Calcinosis cutis was first described by Virchow in 1855, and in 1883 Lewinsky first described scrotal calcinosis as a subtype [1,2]. ISC is characterized by solitary or multiple intradermal nodules in the presence of normal levels of calcium and phosphate. These slow-growing nodules appear early in life, gradually increase in size and number and may break down with release of chalky contents [3].
Dystrophic calcinosis cutis is the most common variant with no sex or race predilection, but is more common in people of South African origin. ISC is a very uncommon occurrence and hence, specific incidence and frequency data are not available [4].
This study was undertaken with an aim to study the clinical, cytological and histopathological aspect of this rare pathology, which has an obscure pathogenesis and is often misdiagnosed clinically. Karnataka ranks seventh in terms of cement production in the country with a production of around 11 million tons per annum, with some of the largest cement factories concentrated in North Karnataka [5]. An attempt was also made to identify a possible correlation between ISC and an increase in calcium compounds in the water due to cement dust pollution in North Karnataka region.
Materials and Methods
In this retrospective study, twenty previously reported cases of idiopathic calcinosis cutis in MR Medical College, Kalaburagi, during a ten year period from 2007 to 2016 were included. Institutional ethical committee clearance was taken.
All cases with scrotal calcinosis and normal serum calcium and phosphorus levels were included in the study, but patients with a raised serum calcium level or some systemic metabolic diseases were excluded. A physical examination of the scrotum to note the consistency, size, shape, number, adhesions to scrotal skin, and draining sinuses (if any) was performed. A detailed history was taken to know of any relevant trauma to the scrotum, previous infections, systemic symptoms, metabolic disorders, similar familial complains and occupation. A complete work-up comprising of CBC, serum and urine calcium and phosphorus, fasting and post prandial blood sugar and USG was done. FNAC with a 22 gauge needle attached to a 10 ml syringe was done in six cases that were referred to cytology by the surgeons. Surgical excision of the lesion was followed by histopathological examination in all the cases.
Results
Among the twenty cases, fourteen showed grey brown, hard, non-tender, solitary nodular scrotal swellings, while the remaining six presented with multiple varying sized nodules on the scrotum. The diameter of the largest nodule was measured which ranged from 0.5 cm to 3.5 cm (mean 1.97 cm). The swellings were easily movable beneath the scrotal skin and the testes were not involved in any of the twenty cases [Table/Fig-1].
Multiple nodules of variable sizes, firm to hard in consistency.

The patient’s age ranged from 19 to 65 years with a mean of 37.2±11.4 years. The duration of swelling varied from two to 24 months, mean of 8.8±5.2 months.
The most common occupation in the present study was farmers (7/20), followed by patients with a sedentary lifestyle (5/20), drivers (4/20), and businessmen (2/20). Two elderly people were retired government employees.
A history of chalky white discharge from the swelling was seen in four cases. Eleven cases complained of a slowly growing swelling and it was painless in all the cases. There was no history of trauma, infections, connective tissue diseases, or any history of family member having a similar complaint.
The serum calcium and phosphorus levels were within normal range in all cases, and, both fasting and post prandial glucose were within the normal limits.
The most common clinical presentation was scrotal swelling in seventeen cases, two cases presented with right inguino-scrotal swelling and one with a non-healing ulcer over the scrotal skin. Most common clinical diagnosis was sebaceous cyst (11/20) followed by epidermal inclusion cyst (6/18).
Three cases had associated findings, viz., two cases presented with right sided inguino-scrotal swelling and a clinical diagnosis of right sided inguinal hernia was made, while, one case presented with a non-healing ulcer over the scrotum with left side haematocele, which were confirmed on USG. A review of other systems revealed no abnormal findings.
