in a 21-year-old female who presented with unilateral nasal obstruction. The radiological features of non-invasion of surrounding structures gave the first clue of benignity of the lesion as well as the location, size and anatomical relations of the tumour with the surrounding structures. This information was useful in planning the surgical approach and predicting the prognosis. Local and adequate excision appeared to be adequate.
Benign mixed tumour, Minor salivary glands, Nasopharynx
Case Report
A 21-year-old female was referred to us with complaints of gradually progressive, left sided nasal obstruction since three years. On thorough clinical examination, a bulging was present on the soft palate on the left side and the uvula was pushed to the opposite side. The left sided tonsil was noted to be pushed medially, almost up to the midline [Table/Fig-1]. On diagnostic nasal endoscopy, a soft tissue bulge was seen over the roof of the left side of the soft palate with septal spur bilaterally with deviation of nasal septum to right.
Clinical picture showing bulge over the soft palate, uvula and tonsil being pushed to the opposite side.

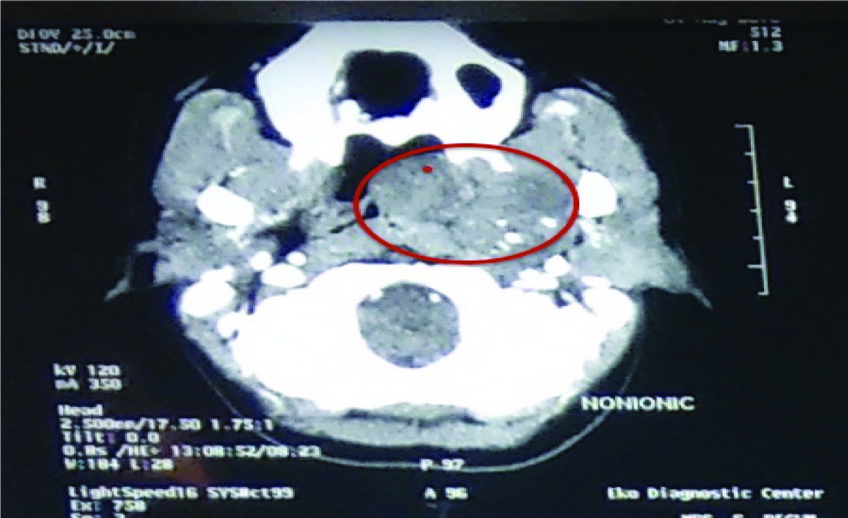
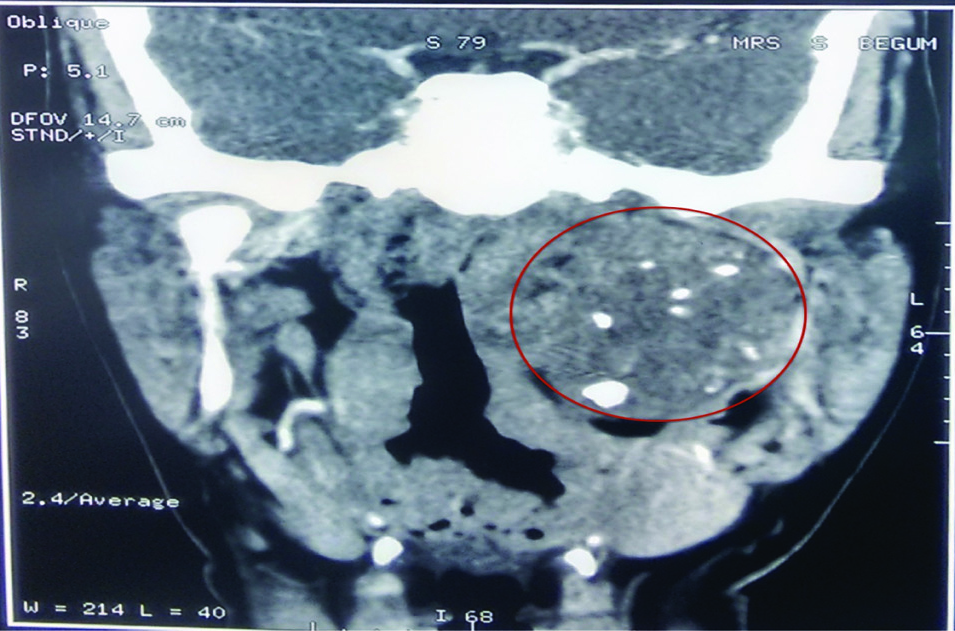
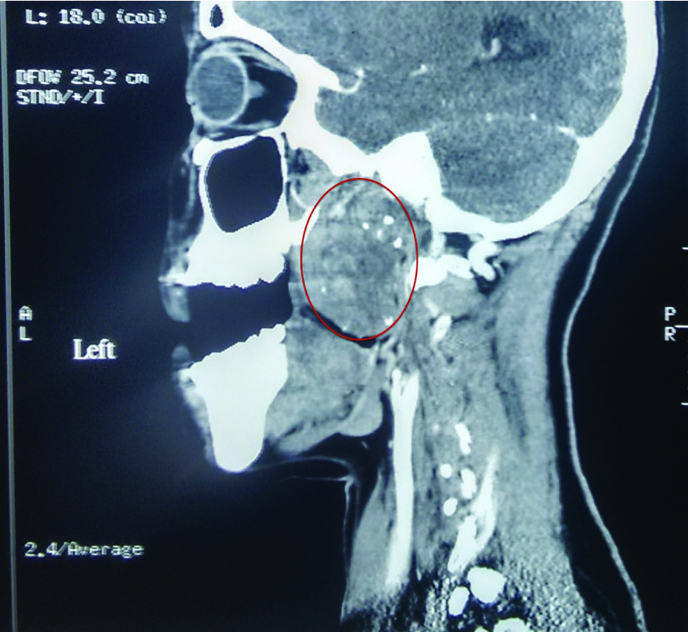
