Drug utilisation study is described as “the marketing, distribution, prescription and utilisation of drugs in the society, with special attention to the resulting medical, social and economic consequences” and has the main objective of facilitating the rational use of drugs which is very important in decision making for healthcare set ups [1]. Globally CKD is a major threat because of an increasing incidence, long term hospital stay, high cost of treatment and poor outcome associated with various complications and co-morbidities. CKD is an array of heterogeneous disorders affecting renal architecture and function as well [2]. The Kidney Disease Outcomes Quality Initiative (KDOQI) of the National Kidney Foundation defines CKD as kidney damage and/or a decreased glomerular filtration rate of less than 60 mL/min/1.73 m2 for three months or more [3]. Hypertension (HTN) has been reported in most of patients with CKD (stages III-V) [4,5].
According to the World Health Organization (WHO), global burden of kidney disease contributes to nearly 8,50,000 deaths/year along with urinary tract problems [6]. The number of renal failure patients, in need of dialysis and kidney transplantation has increased tremendously, due to which developing countries like India, with resource limited setting have a high mortality rate. Dialysis outcome study shows, uncontrolled serum concentration of phosphorous, calcium, potassium, sodium, urea and creatinine. Frequent adjustments in medications during dialysis days, unstable nature of the disease, restricted life styles and prescription of huge number of medications make these patients at high risk for developing adverse drug events due to drug-drug interactions, suboptimal action and non-adherence to treatment plans [7].
Exact therapeutic goals, frequent monitoring and dosage adjustment can hardly be attained without any lifestyle measure and substantial drug treatments because CKD is most frequently associated with hypertension, anaemia followed later on by acidosis, phosphocalcic disorders etc., [8]. Once the dialysis starts, the goals mainly focus on treating complications (anaemia and hyperparathyroidism) and to prevent morbidity and mortality associated with maintenance dialysis [9]. Hence, patients with CKD undergoing dialysis are comparable to diabetes or cardiac disease patients in regard to highest daily pill burden [10]. Hence, the aim of the present study was to analyse the drug utilisation patterns and AEs in CKD patients undergoing maintenance haemodialysis at a tertiary care hospital of eastern Odisha.
Materials and Methods
This prospective and observational study was undertaken in the Department of Pharmacology in collaboration with Department of Nephrology, S.C.B Medical College and Hospital, Cuttack, Odisha, India for a period of seven months from 1st June to 31st December, 2015 and was approved by Institutional Ethical Committee. Written informed consent of the participants or their relatives was taken prior to their inclusion into the study. AEs were also noted to know their incidence and how these can be managed as early as possible and prevented as well.
Study Criteria:
All patients of age group 18-80 years in CKD stage (IV,V), having eGFR between 4-28 mL/min/1.73m2 and undergoing maintenance haemodialysis were included in the study. CKD patients co-infected with HIV/Hepatitis B/Hepatitis C, renal transplantation/tumour/trauma, pregnant and lactating mothers were excluded from the study.
Sample Size Calculation:
About 10% population have some form of CKD [11,12].
Using EpiTools epidemiological calculators:
- Estimated true proportion was 0.1
- Confidence level was 0.95
- Desired precision (±) was 0.05
Population size for finite populations (total OPD and IPD patients in the hospital during our study period) was ≈ 7,20,000.
N=Z2 × P(1-P)/e2
Z=Value from standard normal distribution corresponding to desired confidence level (Z=1.96 for 95% CI).
P=expected true proportion.
e=desired precision (Half of desired CI width).
Calculated n=139.
Assuming that 10% may be lost to follow up (139+13=152).
As per the study criteria only CKD IV and V patients on maintenance haemodialysis were taken for the study and 37 patients were excluded (finally n=115).
Source of Data:
Requisite data were collected from hospital, laboratory records and matched with records of nursing faculties and with the discharged certificate for the treatment given.
Demographic, baseline, clinical and medication data and AE details were collected from patient’s case sheets as per a specially designed proforma. Then collected data were compiled on EXCEL sheet and analysed in a descriptive manner using percentage calculation Spearman’s correlation and multiple logistic regression using the trial version of SPSS v24.
