Basidiobolomycosis - A Rare and Underdiagnosed Fungal Infection Mimicking Eosinophilic Colitis
Siddhant Vijay Mathurvaishya1, Navneet Tiwari2, Anuradha S Sekaran3, Guduru Venkat Rao4, Rebella Pradeep5
1 Registrar, Department of Surgical Gastroenterology, Asian Institute of Gastroenterology, Hyderabad, Telangana, India.
2 Consultant, Department of Surgical Gastroenterology, Asian Institute of Gastroenterology, Hyderabad, Telangana, India.
3 Head of Department, Department of Pathology, Asian Institute of Gastroenterology, Hyderabad, Telangana, India.
4 Head of Department, Department of Surgical Gastroenterology, Asian Institute of Gastroenterology, Hyderabad, Telangana, India.
5 Senior Consultant, Department of Surgical Gastroenterology, Asian Institute of Gastroenterology, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Siddhant Vijay Mathurvaishya, 6-3-661, Somajiguda, Hyderabad-500082, Telangana, India.
E-mail: mathur.siddhant@gmail.com
Basidiobolomycosis is a rare fungal disorder mostly restricted to the arid regions of US and the middle-eastern countries. We report an unusual case of this rare infection of the colon in a 45-year immunocompetent male with a rare fungus Basidiobolus ranarum managed successfully with surgery and antifungals. To the best of our knowledge, this is the first case of gastrointestinal infection with B. ranarum in an immunocompetent individual, reported from India.
Basidiobolus ranarum, Itraconazole, Splendore hoeppli
Case Report
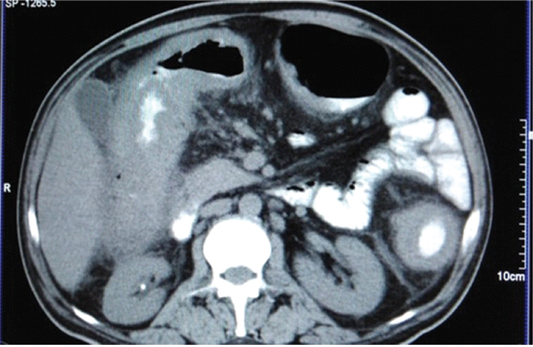
A 45-year-old male presented with history of abdominal pain, intermittent loose stools and anorexia for 6 months. On contrast-enhanced CT abdomen (done elsewhere), ascending colon and hepatic flexure showed asymmetrical thickening with adjacent fat stranding and enlarged lymph nodes [Table/Fig-1]. On colonoscopy an ulcero-nodular growth at the hepatic flexure was revealed and biopsy of the same was taken. Biopsy demonstrated granulomatous inflammation, which favoured tubercular aetiology.
CT showing thickening of transverse colon with prominent fat stranding of surrounding fat planes.
He was started on anti-tubercular medication for three months of four-drug intensive phase (isoniazid, rifampicin, pyrazinamide and ethambutol) and one month of continuation phase with two drugs (isoniazid and rifampicin) after which he stopped the medication, as he was not having any symptomatic improvement.
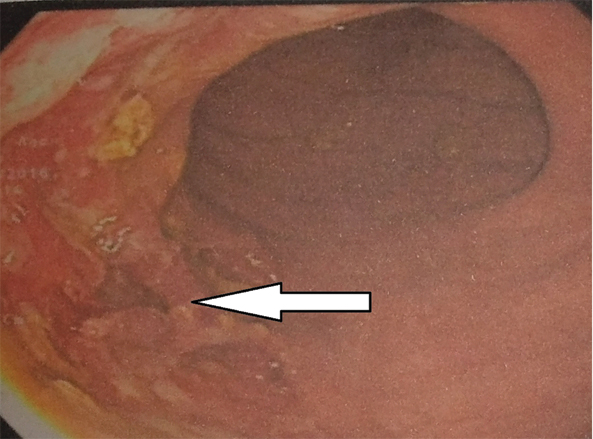
He then came to our institute with the same complaints. Blood investigations showed hemoglobin of 10.2 gm/dl and peripheral eosinophilia 25%. Serum IgE levels were significantly elevated (3635 IU/l), absolute eosinophil count was 1220 cells/mm3 while the lactate dehydrogenase level was normal. Repeat colonoscopy at our institute showed transverse colon stricture [Table/Fig-2], the biopsy of which showed acute on chronic inflammation with mucosal eosinophilia. Eosinophilic enteritis was suspected, upper gastrointestinal endoscopy with biopsy was done from oesophagus and duodenum, which were normal. Since patient was not having obstruction symptoms we differed surgery and started the patient on steroids and planned for repeat colonoscopy after three weeks to see the response to steroid therapy. Patient was re-admitted after three weeks with complaints of abdomen pain and distension, vomiting and loose stools. Colonoscopy, to assess response to therapy, revealed transverse colon stricture with large deep ulcers.
