The present study was conducted to evaluate the efficacies of ramipril as monotherapy compared to combination therapy of ramipril and torsemide in hypertensive patients and to study the adverse effects of both the drugs.
Materials and Methods
The present study was prospective, open labeled, randomized parallel study with intention to treat patients of Stage I and Stage II hypertension who attended outpatients and wards in the department of Medicine in GGS Medical College & Hospital. In total, 100 consecutive newly diagnosed patients were recruited in the study during October 2015 to June 2016.
Stage I and Stage II hypertensive patients were enrolled in the study. Our target was to reduce BP to (<140/90 mmHg), and to determine the effect of Ramipril in one group and Ramipril with torsemide in other group on primary outcome of BP reduction [8]. Also to evaluate the effect in both treatment groups i.e. how much BP reduction will occur and in how much time period along with the safety of the same.
In Indian population no study was found on Torsemide and Ramipril therapy in such patients.
This research project was undertaken in Baba Farid University of Health Sciences, Faridkot as a self-funded project within the scope of postgraduate curriculum research. Institution Ethics Committee (IEC) approved the study in September 2014 and the study was commenced after receiving approval from IEC Letter no. BFUHS/2K14/P-Th/8903.
Inclusion criteria: Newly diagnosed Stage 1 and Stage II hypertensive patients aged 18 years and above with normal renal function were enrolled as per classification of hypertension according to JNC 7, British Heart Society, Indian Hypertension guidelines:
Stage I - 140-159 mmHg (SBP) / 90-99 mmHg (DBP)
Stage II - 160-179 mmHg (SBP) / 100-109 mm Hg (DBP)
Exclusion criteria: Patients with Stage III hypertension (BP ≥180/110 mmHg), secondary hypertension, pre-eclampsia and eclampsia, bilateral renal artery stenosis, renal failure, cardiovascular disorders including concomitant unstable angina pectoris, heart failure, life-threatening arrhythmia, myocardial infarction or previous coronary revascularization and stroke were excluded. Patients on oral contraceptive pills, pregnant and lactating mothers and patients already on antihypertensive drugs or those severely ill were also excluded.
Sample size calculation: The calculations suggested that approximately 90 subjects (45 per treatment arm) were required for this study considering 10% drop out (which was anticipated) and therefore, 50 per treatment arm were planned to be recruited. The calculations were driven by the effect of treatment difference of SBP and DBP administering ramipril as monotherapy and combination of ramipril with torsemide in hypertensive patients with Stage I and Stage II. Statistical tests performed using student’s t-test at a significance level of 5% and with