Results
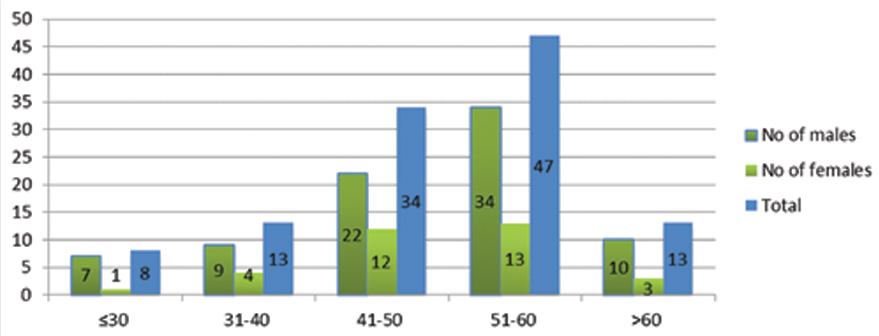
Amongst 115 enrolled CKD patients, 82 (71.3%) were male and 33 (28.7%) were female with mean age of 49.26±11.46 years. Of the total, 15.65% of the patients were in stage IV and 84.34% were in stage V of CKD. Co-morbidities associated with hypertension were seen in all 115 patients, anaemia in 90.43%, urinary tract infections in 63.47% and type-II diabetes mellitus with proteinuria in 45.21% patients [Table/Fig-1,2].
Demographic characteristics.
Baseline clinical and laboratory parameters.
| Parameters | Value |
|---|
| Haemoglobin (gm/dL) | 8.592±2.121 |
| Systolic blood pressure (mm of Hg) | 168.05 ±20.992 |
| Diastolic blood pressure (mm of Hg) | 94.57±7.631 |
| S. creatinine (mg/dL) | 8.547±3.728 |
| Plasma urea (mg/dL) | 117.57±30.526 |
| S. sodium (meq/dL) | 136.06±4.051 |
| S. potassium (meq/dL) | 5.005±0.779 |
| S. phosphorous (mg/dL) | 4.850±0.891 |
| Stages of CKD | |
| Stage IV | 97(84.34%) |
| Stage V | 18(15.65%) |
| Co-morbidities |
| Hypertension | 115(100%) |
| Anaemia | 104(90.43%) |
| U.T.I | 73(63.47%) |
| Type II DM & Proteinuria | 52(45.21%) |
| Glomerulonephritis | 11(9.56%) |
| COPD/Asthma, Hypothyroidism, Metabolic Encephalopathy, CAD | 6(5.21%) each |