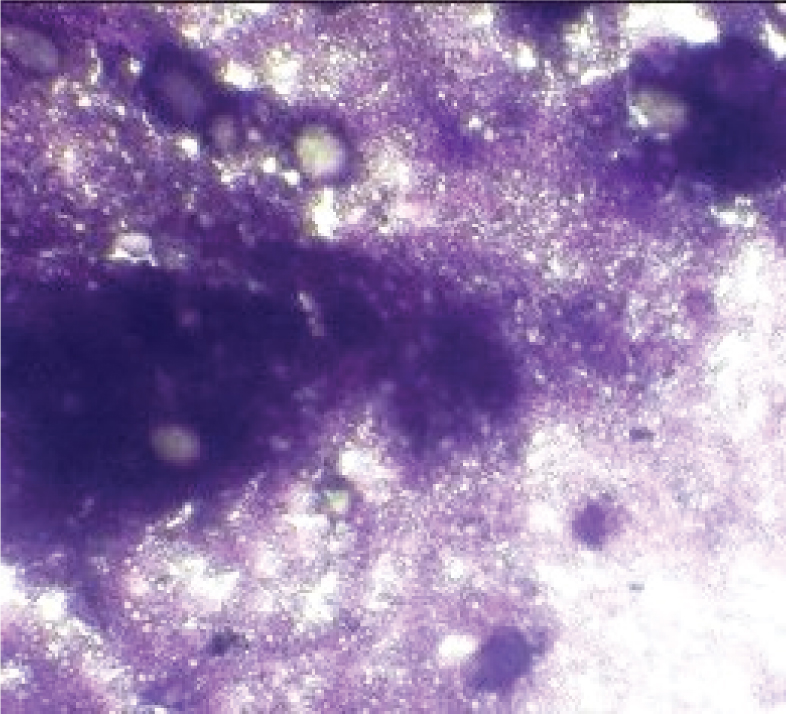
Fine Needle Aspiration Cytology (FNAC) was performed in six cases. The needle penetrated with a gritty sensation and yielded a chalky white granular material. The resultant smears were hypocellular, with amorphous granular, refractile crystals and occasional macrophages in a haemorrhagic background [Table/Fig-2].
FNAC revealing amorphous granular calcified material and calcium crystals (Giemsa, 100X).
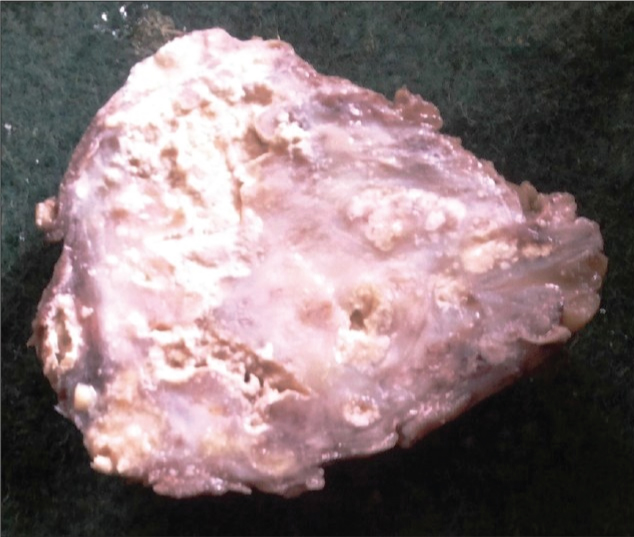
Grossly, the specimens consisted of scrotal skin with firm to hard nodules, whose cut surface revealed, chalky white nodules [Table/Fig-3].
Cut section revealing chalky white areas.
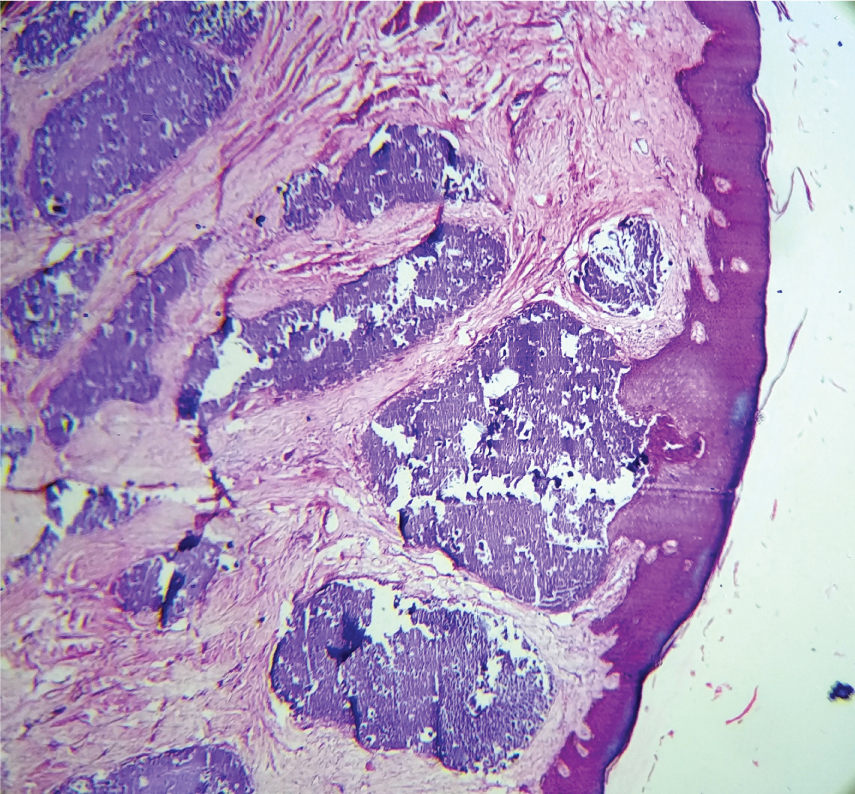
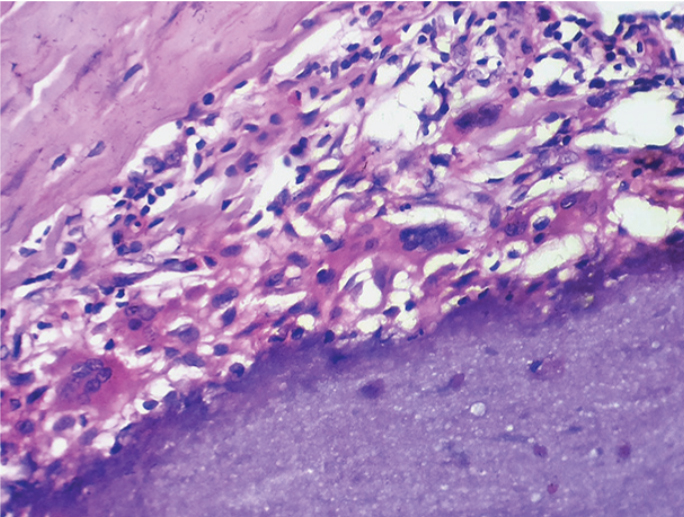