a statistical power of 80%. The power would enable detection of any difference ≥ 5 mmHg in SBP between the two groups with common standard deviation of 7 mmHg, which is considered clinically relevant. Similarly, this sample size is also sufficient and statistically powered enough to detect difference of ≥ 3 mmHg in DBP with common standard deviation of 5 mmHg. Moreover, in this self-financed study, the minimum sample size of 50 was considered in both arms to find suitability of “Future directions of the study”. This can be considered as pilot study on the same research hypothesis.
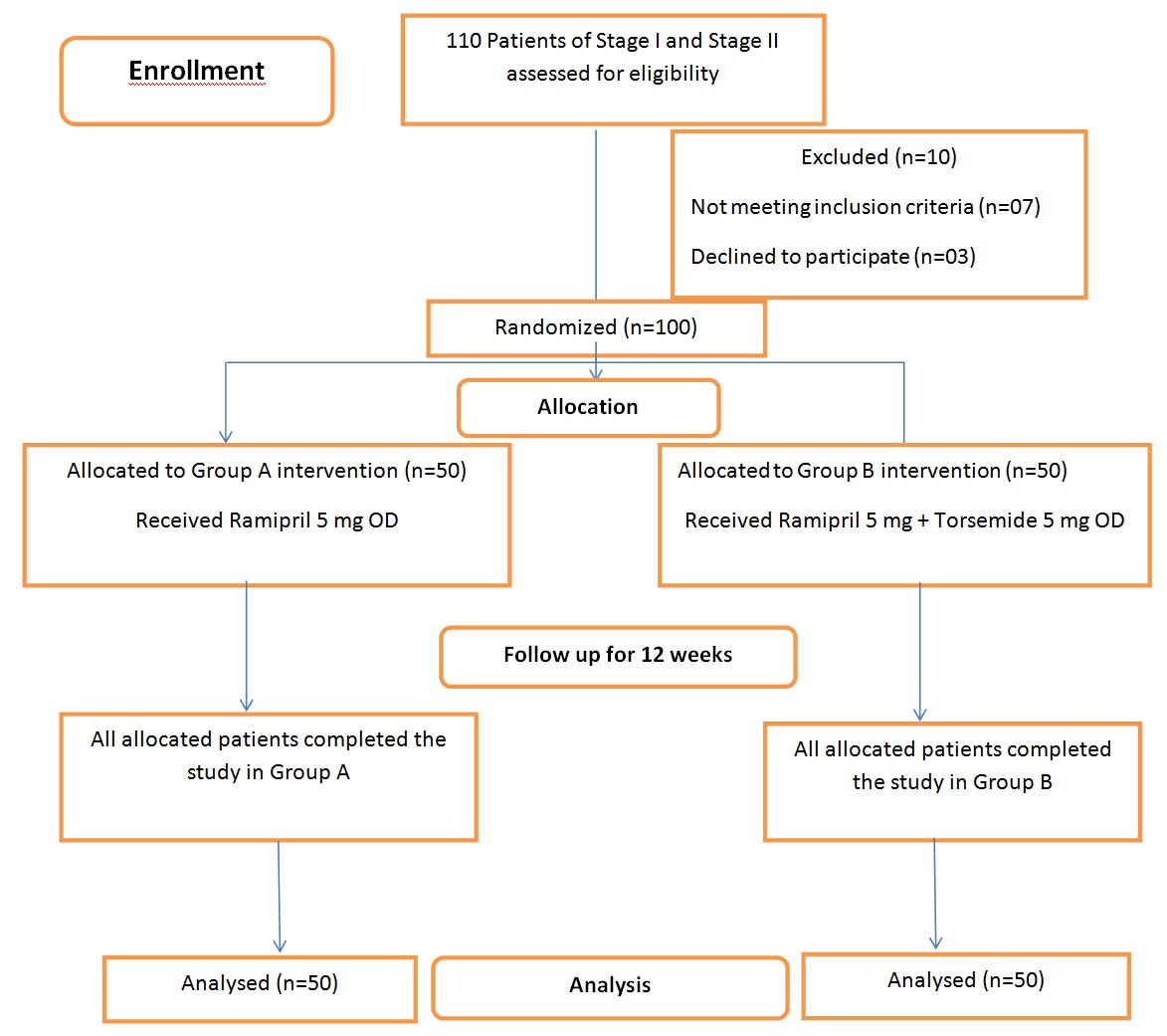
The participants were enrolled after they provided their informed written consent in their vernacular language. They were randomly assigned in two groups A and B of 50 each using random number table as follows [Table/Fig-1]:
Flow chart of the participants as enrolled in the study.
Group A: The participants received ramipril (5 mg) monotherapy.
Group B: The participants received ramipril (5mg) and torsemide (5mg) as Fixed-Dose Combination (FDC) therapy.
Data collection procedure: Each participant was individually counselled prior to the study regarding their right to freely participate in this research project and they had full autonomy to leave the study at any point of time. Moreover, the participants were encouraged to contact the investigators over phone whenever there was a need. Clinical examination was done at the beginning of therapy (1st visit i.e., baseline). Blood pressure was measured in sitting position with the instrument at the level of heart. This was repeated at the end of 2nd, 4th, 8th and 12th week along with recording of adverse reactions, if any. To assess tolerability, the participants were interviewed followed by physical examination including measurement of ankle circumference to check for peripheral oedema, dehydration, nausea, headache, dry cough, asthenia and increase in frequency of urination.
At baseline, investigations viz., electrolytes, lipid profile, blood sugar, blood urea, serum creatinine and complete urine examination were done. During therapy, serum electrolytes, lipid profile, blood urea, Serum creatinine were done to supplement clinically to record adverse drug reactions. Detailed information with the demographic data of the enrolled patients was collected in the Questionnaire. Individual counselling was done on intake of drugs to increase compliance and retention with the prescribed drug regimen during the study period to improve sanctity of the data.
Primary outcome was:
1) To study the efficacy of ramipril as monotherapy and combination of ramipril with torsemide in hypertensive patients.
2) To compare the efficacy of ramipril as monotherapy and combination of ramipril with torsemide in hypertensive patients.
Secondary outcome was: To study the adverse effects in both groups.