The patient had already been evaluated with a plain and contrast- enhanced MDCT scan of the nasopharynx and the parapharyngeal space done in the axial plane with multiplanar reformations. These imaging tests showed a fairly large ill-defined heterogeneously enhancing soft tissue lesion with internal nodular calcifications involving pharyngeal mucosal space and parapharyngeal space on the left side at the nasopharyngeal level extending onto the oropharynx [Table/Fig-2,3]. The lesion measured about 5.8 X 5.1 X 3.9 cm in size and caused gross narrowing of the nasopharyngeal airway [Table/Fig-4]. There was obliteration of the fossa of Rosenmuller on the left side. The infratemporal fossa was normal and the right side appeared to be free of disease. Submandibular and parotid salivary glands were normal on either side. There was no enlarged lymph node seen in the neck. Ear and laryngeal examination were within normal limits.
Axial section showing the medial and lateral extent of the tumour. Laterally, the tumour is extending into the parapharyngeal space.
Coronal section showing the superior and inferior extent of the tumour. Superiorly, extending up to the skull base. Internal nodular calcifications seen.
Sagittal section showing the anterior and posterior extent of the tumour.
An intraoral incisional punch biopsy of the tumour was performed which on microscopy showed both epithelial and stromal elements. The epithelial elements formed trabeculae and tubules. The ductules showed both the epithelial and myoepithelial components and the stroma showed hyaline cartilage. It was confirmed to be a pleomorphic adenoma of a minor salivary gland.