Microscopic examination revealed normal stratified squamous keratinised epithelium with prominent dermal nodules containing an amorphous, homogenous and granular basophilic material corresponding to calcium deposits. An epithelial lining surrounding the nodules was noted in three cases. These nodules were associated with a foreign body giant-cell reaction with scattered inflammatory infiltrates consisting primarily of lymphocytes [Table/Fig-4,5].
Amorphous basophilic masses seen in the dermis (H&E, 40X).
Foreign body giant cells with lymphocytes (H&E, 100X).
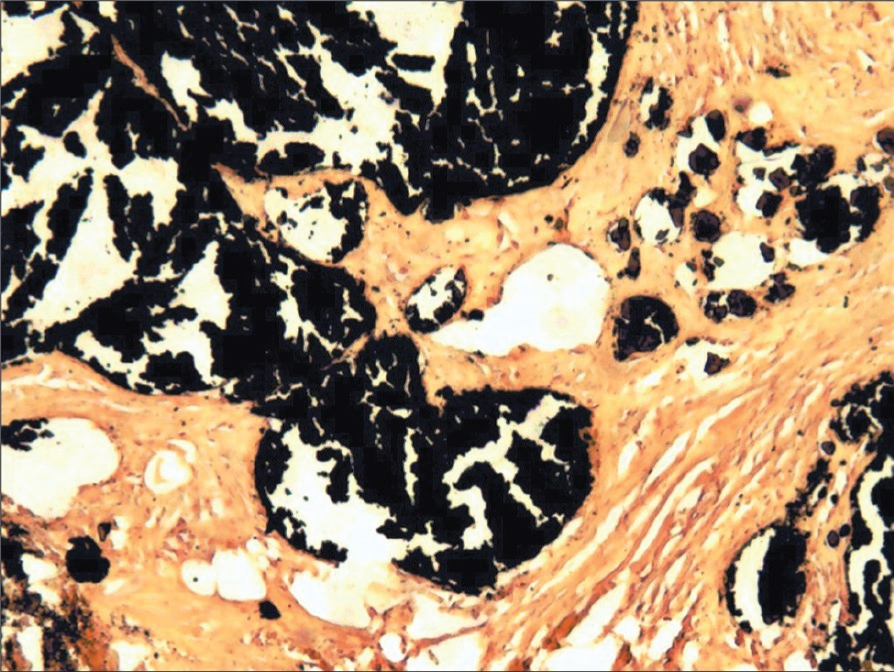
A definitive diagnosis is based on the histology and confirmed by the presence of von Kossa positive dermal deposits, which have also been noted in all the cases of our series [Table/Fig-6].
