Adenomatoid tumours are hormone independent tumours of mesothelial origin. These are distinctive benign neoplasms usually localised in the epididymis in males and myometrium in females. They are uncommon and account for less than 5% of tumours in males and approximately 1% in females. Due to their rarity and distinct histomorphology, we present a case series of six adenomatoid tumours of which three were males and three were females, obtained over a period of five years at a tertiary hospital in South India. The diagnosis of this tumour in all the three women and in one of the male patients was incidental, and they underwent surgical procedure for other coexisting lesions. In two male patients swelling of the testis was present; however, the clinical diagnosis of both these patients was more sinister than a benign entity like adenomatoid tumour. The present series describe the histomorphological features of this entity and establish the unique histopathological findings of this tumour which is clinically subtle and is seldom recognised.
Adenomatoid tumours were first described in 1945 by Golden A and Ash J, as a small asymptomatic intrascrotal mass [1]. These are distinctive neoplasms described within both male and female genital tracts, although extragenital tumours have also been reported in various other sites. These rare benign tumours are seldom diagnosed clinically; hence it is important to recognise them by histopathology to avoid more sinister diagnosis and overtreatment. Moreover, histopathological diagnosis of these clinically subtle lesions requires a high index of suspicion for their diagnosis.
Case Series
A total of six cases of adenomatoid tumour were retrieved retrospectively from 2012 to 2017, from the records of Department of Pathology, Kasturba Medical College, Manipal, Karnataka, India. The clinicopathologic features of these cases are shown in [Table/Fig-1]. The mean age of presentation was 45 years in women and 60 years in men.
Clinicopathological features of adenomatoid tumours.
| Case No. | Age (years) | Sex | Clinical presentation | Location | Size (cms) | Diagnosis | Gross appearance | Common histologic pattern | Lymphoid aggregates |
|---|
| 1. | 45 | Female | Abdominal mass, bleeding per vaginum | Uterus | 3x2.5 | Ovarian cyst, fibroid uterus | Circumscribed and unencapsulated | Multiple cystic spaces and cords resembling vascular channels | Absent |
| 2. | 45 | Female | Abdominal mass | Uterus | 3x3 | Fibroid uterus | Circumscribed and unencapsulated | Absent |
| 3. | 60 | Male | Swelling and pain left scrotum | Left testis | 6x5 | Carcinoma testis | Circumscribed and encapsulated | Present |
| 4. | 59 | Male | Swelling and pain left scrotum | Left testis | 2.3x2 | Tuberculosis epididymis | Circumscribed and encapsulated | Present |
| 5. | 61 | Male | Known case of gastric carcinoma | Mesentery | 1.5x1 | Metastatic mesenteric deposit | Circumscribed and unencapsulated | Present |
| 6. | 50 | Female | Nullipara with fibroid uterus | Uterus | 2.5x2 | Fibroid uterus | Circumscribed and unencapsulated | Absent |
In all the female patients, the tumours were located in the myometrium and were an incidental finding in addition to leiomyoma. In males, lesions were located near the epididymis.
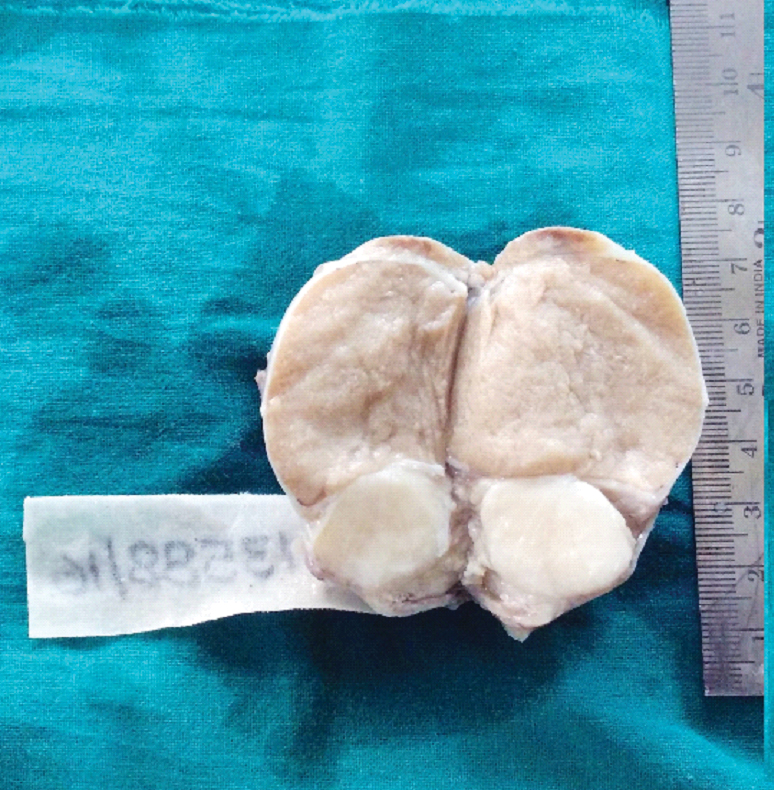
Circumscription was a common feature noted in all the six cases, with encapsulation being a feature seen in the paratesticular lesions [Table/Fig-2].