Torsemide: It has a longer duration of action and potassium sparing effect as compared to furosemide. So, this combination was chosen to counteract the effect of hyperkalemia. Yet for ethical reasons, we enrolled patients with normal renal function and excluded all other cases such as those of renal failure, cardiac disorders, secondary hypertension etc.
Statistical Analysis
Data was entered in MS Excel master data sheet and analysed using IBM-SPPS version 20.0 for windows. Baseline characteristics of two groups were analysed by Student’s t-test (unpaired t-test). Intragroup comparison of baseline was done at 2nd, 4th, 8th and 12th week with Anova test. p-value with p < 0.05 was taken significant at 5 percent significance level and p < 0.01 was taken significant at 1 percent significance level.
Results
Baseline independent variable characteristics of the patients in both the study groups A and B had no statistically significant difference [Table/Fig-2].
Baseline characteristics of patients in Group A (Ramipril) and Group B (Ramipril and Torsemide). A p-value calculated by Student t-test (unpaired t-test).
| Variables | Group A (n = 50)Mean ± SD | Group B (n = 50) Mean ± SD | p-value |
|---|
| Age (years) | 54.8±11.28 | 53.72±11.67 | 0.639 |
| BMI (Kg/m2) | 28.57±6.17 | 28.51±5.34 | 0.95 |
| Body weight (Kg) | 73.62±15.39 | 73.16±14.26 | 0.877 |
| Gender: | Male | 24 (48 %) | 27 (54%) | |
| Female | 26 (52%) | 23 (46%) | |
| SBP (mmHg) | 156.2±7.92 | 158.32±6.38 | 0.143 |
| DBP (mmHg) | 95.44±5.11 | 97.14±6.47 | 0.148 |
| HR (beats/min.) | 75.96±4.63 | 76.32±4.26 | 0.686 |
In the ramipril monotherapy Group A (n=50), the mean SBP prior to treatment was 156.2±7.92 mmHg and after treatment reduced to 149.16±7.20 mmHg, 143.6±5.92 mmHg, 137.8±6.02 mmHg and 133±7.02 mmHg after 2, 4, 8 and 12 weeks respectively. In ramipril and torsemide FDC treated Group B (n=50), the mean SBP prior to treatment was 158.32±6.38 mmHg and after the treatment reduced to 148.6±7.00 mmHg, 138.56±7.32 mmHg, 131.32±6.64 mmHg and 126±6.84 mmHg after 2, 4, 8 and 12 weeks respectively. In Group B, all these reductions were statistically significant than monotherapy Group A after 4 weeks (p <0.01) [Table/Fig-3].
Comparison of reduction of SBP and DBP between monotherapy and FDC (Group A and B: Both n=50)
| Ramipril monotherapy | Ramipril /Torsemide FDC | ‘t’ value | p-value |
|---|
| Time interval | SBPMean ± SD* | Mean change | Percent fall | SBPMean ± SD* | Mean change | Percent fall |
|---|
| Baseline | 156.2±7.92 | | | 158.32±6.38 | | | -1.47 | 0.144 |
| 2 weeks | 149.16± 7.2 | 7.04± 0.71 | 4.50 | 148.6± 7.00 | 9.72± 0.62 | 6.14 | 0.39 | 0.694 |
| 4 weeks | 143.6± 5.92 | 12.6± 1.99 | 8.06 | 138.56± 7.32 | 19.76± 0.9 | 12.48 | 3.79 | 0.0001 |
| 8 weeks | 137.8± 6.02 | 18.4± 1.89 | 11.77 | 131.32± 6.64 | 27±0 .26 | 17.05 | 5.11 | 0.0001 |
| 12 weeks | 133± 7.02 | 23.2± 0.89 | 14.85 | 126± 6.84 | 32.32± 0.5 | 20.41 | 5.18 | 0.001 |
| | | |
| Time interval | DBPMean±SD* | Mean change | Percent fall | DBPMean±SD* | Mean change | Percent fall | | |
| Baseline | 95.44±5.11 | | | 97.14±6.25 | | | -1.49 | 0.140 |
| 2 weeks | 90.72±5.07 | 4.72±0.04 | 4.94 | 90.56±6.89 | 6.58±0.64 | 6.77 | 0.13 | 0.895 |
| 4 weeks | 86.88±4.76 | 8.56±0.34 | 8.96 | 85.84±5.89 | 11.3±0.36 | 11.63 | 0.97 | 0.334 |
| 8 weeks | 83.88±4.83 | 11.56±0.3 | 12.11 | 82.64±4.97 | 14.5±1.28 | 14.92 | 1.27 | 0.209 |
| 12 weeks | 82.28±5.40 | 13.16±0.3 | 13.78 | 79.08±4.98 | 18.06±1.3 | 18.59 | 3.08 | 0.003 |
*Values are expressed as mean±SD (Standard deviation) p-value calculated by Student t-test (unpaired t test).