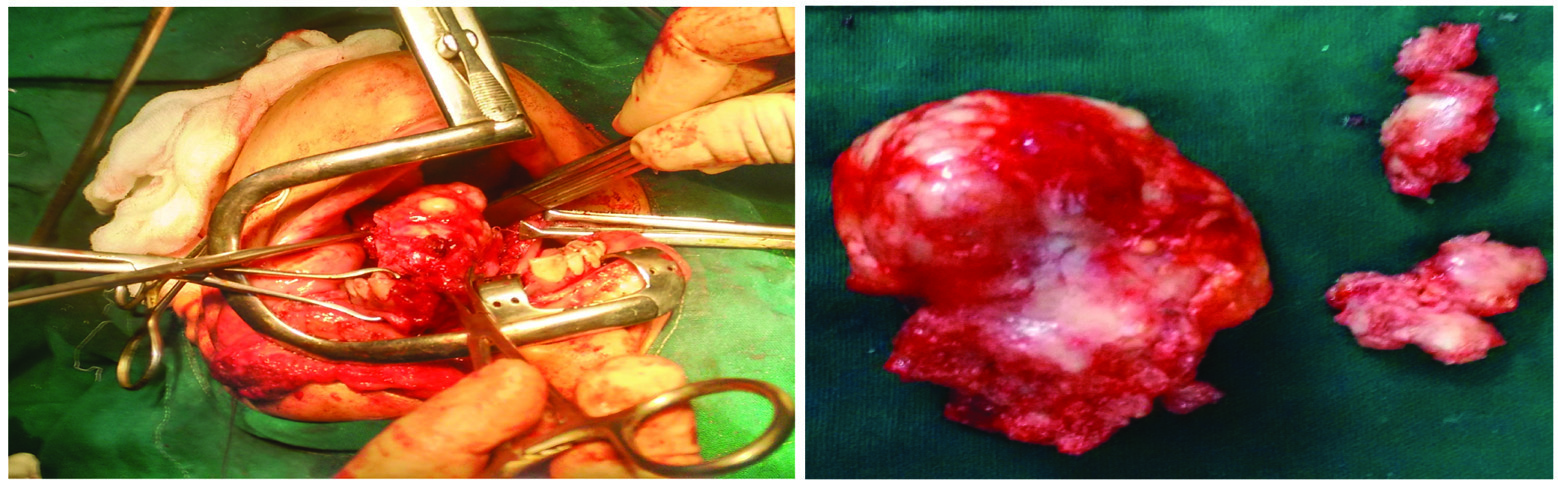
A complete surgical excision was planned for the patient. Following elective tracheostomy, a transcervical approach to the tumour was attempted but since the tumour was deep and higher up, it could not be accessed. Following this, a lateral rhinotomy and lip split were performed and the maxilla was split in the midline using a microdrill and a gigli saw and the tumour was exposed. On digital palpation, the tumour was noted to be extending deep into the left parapharyngeal space and was delivered by blunt dissection as it was a well-encapsulated tumour [Table/Fig-5,6]. Complete surgical removal of the tumour was done and intermaxillary wiring was done [Table/Fig-7]. The wire was removed after three months. The patient reported an improvement in symptoms and the nasopharynx was disease-free even at six months.
Enucleation of the tumour.

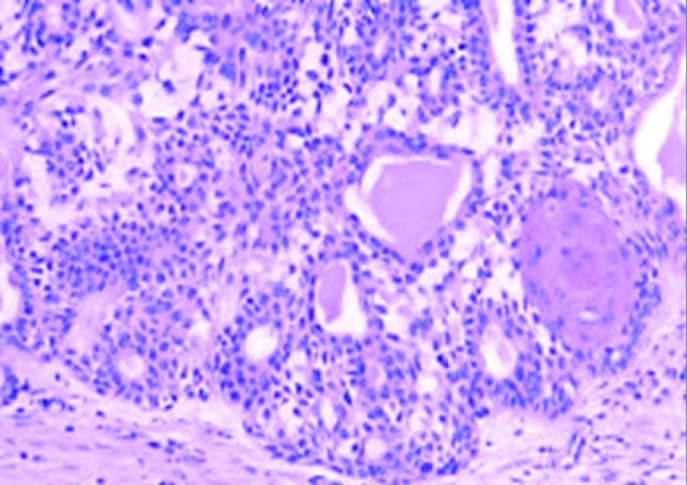
On histopathological examination of the mass, the tumour was composed of epithelial and stromal elements. The epithelial elements were oriented in cords, tubules and nests; consisting of cells with uniform round nuclei and moderate cytoplasm. The stroma was a mixture of fibrous, myxomatous and focally chondromyxomatous elements. A mild diffuse mononuclear cell infiltration was noted. No evidence of malignancy was seen. The features were suggestive of benign mixed tumour or pleomorphic adenoma of the minor salivary gland [Table/Fig-8].