| Polycystic Kidney Disease | 3(2.60%) |
| Anemia+Hypertension | 104(90.43%) |
| Anemia+Hypertension+Type II DM | 44(38.26%) |
| Anemia+Hypertension+Type II DM+U.T.I | 39(33.91%) |
| Anemia+Hypertension+U.T.I | 62(53.91%) |
| Anemia+Hypertension+Hyperlipidemia | 14(12.17%) |
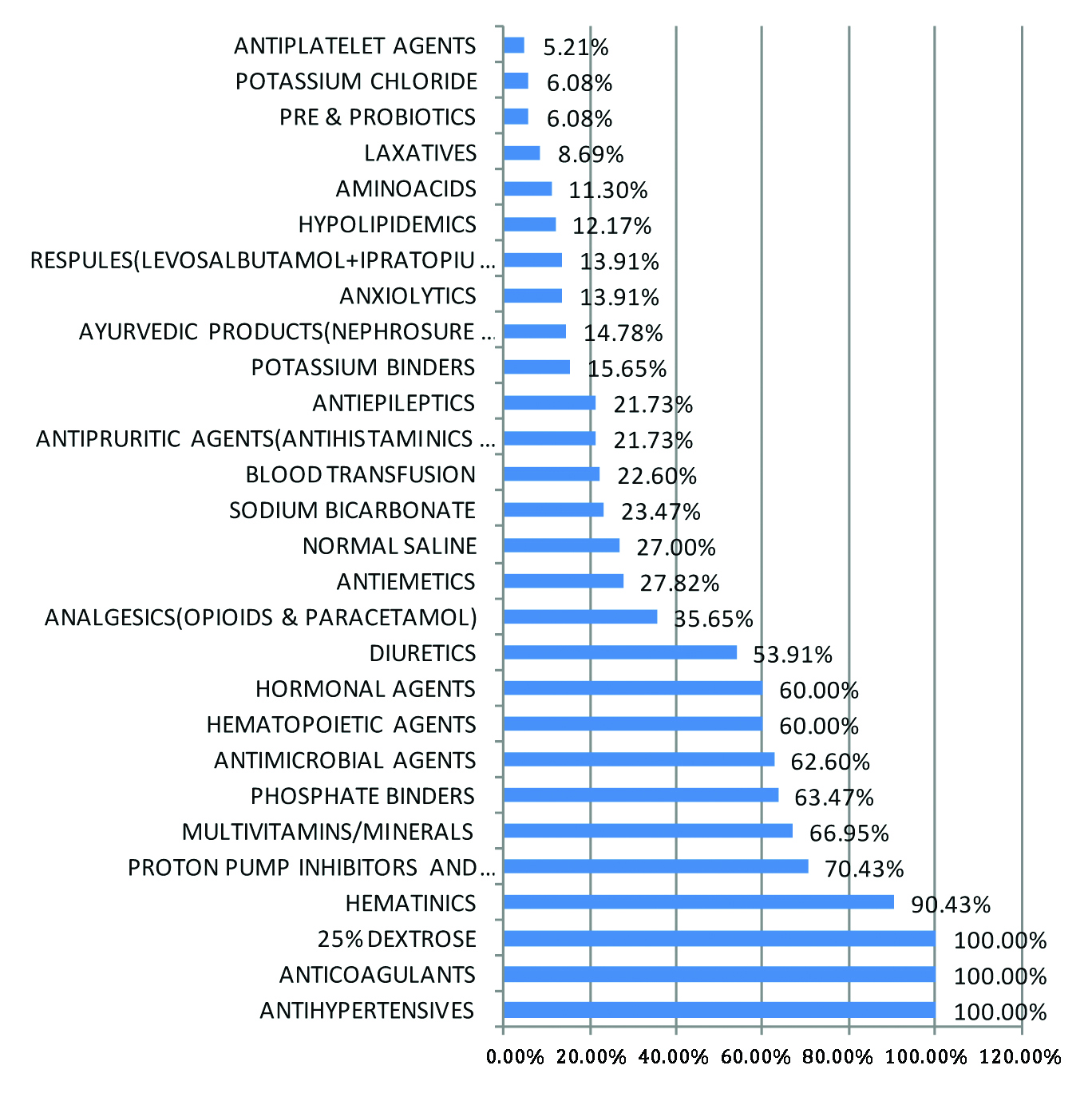
On analysis of bed head tickets it was observed that mean number of drugs per prescription was 12.8. Antihypertensives, 25% dextrose and heparin were prescribed to all patients followed by haematinics in 90.43% of the patients and proton pump inhibitors were prescribed in 70.43% of the patients. It was observed that 40.96% of the prescribed drugs were in generic name and 72.62% of the prescribed drugs were from NLEM [Table/Fig-3,4].
Analysis of prescriptions.
| Total number of prescriptions analysed | 115 |
| Number of different classes drugs prescribed | 48 |
| Total number of drugs prescribed in the beginning of the study during dialysis | 1472 |
| Average number of drugs per prescription during dialysis | 12.8 |
| Number of drugs prescribed by generic name | 603(40.96%) |
| Number of drugs prescribed from NLEM | 1069(72.62%) |
Specific groups of drugs (%) used among the total groups used (n=1472).