Mean DBP before ramipril monotherapy was 95.44±5.11mmHg and after treatment reduced to 90.72±5.07 mmHg, 86.88±4.76 mmHg, 83.88±4.83 mmHg and 82.28±5.46 mmHg after two, four, eight and 12 weeks respectively. The mean DBP before ramipril and torsemide treatment was 97.14±6.25 mmHg and after FDC therapy reduced to 90.56±6.89, 85.84±5.89, 82.64±4.97 and 79.08±4.98 mmHg after two, four, eight and 12 weeks respectively. In FDC, the reduction was found to be statistically significant than monotherapy only after 12th week (p<0.01) [Table/Fig-3].
Laboratory Investigations in Group A and Group B also Showed Some Significant Findings
Renal function tests in both the treatment groups: There was statistically significant difference in Blood urea (p <0.01) in both the groups and S. Creatinine (p <0.01) in Group A only at the end of 12 weeks as compared to baseline. [Table/Fig-4,5].
Lab Investigations Of Group A (n= 50).
| Parameters | 0 week | 4 week | 8 week | 12 week |
|---|
| Blood urea (mg/dL) | 26.76±4.91 | 26.84±4.88 | 26.12±4.77* | 26.16±4.96* |
| S. Creatinine (mg/dL) | 0.855±0.13 | 0.856±0.13 | 0.8±0.12* | 0.81±0.14* |
| S. Sodium (meq/L) | 140.51±4.85 | 140.34±4.82 | 138.44±4.81* | 138.12±5.00* |
| S. Potassium (meq/L) | 4.21±0.39 | 4.19±0.4 | 4.22±0.39 | 4.22±0.69 |
| S. Chloride (meq/L) | 104.06±3.99 | 103.22±3.93* | 101.9±4.27* | 101.3±4.32* |
| S. Cholesterol (mg/dL) | 191.9±39.32 | 188.72±39.92 | 180.58±34.61* | 176.96±34.81* |
| S. Triglycerides (mg/dL) | 181.62±75.75 | 178.84±70.77 | 172.06±64.27 | 170.16±63.78* |
| LDL- Cholesterol (mg/dL) | 130.996±45.94 | 127.364±44.96 | 122.52±44.88* | 118.716±45.00* |
| HDL- Cholesterol (mg/dL) | 44.02±7.52 | 43.94±7.27 | 44.26±7.22 | 44.36±7.76 |
| AST (IU/L) | 28.54±6.46 | 28.38±6.33 | 28.34±6.21 | 28.2±6.02 |
| ALT (IU/L) | 27.56±6.13 | 27.42±5.89 | 27.26±5.78 | 27.18±5.75 |
| BMI (Kg/m2) | 28.57±6.17 | 28.57±6.17 | 28.14±6.06* | 28.53±5.99* |
| Body weight (Kg) | 73.62±15.39 | 73.62±15.39 | 73.14±15.20* | 73.02±15.06* |
Values are expressed as mean±SD (Standard deviation)
*p < 0.01: highly significant p-value calculated by Anova test
Serum electrolytes in both the treatment groups: Statistically significant reduction in values of S. sodium (p<0.01) and chloride (p<0.01) was observed at 12th week as compared to baseline values in both the groups. Potassium showed a significant reduction in Group B only [Table/Fig-4,5].