Histopathological appearance of the tumour.
Discussion
Benign tumours of nasopharynx are rare, as nasopharynx is considered as one of the notorious anatomical sites for malignant tumours. Pleomorphic adenoma or benign mixed tumour is the most common salivary tumour, accounting for up to two-thirds of all salivary gland neoplasms [1]. Approximately 85% of all pleomorphic adenomas are found in the parotid glands, 10% in the minor salivary glands and 5% in the submandibular glands [2]. These are benign tumours. If the minor salivary glands are involved, the most common site is palate but it can also occur in other sites including the upper lip, cheek, pharynx, floor of the mouth, larynx and trachea [3,4]. The first site of origin in nasopharynx is very rare. For most tumour types, there is a slight female preponderance. All age groups may be affected. However, the most common age for the presentation of a benign salivary gland tumour is the fourth decade of life [5]. Palate, nasal cavity and nasopharynx have abundant salivary glands and pleomorphic adenoma is the most common benign tumour of these glands.
When a pleomorphic adenoma arises from the nasopharynx, the major symptom is nasal congestion due to obstruction of the nasal airway. Other symptoms, such as epistaxis, otalgia, dysphagia, hearing loss, mucopurulent rhinorrhea and serous otitis media may also be reported [6]. Prominent bulge over the soft palate before the lateral pharyngeal wall and tonsil are pushed medially which is one of the earliest features of a parapharyngeal mass [7]. Pleomorphic adenoma in the parapharyngeal space most commonly arises from the deep lobe of parotid, palpated externally as a retromandibular mass [7]. In this patient, CT localized the tumour to the nasopharynx causing gross narrowing of nasopharyngeal airway with obliteration of fossa of Rosenmuller as well as the parotids were normal on both sides. The patient can present with complaints of trismus and with symptoms of cranial nerves 9,10,12 or sympathetic chain involvement, which was not seen in our patient [7].
A retrospective study by Prasad SC et al., indicated that benign Parapharyngeal Space (PPS) tumours can be effectively managed with a lateral skull base approach, which, according to the investigators, offers excellent exposure and reduced morbidity [8]. Transcervical, transcervical-transparotid, transcervical-transmastoid, and infratemporal fossa approaches were used, with 46 of 48 tumours (96%) undergoing total radical removal [8]. Transcervical approach could not expose the tumour in this case.
The tumour is usually well encapsulated and appears with a smooth surface, an elastic and rubbery structure upon physical examination with no destruction of the mucosa of the adjacent structures. In addition, it does not bleed easily. Microscopically, epithelial, myoepithelial and stromal elements usually form the histologic structure of pleomorphic adenomas [9]. Myxoid, cellular and mixed types are the main histologic subgroups of pleomorphic adenoma. Radiological evaluation and endoscopic examination are very useful in deciding the most appropriate surgical treatment. CT provides excellent detail of tumour volume and can help with surgical planning in identifying the relation to vessels and bony landmarks as well as identify involved lymphatics. However, it requires contrast and radiation. In contrast, MRI does not require ionization radiation, provides excellent soft tissue detail. MRI is superior in defining the tumour boundaries and is thought to be more useful to determine if nerve involvement is present [10]. An incisional biopsy is a must for initial diagnosis before the main treatment of the tumour.