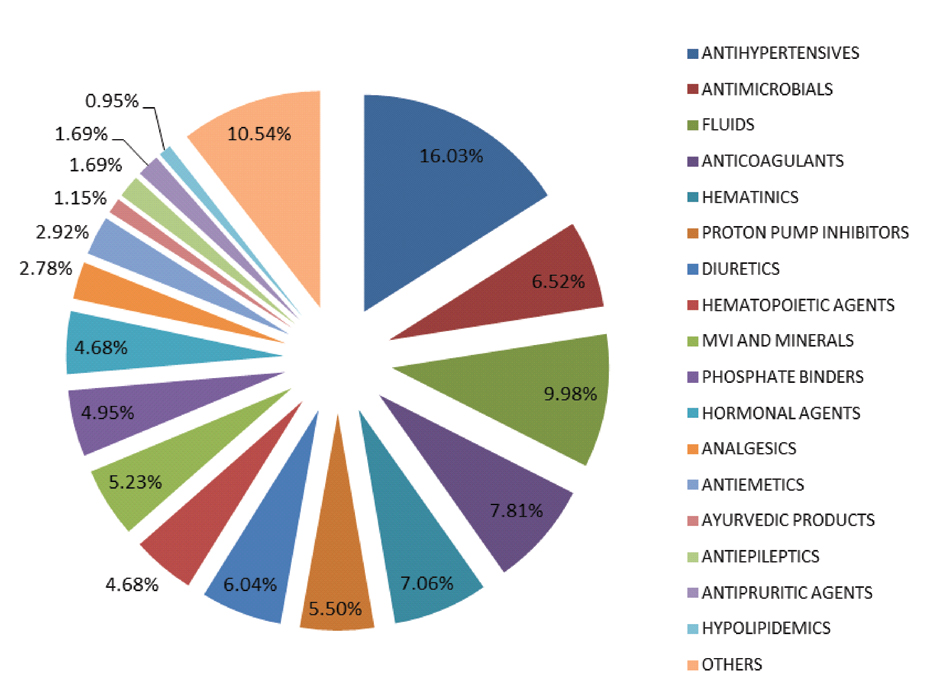
Antimicrobial agents were prescribed in 62.6% of the patients under study that included antimalarials, antiprotozoals, antifungals and antibacterials [Table/Fig-5]. Insulin was prescribed to all type II diabetes mellitus patients. Torsemide was the most frequently used diuretic followed by furosemide [Table/Fig-6].
Percentage of patients on selected medications/fluids (N=115).
Different drugs (%) used by study population.
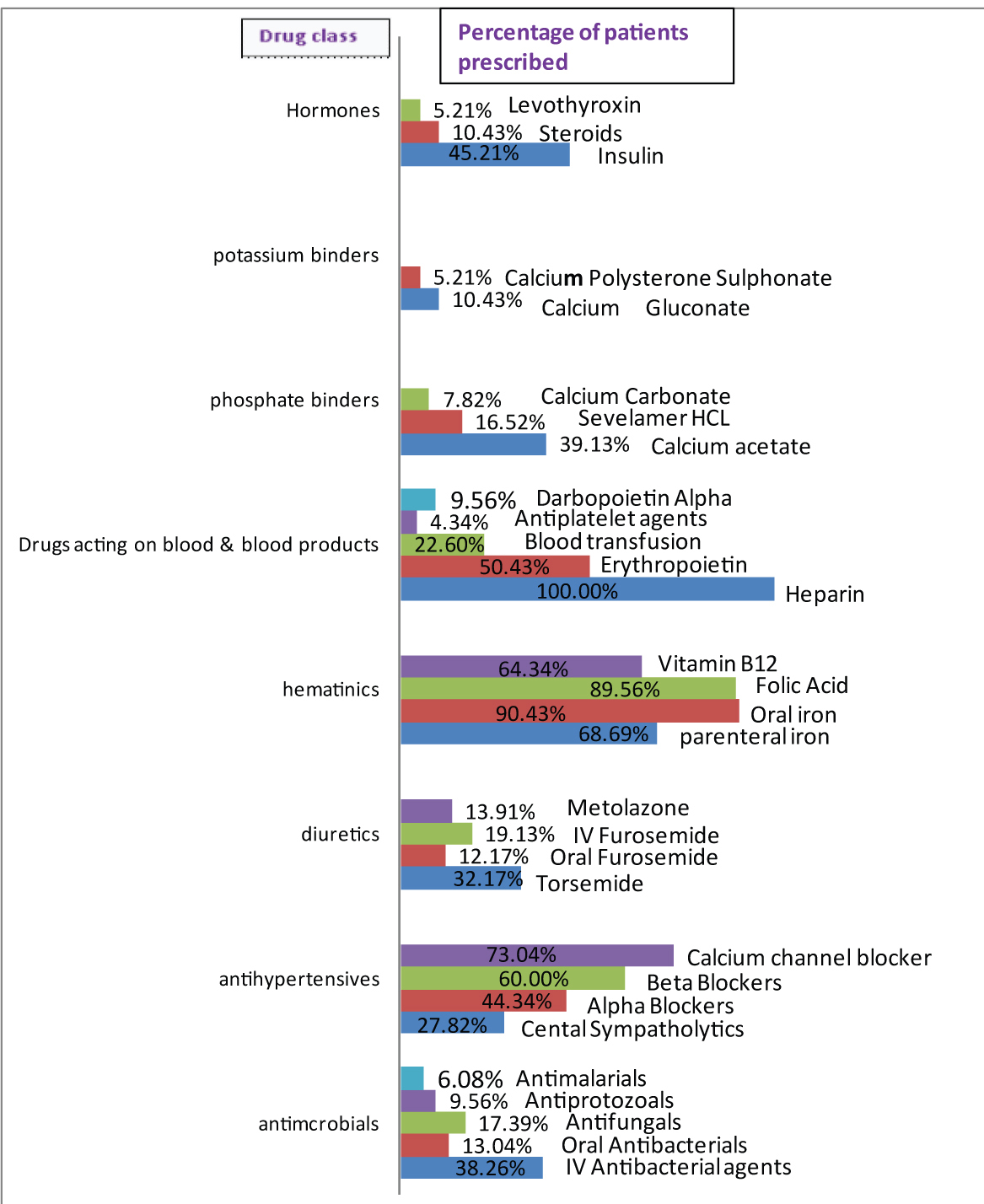
Erythropoietin stimulating agents were prescribed in 59.99% and blood transfusion was advised in 22.6% of the patients to combat anaemia. Other haematinics like oral and parenteral iron preparation, folic acid and vitamin B12 were also prescribed. Phosphate binders was prescribed in 63.47% of the patients of which calcium acetate was most frequently used followed by sevelamer hydrochloride.
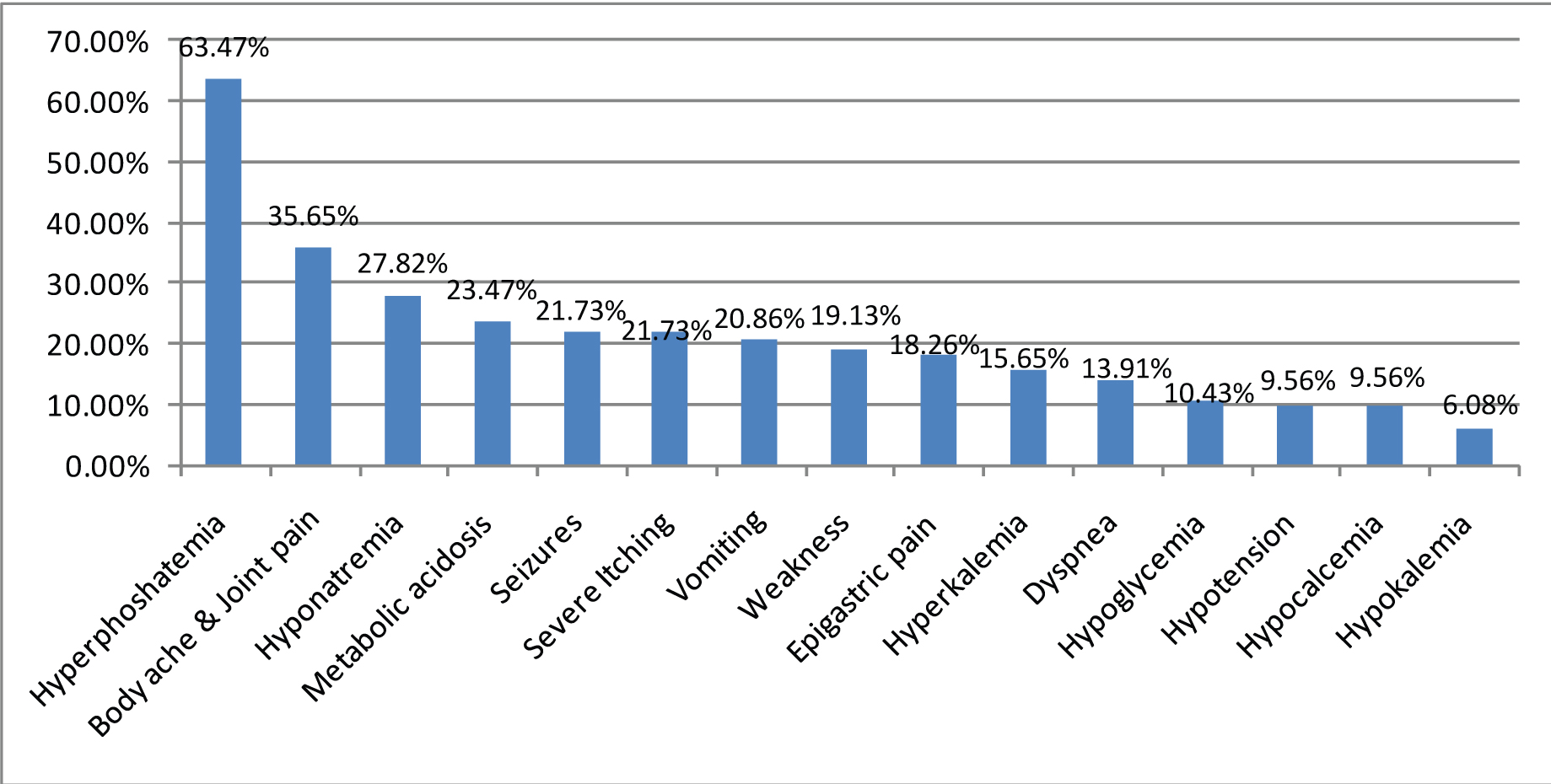
Adverse events were reported with varying severity in all the patients. Frequently observed AEs as per the laboratory investigations were hyperphosphataemia (63.47%), followed by hyponatraemia, metabolic acidosis, hyperkalemia, hypoglycaemia, hypocalcaemia and hypokalemia. In addition to these biochemical changes other AEs like epigastric pain, vomiting, bodyache with joint pain, seizure, severe