Black granular deposits of calcium within the dermis (von Kossa, 40X).
All cases underwent en-bloc surgical resection with primary closure and no recurrence was noted during the maximum follow up period of two years.
Discussion
Calcinosis cutis is a term used to describe a group of disorders in which circumscribed calcium deposits form in the dermis of the skin in various parts of the body. It is classified into four major types: metastatic, dystrophic, idiopathic, and subepidermal calcified nodule [2]. Idiopathic calcinosis cutis occurs in the absence of tissue injury or a systemic metabolic disorder and the calcification is localized to one area. A rare form is calcinosis cutis of the scrotum and penis. Idiopathic calcium deposits have also been described in the vulva, knee, neck and breast [6,7]. Idiopathic calcinosis of the scrotum or scrotal calcinosis consists of asymptomatic nodules of the scrotal skin which may sometimes form sinuses to discharge their chalky contents [2]. These asymptomatic and painless nodules usually appear during childhood or early adulthood and slowly increase in size over the years and may present as single or multiple firm lesions [8,9].
The pathogenesis of scrotal calcinosis still remains unclear and is somewhat controversial. A number of histopathologic mechanisms have been put forth in the formation of scrotal calcinosis. The main dispute is whether the calcium is deposited at the site of preexisting structures; including epidermal cysts, calcification of eccrine sweat ducts or degenerated dartoic muscle or whether the calcified nodules are truly idiopathic [3,8].
In the dystrophic form of calcinosis cutis there is a local environmental niche, possibly due to tissue injury, which favours calcium deposits rather than its increased plasma levels. It may be observed in connective tissue diseases like scleroderma, dermatomyositis, Systemic Lupus Erythematosus (SLE) and secondary to trauma and inflammation [2].
In a study, Swinehart and Golitz examined numerous scrotal nodules, and concluded that ISC represents the end stage of dystrophic calcification of epidermal cyst in the scrotal wall. They found that among the numerous scrotal nodules, many were epidermal cysts which either showed rupture of their walls or calcification of the keratin contents such that eventually the cyst wall was completely destroyed and only dermal calcified masses remained [10].
One of the largest studies describing this entity was done by Dubey S et al., in which the authors studied 100 cases and concluded that true cyst wall and associated epidermoid cysts were more common in the smaller nodules, with the larger calcific masses being ‘naked’. It points toward a plausible explanation for the absence of a cyst wall in 40% cases published literature, because excision is generally performed in the late stage, when only the calcified masses remain. The histological photomicrographs in their study showed a continuous spectrum of changes ranging from intact epithelial cysts, calcified inflamed cysts with partial epithelial lining to ‘naked’ calcium deposits lying in the dermis which also supports the idea that ISC may be a consequence of dystrophic calcification of epidermal cysts which may progress in a sequence of inflammation, rupture, calcification and obliteration of the cyst wall [11].
Song DH et al., who studied 51 nodules found various types of cysts-epidermal, pilar, hybrid, and indeterminate cysts showing various degrees of calcification apart from the dermal calcium deposits and assumed that early lesions start out as cysts but, as they age, calcify and lose their cyst walls [12].
In our study, an epithelial lining surrounding the deposits were noted in three cases, which favours the theory that cyst wall may be present in smaller nodules or early lesions.
The findings in the study by Kelten EC et al., suggest that degenerated dartos muscle fibres where superimposed inflammatory reaction and calcium chelation triggered by mast cells are the mechanisms involved in scrotal calcinosis [13].
A large international series of 14 cases, by Chakravarti S et al., suggests an idiopathic origin for this condition, similar to most of the cases in this series [14].
The size and number of nodules may vary, from solitary lesions to multiple nodules with extensive involvement of the scrotum. Six cases in our study presented with multiple nodules. Cases with up to 300 and 220 nodules have been reported by Dombale VD et al., and Chakravarti S et al., respectively [7,14].