Complete surgical excision is necessary for tumours with histologically clear margins but may not be easy owing to its proximity to important structures, like the eustachian tube and cranial nerves. Complications like bleeding and eustachian tube dysfunction can occur after surgery. Surgical resection may be done either by a transnasal endoscopic approach or by an external such as the transpalatal, transmaxillary, transmandibular and transpterygoid approach but the external approaches may lead to postoperative morbidity. Roh et al., treated a case of nasopharyngeal pleomorphic adenoma with surgical approach using the endoscope [3]. Also Lee SL et al., used the endoscopic approach with excellent results [11]. Thakur JS et al., were the only ones to utilize the FNAC for first and erroneous diagnosis of carcinoma [12]. In this case, since it was a large tumour with extension into the parapharyngeal space, a transmaxillary approach was taken with maxillary split for removal of the tumour.
Conclusion
Pleomorphic adenoma of the nasopharynx is a very rare disease. The radiological feature of non-invasion, clinical presentation of the tumour showing no bleeding and multilobulated appearance gives us clues on the diagnosis. The final confirmation is by the histopathological examination. From the review of literature and our experience, the gold standard for treatment is surgical excision, either by an endoscopic approach or transmaxillary, transpalatal, transmandibular and transpterygoid approach.
[1]. Califano J, Eisele DW, Benign salivary gland neo- plasmsOtolaryngol Clin North Am 1999 32(5):861-73. [Google Scholar]
[2]. Luna MA, Salivary glands. In: Pilch BZ, editorHead and neck surgical pathology 2001 PhiladelphiaLippincott Williams and Wilkins:284-349. [Google Scholar]
[3]. Roh JL, Jung BJ, Rha KS, Park CI, Endoscopic resection of pleomorphic adenoma in the nasopharynxActa Otolaryngol 2005 125(8):910-12. [Google Scholar]
[4]. Amilibia E, Nogues J, Sandoval M, Arias G, Dicenta M, Minor salivary gland tumour in nasopharynxActa Otorrinolaringol Esp 1997 48(8):671-73. [Google Scholar]
[5]. Gleeson M, Cawson R, Benign salivary gland tumours, In: Kerr AG, editorScott Brown’s Otorhinolaryngology 2008 vol:27th edGreat BritainButterworth International Editions:2475 [Google Scholar]
[6]. Maruyama A, Tsunoda A, Takahashi M, Kishimoto S, Suzuki M, Nasopharyngeal pleomorphic adenoma presenting as otitis media with effusion: Case report and literature reviewAm J Otolaryngol 2014 35:73-76. [Google Scholar]
[7]. Gourin C.G. Parapharyngeal Space Tumours [Internet]. 2015. [cited 3 May 2017]. Available from: http://emedicine.medscape.com/article/849385-overview#a8 [Google Scholar]
[8]. Prasad SC, Piccirillo E, Chovanec M, La Melia C, De Donato G, Sanna M, Lateral skull base approaches in the management of benign parapharyngeal space tumoursAuris Nasus Larynx 2015 42(3):189-98. [Google Scholar]
[9]. Berrettini S, Fortunato S, De Vito A, Bruschini L, A rare case of nasopharyngeal pleomorphic adenomaCase Rep Otolaryngol 2013 2013:712873 [Google Scholar]
[10]. Pernas F.G, Current Controversies in the Management of Malignant Parotid TumoursUnpublished Thesis. The University of Texas Medical Branch 2011 [Google Scholar]
[11]. Lee SL, Lee CY, Silver SM, Kuhar S, Nasopharyngeal pleomorphic adenoma in an adultLaryngoscope 2006 116(7):1281-83. [Google Scholar]
[12]. Thakur JS, Mohindroo NK, Mohindroo S, Sharma DR, Thakur A, Pleomorphic adenoma of minor salivary gland with therapeutic misadventure: A rare case reportBMC Ear Nose Throat Disord 2010 10:2 [Google Scholar]