itching, weakness and dyspnoea were observed. By Spearman’s correlations, AEs and age were highly correlated having correlation coefficient 0.518 with p-value<0.005. By multinomial logistic regression analysis, AEs were statistically significant with age group >45 years p=0.001 [Table/Fig-7,8].
Adverse events occurred during study.
Adverse events in relation to age and sex.
| <2 ADRs | >2ADRs | Unadjusted OR | p-value | Adjusted OR | p-value |
|---|
| <45 years | 30 | 14 | 1 | | | |
| >45 years | 12 | 59 | 10.536(4.337-25.592) | 0.001 | 0.095(.039-.231) | 0.001 |
| Male | 28 | 54 | 1 | | | |
| Female | 14 | 19 | .704(.308-1.610) | 0.405 | | |
(ADE is statistically significant with age group >45yrs p < 0.05)
Discussion
The gender distribution of the present study showed male preponderance which was similar to reported earlier studies [13,14]. The mean age of the patients was 49.26±11.46 years which was similar to a study done by Bajait CS et al., (51 years) [13]. In this study, 84.34% of the patients were in end stage renal disease in contrast to study by Bajait CS et al., and Ahlawat R et al., where only 42% were in stage V of CKD [13,14]. Studies have also included 90% of the patients in end stage renal disease [15,16]. The reason for this difference lies in the inclusion and exclusion criteria of the study.
In the present study, hypertension was found to be the most frequently associated co morbidity followed by anaemia which was similar to study by Al-Ramahi R et al., [16]. Studies by Bajait CS et al., and Ahlawat R et al., showed that hypertension was the most common co morbidity followed by type II diabetes mellitus [13,14]. The variation may be due to geographic distribution, life style and regular medical checkups. Type II diabetes mellitus associated CKD was observed in 45.21% subjects of current study in contrast to 30.63% and 40% in previous studies of Bajait CS et al., and Ahlawat R et al., respectively [13,14].
In the present study median (IQR) number of drugs prescribed per patient was 12.8 which shows the practice of polypharmacy. Similar studies by Bailie GR et al., and Manley HJ et al., in CKD patients showed similar result with average number of drugs per prescription varying from 8 to 12.3 [17,18]. Studies by Bajait CS et al., and Al-Ramahi R et al., showed average number of drugs prescribed per prescription to be 9.4 and 9.3 respectively [13,16]. Polypharmacy is defined as prescription of five or more medications to one patient at one time [19]. However, considering the requirement of polypharmacy in CKD patients, some experts advise redefining polypharmacy as nine or more medications, instead of five or more [20,21].