Colonoscopic picture showing colonic ulceration.
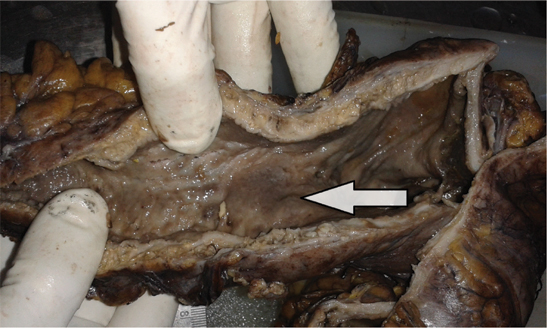
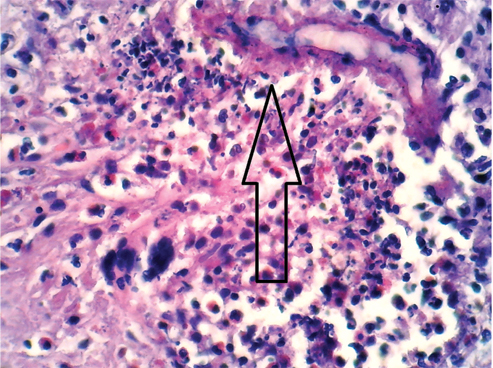
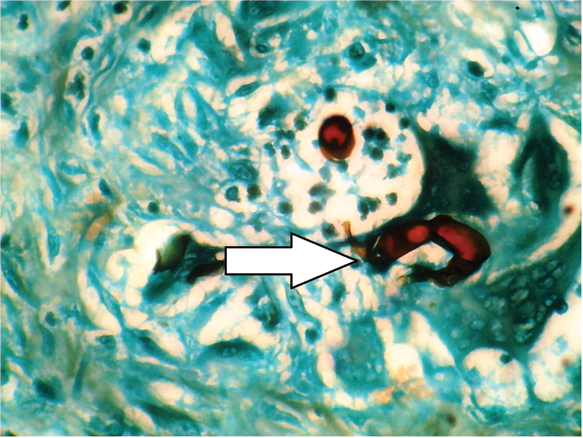
During the same admission patient developed partial obstruction and was taken for surgery. Whole colon was thick and inflamed with hard mass present in the proximal transverse colon [Table/Fig-3]. Patient underwent subtotal colectomy with ileorectal anastomosis. Histopathology report showed chronic suppurative granulomatous inflammation with foreign body giant cell reaction surrounding the broad, pauciseptate branching fungal hyphae [Table/Fig-4] and eosinophilic abscess. PAS and GMS stain revealed splendore hoeppli phenomenon which is suggestive of basidiobolomycosis infection [Table/Fig-5].
Thick wall of colon with ulcerated mucosa.
H&E stain showing Splendore Hoeppli phenomenon with eosonophilic abscess and granulomatous giant cell reaction (40x).
GMS stain showing broad, pauciseptate branching fungal hyphae (40x).
We advised patient to take oral itraconazole 200 mg daily for 6 months. On his follow up at 1, 2 and 4 months for outpatient visits, the patient remained well with no evidence of recurrence of disease.
Discussion
The fungal order Entomophthorales is part of class zygomycetes along with Mucorales. Mucorales affects mostly immunocompromised hosts while the Entomophthorales, which includes Basidiobolus has the capacity to affect immune competent individuals. Basidiobolus ranarum species of fungal order Entomophthorales is part of class zygomycetes and is mostly restricted to tropical areas. It has a ubiquitous presence in soil but also exists in decaying vegetable matter and the intestine of certain amphibians, reptiles, fishes and insectivorous bats. Route of infection for dermatological disease is through non-intact skin as caused by insect bites or following minor trauma to the skin. Gastrointestinal tract involvement is thought to occur from ingestion of soil or animal faeces or food contaminated by either specially in presence of ulcerations. Other known risk factors include prolonged use of Ranitidine, occupational involvement in digging owning a vegetable garden or a dog and longer duration of smoking [1]. Colon is the site most commonly involved followed by stomach and rarely retroperitoneum (3 cases) [1-3].
The infection is usually encountered in Africa, Middle-Eastern countries, tropical parts of USA and Mexico, Indonesia, affecting the trunk and limbs causing chronic subcutaneous infections [1]. However, cases of infection in animals in colder climates are known and human infections may be underreported due to low suspicion [4]. Cutaneous and systemic infections are reported in southern India but are still quite uncommon in northern India. Till 2015, 73 cases of visceral infection with Basidiobolus ranarum have been reported with only one from a country with cold environment (Netherland) [5].