Well circumscribed grey white firm tumour near the epididymis with adjacent testicular parenchyma in a 59-year-old male patient (case 4).
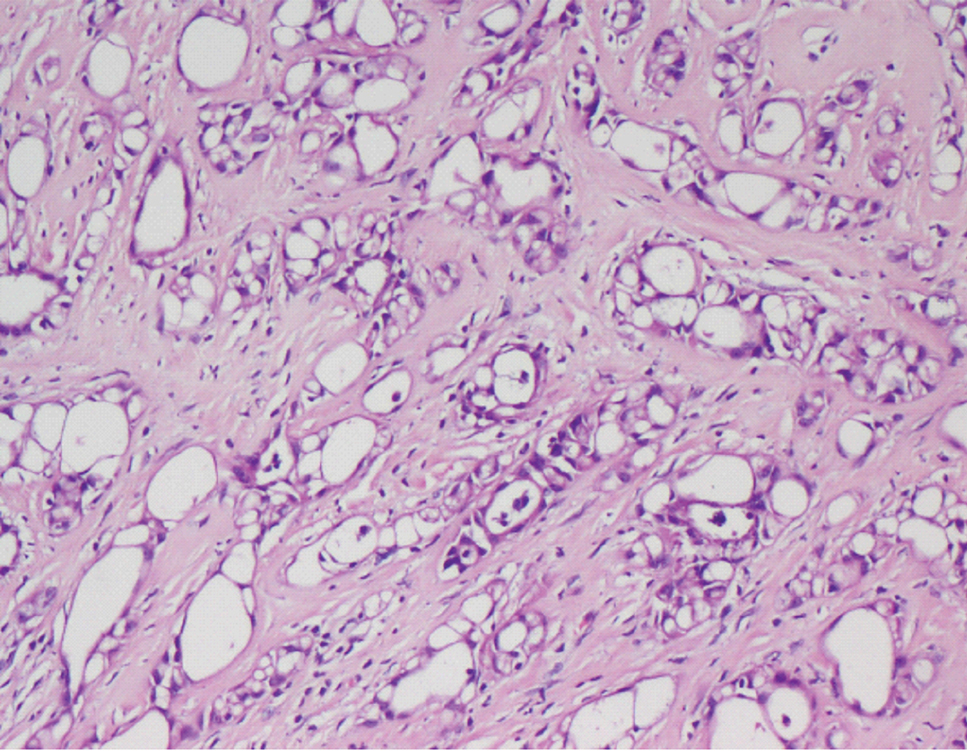
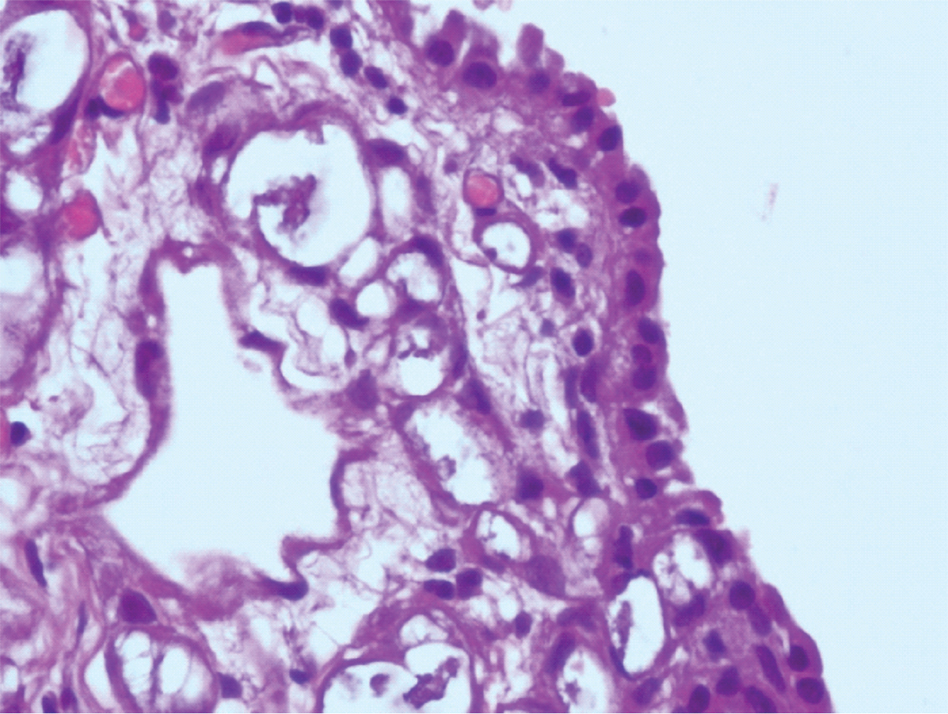
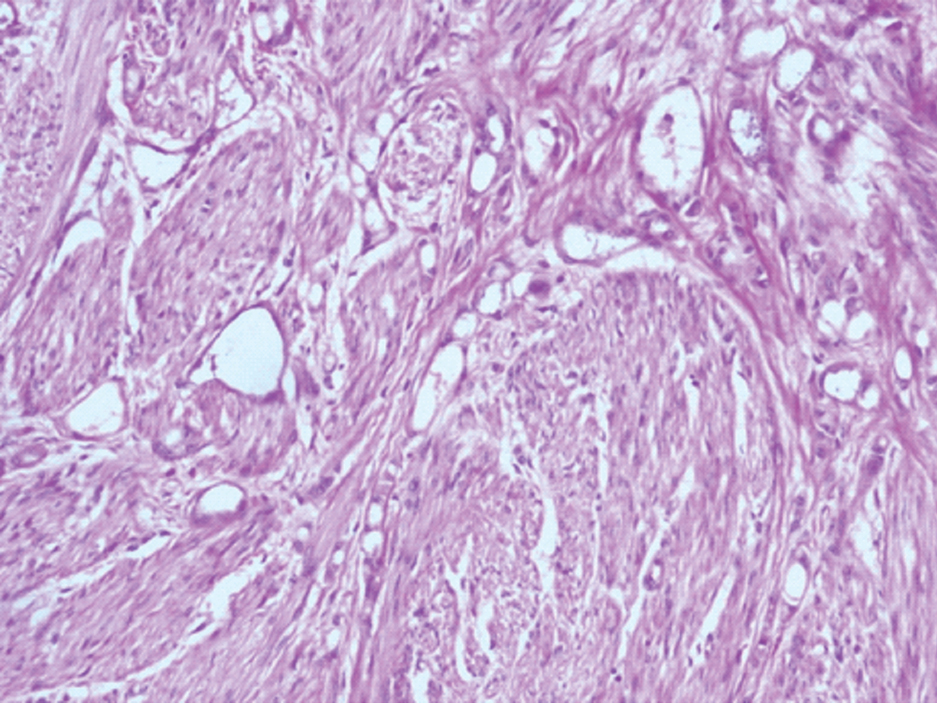
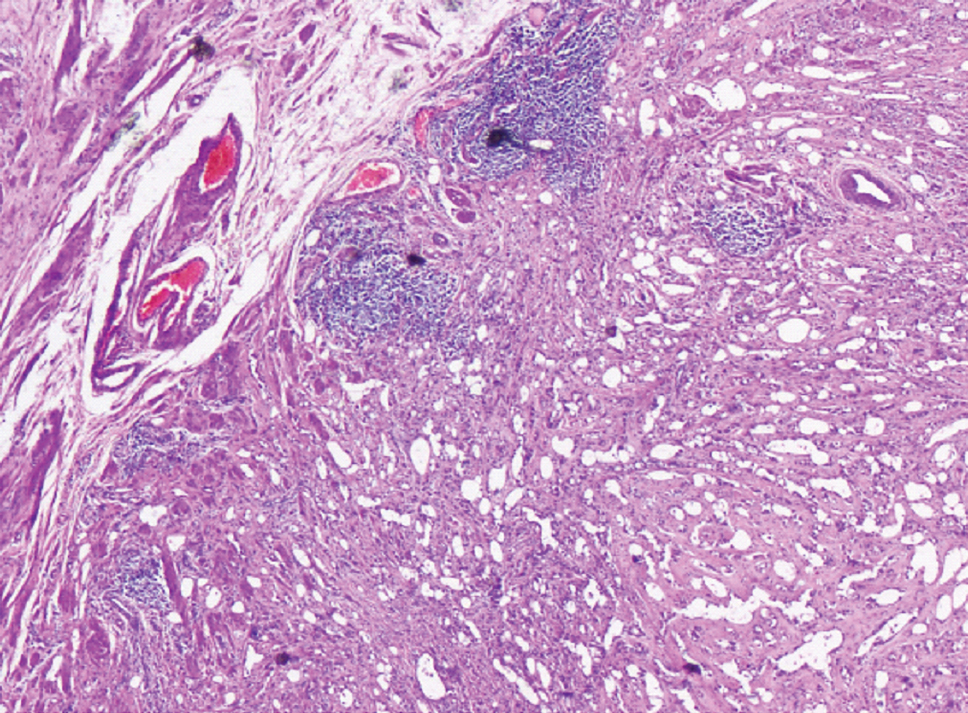
Microscopy was characterised by multiple cystic spaces and cords resembling vascular channels lined by flattened to cuboidal cells with vacuolated cytoplasm, vesicular nuclei and small nucleoli surrounded by a fibrous, focally hyalinised stroma [Table/Fig-3,4 and 5], with interspersed smooth muscle fibres [Table/Fig-5], being seen in the uterine lesions. Further, a peripheral ill formed rim of lymphoid aggregates [Table/Fig-6] was a feature seen only in males.
Case no.4-Adenomatoid tumour showing multiple cystic spaces and cords surrounded by a fibrous stroma (H&E, 4X).
Case no. 5-Adenomatoid tumour of mesentery with overlying mesothelial cells (H&E, 40X).
Case no. 2-Prominent smooth muscle bundles in a case of uterine adenomatoid tumour (H&E, 20X).
Case no. 4-Prominent lymphoid aggregates at the tumour periphery in a paratesticular adenomatoid tumour (H&E, 20X).
Treatment of all cases included complete excision of the tumour. On follow up (for a period of two years), no recurrence was noted. In some cases, the diagnosis of adenomatoid tumour was an incidental finding and was not a clinical diagnosis. However, the management as well as the outcome of these patients was not altered.