In our study, 40.96% medications were prescribed in generic name, in contrast to previous studies where no drug was prescribed in generic name [13-16]. Writing prescription in generic names is always recommended to promote rational use of medicines. Implementation of this practice is satisfactory in Odisha and requires more availability of the medications from Essential Drug List. Our study showed 72.62% of the prescribed drugs were from the National list of Essential Medicine which is at par with the studies of Ahlawat R et al., and Devi DP and George J where 81% and 84% of the prescribed medications were from NLEM, respectively [14,15].
Among the drugs for cardiovascular system it was observed that diuretics (6.04%) were most commonly prescribed followed by calcium channel blockers i.e., 5.70% and β blockers (4.78%) of all the drugs prescribed. Studies by Bajait CS et al., Ahlawat R et al., and Chakrabarty S et al., reported that diuretics were most commonly prescribed cardiovascular drugs (6.3%, 5.89% and 5.92% respectively of all the drugs) followed by calcium channel blockers [13,14,22]. Studies by Devi DP and George J, and Bailie GR et al., showed calcium channel blockers were most frequently prescribed cardiovascular drugs [15,23] in contrast to few other studies, ß blockers were the most frequently prescribed antihypertensives [24,25]. Bajait CS et al., Ahlawat R et al., and Chakrabarty S et al., have shown the use of angiotensin converting enzyme inhibitors or angiotensin receptor blockers in contrast to the present study [13,14,22]. In chronic renal failure or end stage renal disease, hyperkalemia is more likely to develop when angiotensin converting enzyme inhibitors or angiotensin receptor blockers are prescribed. In the present study 53.91% patients were prescribed diuretics. This finding corroborates with the study Ahlawat R et al., and Devi DP and George J, in which 54% and 50% of the patients were prescribed diuretics respectively [14,15].
Erythropoietin Stimulating Agents (ESA) like erythropoietin and darbopoiten were prescribed to a tune of 59.99% of the patients in comparison 32% in a study by Chakrabarty S et al., [22]. Underutilisation of ESA was mentioned by Bajait CS et al., due to high cost and low economic status [13]. However, in our set up none was denied of ESA, in need as most of them were under insurance scheme like Rastriya Swasthya Beema Yojna (RSBY) or Biju Krushi KalyanYojna (BKKY) or financed through Odisha State Treatment Fund (OSTF). Many drugs were also being supplied free of cost by the government of Odisha by NIRAMAYA scheme.
Among all the prescribed drugs in our study 6.04% were phosphate binders and calcium acetate was most frequently prescribed followed by sevelamer hydrochloride and calcium carbonate. Utilisation of phosphate binders was less than Bajait CS et al., and Chakraborty S et al., in which they have reported the use of phosphate binders in 11.02% and 11.20% respectively of the total drugs [13,22]. Both the studies show that calcium carbonate was the most frequently prescribed phosphate binders.
In the present study all the diabetics received insulin in contrast to the study by Chakraborty S. et al., where 65.22% patients received insulin [22]. Oral hypoglycaemic agents were not prescribed. Similar findings were obtained by Devi DP and George J, and Chakraborty S et al., [15,22]. Studies by Bajait CS et al., and Nayagam DB et al., showed that insulin was used in <50% of deteriorating renal function, as the kidney is a site of insulin degradation. Probably because of this reason glycaemic variation is high in those patients [13,26]. Since, proper monitoring was done during the hospital stay, the incidence of hypoglycaemia in our study (10.43%) was comparatively low similar to14.18% (10.72 diabetic CKD + 3.46 nondiabetic CKD) in Baltimore, US study [27].
In the present study, alimentary tract and metabolism class of drugs were prescribed less in contrast to study by Ahlawat R et al., and Chakrabarty S et al., [14,22]. Antimicrobial agents were prescribed rationally in patients with associated UTI, respiratory tract infection and cellulitis. In the present study 62% of the received antimicrobial agents in contrast to the study by Chakraborty S et al., where 82.05% of the patients did not receive any antibiotics [22].