A case of pulmonary basidiobolomycosis in a patient with adenocarcinoma lung [6] and a case of liver infection post liver transplant [7] have been reported from India. No other report of visceral involvement exists from India making ours the first case of visceral involvement in immunocompetent individual. A case of intestinal obstruction due to perineal infection by B. ranarum following episiotomy for vaginal delivery has been reported [8].
Common initial symptoms with Gastrointestinal Basidiobolomycosis (GIB) are abdominal pain and fever. Some patients additionally have constipation, diarrhea and gastrointestinal bleeding with concomitant high Erythrocyte Sedimentation Rate (ESR) and eosinophilia. There is often no identifiable risk factor and as the causative agent lies deep beneath the mucosa, mucosal biopsies may be non-representative. Victims are usually immunocompetent in contrast to other most common opportunistic fungal infections.
Radiological features mimic inflammatory bowel disease, tuberculosis or malignancy. Other differential diagnoses of GIB are sarcoidosis and eosinophilic colitis. Culture of the fungus is the gold standard for definite diagnosis and the disease has classical histopathological features like- Splendore hoeppli phenomenon making diagnosis feasible in patients with high suspicion of GIB. Recently, PCR has been developed for establishing diagnosis of GIB with high sensitivity and specificity [9].
The treatment is surgical resection of the affected part with pre and postoperative itraconazole for atleast six months. Early discontinuation of the antifungals can cause recurrence of the disease even after surgery with a mortality of 20% [10]. Recently cases of basidiobolomycosis with successful treatment with posaconazole and voriconazole after surgery were reported and should provide alternatives in resistant cases [11]. Though cases of successful treatment of extensive cutaneous involvement by antifungals have been described, yet surgery forms the backbone of management in GIB with antifungal treatment being of adjuvant benefit.
Conclusion
GIB is an emerging infection that leads to diagnostic confusion, morbidity and mortality. Its diagnosis requires a high index of suspicion and awareness. Treatment requires surgery, which is the backbone along with long-term antifungal therapy.
[1]. Lyon GM, Smilack JD, Komatsu KK, Pasha TM, Leighton JA, Guarner J, Gastrointestinal basidiobolomycosis in Arizona: clinical and epidemiological characteristics and review of the literatureClinical Infectious Diseases 2001 32(10):1448-55. [Google Scholar]
[2]. Finelli A, Rasul I, Keystone J, Bargman JM, Development of severe secondary hypertension in a patient with systemic entomophthoromycosisAmerican Journal of Kidney Diseases : The official Journal of the National Kidney Foundation 1997 29(4):620-23. [Google Scholar]
[3]. Nazir Z, Hasan R, Pervaiz S, Alam M, Moazam F, Invasive retroperitoneal infection due to Basidiobolus ranarum with response to potassium iodide--case report and review of the literatureAnnals of Tropical Paediatrics 1997 17(2):161-64. [Google Scholar]
[4]. Okada K, Amano S, Kawamura Y, Kagawa Y, Gastrointestinal basidiobolomycosis in a dogThe Journal of Veterinary Medical Science/The Japanese Society of Veterinary Science 2015 77(10):1311-13. [Google Scholar]
[5]. Mandhan P, Hassan KO, Samaan SM, Ali MJ, Visceral basidiobolomycosis: An overlooked infection in immunocompetent childrenAfrican Journal of Paediatric Surgery: AJPS 2015 12(3):193-96. [Google Scholar]
[6]. Deba Dulal, Biswal MSaPB, Pulmonary Basidiobolomycosis: An unusual presentation in a cancer patient: A case report and mini review of cases in IndiaInt J Curr Microbiol App Sci 2015 4(5):798-805. [Google Scholar]
[7]. Sethi P, Balakrishnan D, Surendran S, Mohamed ZU, Fulminant zygomycosis of graft liver following liver transplantationBMJ Case Reports 2016 2016:pii [Google Scholar]
[8]. Angeline Neetha, Radjou NR, Intestinal obstruction due to Basidiobolus ranarum: An unusual caseIndian Jour Medic Microbiol 2011 29(2):186-88. [Google Scholar]
[9]. Gomez-Munoz MT, Fernandez-Barredo S, Martinez-Diaz RA, Perez-Gracia MT, Ponce-Gordo F, Development of a specific polymerase chain reaction assay for the detection of BasidiobolusMycologia 2012 104(2):585-91. [Google Scholar]
[10]. Vikram HR, Smilack JD, Leighton JA, Crowell MD, Giovanni De Petris, Emergence of gastrointestinal basidiobolomycosis in the United States, With a review of worldwide casesClin Infect Dis 2012 54(12):1685-91. [Google Scholar]
[11]. Rose SR, Lindsley MD, Hurst SF, Paddock CD, Damodaran T, Bennett J, Gastrointestinal basidiobolomycosis treated with posaconazoleMedical Mycology Case Reports 2013 2:11-14. [Google Scholar]