Lab. Investigations of Group B (n=50)
| Parameters | 0 weeks | 4 weeks | 8 weeks | 12 weeks |
|---|
| Blood urea (mg/dL) | 25.24±5.70 | 25.26±5.66 | 24.94±5.58* | 24.74±5.56* |
| S. Creatinine (mg/dL) | 0.87±0.10 | 0.88±0.10 | 0.87±0.09 | 0.86±0.10 |
| S. Sodium (meq/L) | 141.46±5.23 | 141.18±4.97 | 140.18±4.89* | 139.82±5.01* |
| S. Potassium (meq/L) | 4.36±0.38 | 4.35±0.38 | 4.33±0.39 | 4.28±0.38* |
| S. Chloride (meq/L) | 103.21±4.76 | 102.84±4.67 | 102.1±4.45* | 101.66±4.56* |
| S. Cholesterol (mg/dL) | 197.00±39.59 | 189.76±34.70* | 182.74±31.88* | 175.7±28.01* |
| S. Triglycerides (mg/dL) | 202.82±66.61 | 195.32±62.50* | 187.68±58.61* | 179.94±51.98* |
| LDL- Cholesterol (mg/dL) | 131.73±34.50 | 128.14±32.52* | 124.4±31.35* | 120.068±30.63* |
| HDL- Cholesterol (mg/dL) | 44.94±6.61 | 45.19±6.47 | 45.46±6.36 | 46.32±6.27* |
| AST (IU/L) | 26.65±5.45 | 26.6±5.42 | 26.3±5.27 | 26.26±5.22 |
| ALT (IU/L) | 26.24±5.87 | 26.26±5.72 | 26.28±5.65 | 26.22±5.60 |
| BMI (kg/m2) | 28.51±5.34 | 28.51±5.34 | 28.45±5.37 | 28.24±5.17* |
| Body Weight (Kg) | 73.16±14.26 | 73.16±14.26 | 73±14.31 | 72.44±13.89* |
Values are expressed as mean±SD (Standard deviation)
*p < 0.01: highly significant p-value calculated by Anova test
Lipid profile in both the treatment groups: In group A, at the end of 12th week, statistically significant decrease in S. Cholesterol, S. triglycerides, LDL Cholesterol (p<0.01) but no rise in HDL Cholesterol (p >0.05) was observed. On the other hand, in group B, statistically significant reduction in S. cholesterol levels (p <0.01), S. triglycerides (p <.01), LDL cholesterol (p <0.01) and rise in HDL Cholesterol (p <0.01) was observed [Table/Fig-4,5].
Body Mass Index (kg/m2) and body weight in both the treatment groups: A mean baseline value of BMI in group A was 28.57±6.17 and in group B 28.51±5.34 kg/m2 thereby, indicating that the patients were overweight. On comparing the baseline and end of 12th week values, statistically significant reduction in BMI in group A (p <0.01) and Group B (p <0.01) was observed. Significant weight reduction was found in both the groups at the end of treatment as compared to baseline values (p <0.01) [Table/Fig-4,5].
In safety analysis during the entire study period, all the patients were closely monitored for any adverse effects as per the adverse effect checklist and by voluntary reporting by the patients. In Group A, 6 (12%) patients had reported side effects viz., (1) nausea, (2) headache, (3) dry cough whereas in Group B, 9 patients (18%) had reported side effects viz., (4) headache, (5) increased frequency of urine, (6) asthenia. Side effects were mild and there was no other serious adverse effects reported in either of the treatment groups. Further, none of the patients withdrew from the study due to the same.
Discussion
In ramipril monotherapy group (Group A), 88 percent achieved goal BP (<140/90 mmHg) while with ramipril torsemide FDC group (Group B), 98 percent achieved goal BP. Ramipril/torsemide FDC was associated with significantly reduced ambulatory and office-measured BP as compared to ramipril monotherapy to achieve the goal BP. The goal BP was achieved with combination therapy in 4 weeks as compared to monotherapy in 8 weeks.
Diuretics augment the antihypertensive response to ACE inhibitor by rendering the patient’s BP renin dependent. Intravenous torsemide has 100% bioavailability and oral has 91% bioavailability. Torsemide has three times longer half life than furosemide (3 hours vs 0.8 hrs). Torsemide is eliminated via hepatic route (73%), while furosemide is excreted through kidneys (83%). In patients with renal insufficiency, accumulation of torsemide does not occur. They enhance the efficacy of all other antihypertensive drugs mainly ACE inhibitors [6]. An appropriate combination of antihypertensive drugs can produce beneficial effects on blood pressure, adverse reactions and hemodynamic effects [7]. The introduction of an ACE inhibitor allows the dose of diuretic to be lowered [9].
The patients on ramipril had an expected BP reduction that was similar to other studies [10-13]. In the present study, 88 percent Group A patients achieved goal BP (i.e. <140/90 mmHg) which was consistent with the study by Zidek W et al., [14]. A comparative study undertaken in India, comparing the efficacy and tolerability of telmisartan and ramipril has shown no significant difference in the reduction of BP till the end of treatment. BP was measured at the same time interval as in our study i.e., at baseline, 2nd, 4th, 8th and 12th week. In ramipril treated group, SBP and DBP reduction was compared to our study at the end of 12 weeks. The difference in results could be due to the fact that more than 65 years aged patients were excluded from their study and higher dose of ramipril (10 mg) was used [15].