These lesions are usually asymptomatic. In the study by Dubey S et al., 72% patients came with concern of scrotal swellings; complaints of pruritus were found in 22%, a history of chalky discharge in 33% and ulceration in 3% cases [11]. In our study, 17/20 cases (85%) presented with scrotal swellings, 4/20 cases (20%) with a chalky white discharge and 1/20 (5%) with ulceration over the scrotum.
The most common differential diagnosis of idiopathic calcinosis of scrotum clinically are sebaceous cyst and epidermal inclusion cyst. Other less common conditions which should be considered clinically are cutaneous horn or other benign tumors such as, lipoma, fibroma, lymphangioma circumscriptum and angiokeratoma [15].
The most common clinical diagnosis in this series was sebaceous cyst. Associated findings in two cases were right inguinal hernia and one case with left haematocele.
Ancillary studies like USG and FNAC were performed in eight and six cases, respectively. USG study revealed soft tissue calcification along with other prominent findings of right sided inguinal hernia and left haematocele.
Very few case reports are available in literature with regards to the cytological features of idiopathic calcinosis cutis. In one report according to Dombale VD et al., the experience of performing fine needle aspiration was difficult, with a gritty sensation and the aspiration was granular [7]. Smears with granular amorphous and refractile material associated with lymphocytes histiocytes and foreign body giant cells suggest idiopathic scrotal calcinosis [11,16]. Absence of epithelial cells rule out calcified epidermal cysts on FNAC smears, which may support the idiopathic nature of the lesion [15].
The FNAC smears in this study consisted of calcified material with occasional foreign body giant cells which were suggestive but not diagnostic of idiopathic scrotal calcinosis.
Surgical excision of the affected part with scrotal reconstruction is curative and also allows for histopathological examination which is required for the confirmation of the diagnosis [11].
Relapses may be encountered in this condition. No relapses were seen in the six months of follow up in our study.
An attempt was made in the present study to find a possible correlation between ISC and an increase in calcium compounds in water due to cement dust pollution. Karnataka ranks seventh in terms of cement production in the country with a production of around 11 million tons per annum [5]. Cement dust, which is a mixture of calcium, potassium, aluminium, silicone and sodium and is produced and released into the surroundings by manufacturing units, is one of the most hazardous and dangerous environmental pollutants with drastic consequences.
Increase in calcium and calcium salts renders the regional ground water unfit for both drinking and irrigation purposes. The acceptable levels of total hardness in water according to World Health Organisation (WHO) and Indian Standard Institution (ISI) are 100 ppm and 300 ppm, respectively and that of calcium hardness is 75 ppm. Multiple water samples from various districts of North Karnataka, with close vicinity to cement factories have shown substantial increases in both calcium and total hardness [Table/Fig-7] [17,18].
Total and calcium hardness reference values.
| Total hardness (ppm) | Calcium hardness |
|---|
| WHO [18] | 100 | 75 |
| ISI [18] | 300 | 75 |
| North Karnataka [19] | 608-2736 (66 samples) | 202-380 (28 samples) |
In our study, most patients belong to suburban areas of Northern Karnataka where there is a reliance on groundwater as the principal source of drinking water.
The fact that most patients belonged to suburban areas of Northern Karnataka and the most common profession encountered in our study was farmers, which would increase their exposure to hard water used in irrigation as well, an increase in prevalence of this otherwise rare entity in this region may point towards a possible association with consumption of hard water, possibly due to pollution of water by cement dust.
Limitation
The limitation of the study was that it was carried out in a small population group of North Karnataka. There has been an increase in the number of cement factories in this region which could have contributed in an escalation of calcium content in the water. To substantiate our hypothesis that calcium levels in the ground water could be related to calcinosis cutis, similar studies need to be done in regions with high calcium in the ground water.
Conclusion
The present study of 20 cases with scrotal calcinosis spanning a period of 10 years is one of the fewer case series of this entity, which has usually been described in the form of case reports. ISC is characterized by a solitary or multiple, painless intradermal nodules in the presence of normal levels of calcium and phosphate and in the absence of any systemic metabolic disorder. The cases in this series support the theory that ISC are dystrophic calcifications of epithelial inclusion cysts.
The treatment of choice is surgical excision which was limited to the scrotal skin and has an excellent prognosis. Recurrence rates varied in different studies. Increased levels of calcium in water could have a favourable role in the occurrence of this otherwise rare entity, inspite of normal calcium levels in the body.