Discussion
Adenomatoid tumours are benign tumours of mesothelial origin that are most commonly seen in the genital systems of both males and females [2,3]. In men, they are the most common paratesticular tumours of middle aged patients; average age being 36 years [2,4]. These tumours are usually incidental findings [2,4]. Some patients may report mild discomfort or pain, mainly during exercise [2]. Common location of this tumour is in either pole of epididymis [2]. In women, these tumours are located in the myometrium or wall of fallopian tube where they are usually mistaken for leiomyoma [2]. Other sites include spermatic cord, prostate and ejaculatory duct [2]. Intratesticular adenomatoid tumours can arise in the tunica albuginea, tunica vaginalis and rete testis [2,4]. In women, ovarian hilar tumours have also been documented [2,4]. Unusual extragenital locations include adrenal gland [2,3], pleura [2,5], lymph node [2,6], umbilicus [7] and omentum [8] where these are incidental findings as occurred in our case No.5.
The histologic spectrum of these tumours includes adenoid, glandular, angiomatoid, solid, cystic or transitional patterns [2,4]. Eosinophilic mesothelial cells are seen arranged as solid cord as well as dilated tubules that may resemble endothelium [2]. A pathognomonic feature of these cells is cytoplasmic vacuolation with cytologic atypia [9]. It is also characterised by a peripheral eosinophilic and lymphocytic infiltrate [2,9,10]. Mitosis is absent, the stroma is fibrous but may contain smooth muscle component [2,9,11]. Gaping spaces with no evident lining, signifying a necrotic tubular component, and smaller spaces, representing ghost remnants of the typical vacuolar spaces, serve as diagnostic clues [2,9,10].
Various studies have documented that prominent lymphoid aggregates is a feature of male genital tract tumours [9]. A definite etiology to this gender difference is however uncertain, though a speculated cause is that the testis or epididymis is more prone to trauma when compared to uterus [2].
Another corroborative diagnostic feature in genital tract adenomatoid tumours is the presence of thread like bridging strands traversing tubular spaces [2]. This feature however has no gender predilection [2]. Less recognised morphological features include oncocytic change and ischaemia which can cause diagnostic difficulties [2,9,11]. Sometimes the prominent eosinophilic cytoplasmic appearance may mimic sex cord stromal tumours or other non epithelial neoplasms [2]. Other diagnostic pitfalls include the presence of infarction and prominent stromal hyalinisation which may warrant the use of immunohistochemical markers for definite diagnosis [2,3,6,12].