A study by White WB et al., reported greater reduction in BP in combination therapy (ramipril and hydrochlorthiazide) as compared to ramipril alone and hydrochlorthiazide alone. Almost same results were observed in the present study although, the combination therapy has lowered DBP to a greater extent probably due to the fact that patients with DBP >110 mmHg were not included in our study. Only 54 percent cases achieved target BP in their study whereas in our study 98 percent achieved BP control [16]. The results of the present study are consistent with PROGRESS study (Perindopril Protection Against Recurrent Stroke Study) [17].
Published literature reported that torsemide, at a low dose, once a day, induces a decrease in arterial blood pressure greater than placebo and which is similar in magnitude to that of Hydrochlorthiazide or indapamide [18-20]. Further, torsemide is equally effective as thiazide and related diuretic compounds. Therefore, in essential hypertension treatment, low dose of torsemide could be an alternative to thiazides [21,22].
Effect of drugs on primary efficacy parameters were assessed in both the study groups, ramipril either as monotherapy or in combination with torsemide. As per literature, diuretics are used as antihypertensive drugs in different doses. Although, thiazide is first choice drug as per accepted guidelines, literature mentions that at dose 12.5-25 mg it shows several side effects, which do not occur at sub-diuretic dose of torsemide (2.5-5 mg). This drug compares favourably with hydrochlorthiazide and indapamide. Torsemide exhibits favourable side effect profile, particularly because it does not endanger hypokalemia, increase in blood glucose or lipid levels and can be used as an alternative to thiazide [18,19,22].
Strengths of the Study: The present study was done with the intention to treat Stage I and II hypertensive patients and attempts to compare antihypertensive efficacy and incidence of adverse drug reactions between group containing ACE inhibitor alone (Ramipril) and combination of ACE inhibitor with loop diuretic (Ramipril and Torsemide). Further, it was a short duration study (12 weeks) and no harmful effects of drugs were observed during that time period. The participants responded well as per efficacy and safety in both the therapy groups with perceived improvements of their Quality of Life (QoL).
Cost effectiveness: In our study, it was our additional observation that with a marginal addition of price at the consumer end in the hypertensive patients in our study population was grossly benefitted without addition of adverse drug reactions as follows: The cost of monotherapy with one tablet of Ramipril 5 mg was Rs. 10 daily (i.e., once a day cost), while cost of combination therapy (in our study) was Rs. 11.30 (i.e., once a day cost) i.e., One tablet of Ramipril 5 mg (Rs. 10) plus One tablet Torsemide 5 mg (Rs. 1.30) daily.
Limitation
Firstly, this was an open labelled study without any blinding. Secondly, the patients were followed up for 12 weeks only. Therefore, long-term efficacy and safety could not be delineated. Also, this was only a revelation of a single centre with limited external validity. Moreover, groups were not subdivided according to stage of hypertension. Fifty patients in each group were enrolled with stage I and Stage II hypertension to observe the response of drug therapy in general, (i.e., on BP reduction in both groups with monotherapy and combination therapy) and target was to achieve the goal BP in less time period so that hypertension related complications could be delayed/reversed or prevented as early as possible by improving the quality of life of patients.
Future Perspectives of this Study: In the future projects, on comparable field of research, the basis for synergy with Torsemide and ACE inhibitors will be considered in light of other molecules like hydrochlorthiazide or indapamide to sensitise our fraternity to identify and fill up the lacunae regarding newer antihypertensive prescribing practices.
Conclusion
To sum up, this study compared the efficacy of ramipril with torsemide FDC with ramipril monotherapy among newly diagnosed hypertensives. Although, both the regimens were well tolerated but FDC treatment groups showed significant fall in systolic blood pressure after four weeks and diastolic blood pressure after 12 weeks compared to the monotherapy. This study suggests that torsemide in combination with ramipril could be a promising agent in patients with stage I and stage II hypertension as compared to ramipril monotherapy. Potential advantages of torsemide and ramipril combination include its apparently better efficacy, tolerability, safety than ramipril alone as monotherapy.
*Values are expressed as mean±SD (Standard deviation) p-value calculated by Student t-test (unpaired t test).