The differential diagnosis of this entity include adenocarcinoma of testis, histiocytoid hemangioma, malignant mesothelioma, yolk sac tumours, metastatic carcinoma of prostate, carcinoma of rete testis and infrequently inflammatory pseudotumour and pseudosarcomatous myofibroblastic proliferation [2,8].
Immunohistochemically, adenomatoid tumours are positive for markers such as CK (AE1/AE3), EMA, Cam 5.2, CK5/6, CK7, CD99, calretinin, vimentin, WT1, D2-40 [9,13]. The mesothelial origin of tumour is confirmed by calretinin [9,12,13]. They showed equally strong and diffuse immunoreactivity to both calretinin and D2-40 [13]. Due to the significant background staining with calretinin in many lesions of female genital tract, D2- 40 is of diagnostic value [13]. These tumours show negativity for factor VIII and CD 34, thus excluding vascular tumours. Absence of inhibin expression helps to eliminate adrenal cortical and sex cord stromal neoplasms [2,10,11,13].
Conclusion
Adenomatoid tumour is a benign, rare and a distinct clinical entity, the accurate characterisation of which requires a comprehensive clinicopathological approach, clinical history, gross and microscopic features, with immunohistochemical markers. This kind of an approach becomes particularly useful when variants of these lesions are encountered, especially at unusual sites. The importance of recognising this entity lies in the fact that these tumours are seldom recognised clinically and hence may lead to an incorrect and overtreatment of this benign entity. Moreover, it becomes extremely challenging for the pathologists as these tumours are almost always clinically subtle and may be masked by other clinically obvious lesions.
[1]. Golden A, Ash J, Adenomatoidtumors of the genital tractAm J Pathol 1945 21:63-79. [Google Scholar]
[2]. Sangoi AR, McKenney JK, Schwartz EJ, Rouse RV, Longacre TA, Adenomatoid tumours of the female and male genital tracts: A clinicopathological and immunohistochemical study of 44 casesModern Pathology 2009 22:1228-35. [Google Scholar]
[3]. Daly HE, Rao O, Palazzo F, Gudi M, A rare entity of an unusual site: adenomatoid tumour of the adrenal gland: A case report and review of the literaturePathology Resaerch International 2010 :01-04. [Google Scholar]
[4]. Klerk DP, Nime F, Adenomatoid tumours (mesothelioma) of testicular and paratesticular tissueUrology 1975 6:635-41. [Google Scholar]
[5]. Minato H, Nojima T, Kurose N, Kinoshita E, Adenomatoid tumour of the pleuraPathol Int 2009 59:567-71. [Google Scholar]
[6]. Isotalo PA, Nascimento AG, Trastek VF, Wold LE, Cheville JC, Extragenital adenomatoid tumour of a mediastinal lymph nodeMayo Clin Proc 2003 78:350-54. [Google Scholar]
[7]. Adem C, Schneider M, Hoang C, Pathologic quiz case: an unusual umbilical massArch Pathol Lab Med 2003 127:e303-04. [Google Scholar]
[8]. Hanrahan JB, A Combined papillary mesothelioma and adenomatoid tumour of the omentum. Report of a caseCancer 1963 16:1497-500. [Google Scholar]
[9]. Diffalha SA, Pambuccian SE, Farooq AV, Barkan GA, Intratesticular adenomatoid tumour: A case report and review of LiteratureHuman Pathology 2016 4:13-17. [Google Scholar]
[10]. Bolat F, Kocer NE, Bal N, Kucukgoz U, Adenomatoid tumour of the female genital tract: Report of three casesTurkish Journal of Pathology 2007 23:98-102. [Google Scholar]
[11]. Alvarez Maestro M, Tur Gonzalez R, Alonso Dorrego JM, Jesus De la Peña Barthel J, Nistal Martin De Serrano M, Adenomatoid Tumours of the epididymis and testicle:Report of 9 cases and bibliographic reviewArch Esp Urol 2009 62:137-41. [Google Scholar]
[12]. Skinnider BF, Young RH, Infarcted adenomatoid tumour: A report of five cases of a facet of a benign neoplasm that may cause diagnostic difficultyAm J Surg Pathol 2004 28:77-83. [Google Scholar]
[13]. Delahunt B, Eble JN, King D, Bethwaite PB, Nacey JN, Thornton A, Immunohistochemical evidence for mesothelial origin of paratesticular adenomatoid tumourHistopathology 2000 36:109-15. [Google Scholar]