AEs were reported with varying severity in all the patients. In the present study most frequently observed AE which was documented through laboratory investigation was hyperphosphatemia (63.47%), hyponatraemia (27.82%), metabolicacidosis (23.47%), hyperkalemia (15.65%), hypoglycaemia (10.43%), hypocalcaemia (9.56%) and hypokalaemia (6.08%). The incidence of hyperphosphataemia in CKD was due to disorder of bone turn-over and vascular calcification leading to calcium and phosphate imbalance [28]. A study by Chakrabarty S et al., reported that frequently occurring AE was hyponatraemia (32%) followed by hypoglycaemia (16%) and hypokalaemia (10%) [22]. In addition to these biochemical changes there was also other AEs like epigastic pain, vomiting, bodyache with joint pain, seizure, severe itching, weakness and dyspnoea among the study population. According to another study conducted by Nayagam DB et al., nausea was the frequent AE [26]. In accordance to few other studies,15% of the CKD patients presented with AEs like nausea, vomiting followed by 10% with headache and itching [29]. The comparison of various similar studies with the present study is shown in [Table/Fig-9].
Comparison of the present study with the previous studies.
| Core Indicator | Present Study | Chakrabarty S et al., | Nayagam BD et al., | Ahlawat R et al., | Bajait CS et al., | Al-Ramahi R et al., | Devi DP et al., |
|---|
| Study population | 115 | 100 | 83 | 408 | 111 | 600 | 102 |
| Study type | Prospective,Observational,Descriptive | Cross-sectional,Observational | Cross-sectional | Cross-sectional | Prospective,Cross-sectional, Observational | Prospective | Prospective, Cross-sectional, Observational |
| Gender Distibution (M:F) | 2.48:1 | 1.54:1 | 3.88:1 | 1.13:1 | 1.70:1 | 1.27:1 | 2:01 |
| Mean age | 49.26±11.46 | NA | 56.11±5.18 | 53.8 | 51.40±14.29 | 55.56±14.15 | 55.1±9.5 |
| Stage of Chronic Kidney Disease (%) | IV/V=15.65/84.35 | NA | NA | IV/V=21/42 | IV/V=23/46 | IV/V=7.7/88.7 | IV OR V=93% |
| Under maintainance dialysis | 100% | NA | 81.92% | NA | NA | 66% | NA |
| ASSOCIATED CO-MORBIDITY | | | | | | | |
| Hypertension | 100% | 85% | 76% | 55% | 54.95% | 80% | 100% |
| Anaemia | 90.43% | 89% | NA | 46% | 49.54% | 87.30% | NA |
| Type II Diabetes Mellitus | 45.21% | NA | 41% | 40% | 30.63% | 62.30% | 100% |
| Number of drugs/Prescription (mean) | 12.8 | 10(median) | 5.8±2.5 | 6.57% | 9.47% | 9.38±3.63 | 7.4 |
| Drugs prescribed in generic names | 40.96% | NA | NA | 0% | 0.00% | NA | 12% |
| Drugs from NLEM/ WHO MLEN(%) | 72.62%(NLEM) | NA | NA | 81%NLEM | 41.53%(W.H.O) | NA | NA |
| Cardiovascular Drugs (%) | 22.35% | 23.41% | NA | 33.90% | 22.05% | NA | 27.90% |
| Diuetics | 6.04% | 9.29% | NA | 8.20% | 9.50% | NA | NA |
| Calcium channel blockers | 5.70% | 5.92% | NA | 6.30% | 5.90% | NA | NA |
| ß Blockers | 4.68% | 0.91% | NA | 1.60% | 1.04% | NA | NA |
| Alpha blockers | 3.46% | 2.91% | NA | 1.80% | 1.54% | NA | NA |
| Centrally acting sympatholytic | 2.17% | NA | NA | NA | NA | NA | NA |
| Angiotensin converting enzyme Inhibitors | 0.00% | 0.36% | NA | 2.00% | 0.57% | NA | NA |
| Angiotensin receptor blockers | NA | 0.18% | | 2.80% | 1.23% | NA | NA |
| Patients prescribed with Diuetics | 53.91% | NA | 14.50% | 54% | NA | 49% | 28% |
| Patients prescribed with Hematopoietic agents | 60% | NA | 44% | NA | NA | NA | NA |
| Patients prescribed with phosphate binders | 63.47% | NA | 53% | NA | NA | NA | NA |
| Patients Prescribed with insulin | 45.21% | NA | 16% | NA | NA | 45.30% | 61.76 |
| Patients prescribed with drugs acting on G.I Tract | 70.43% | NA | 19% | NA | NA | 49.70% | 68.62% |
| Patients prescribed with Antimicrobial | 62.60% | NA | NA | NA | NA | 54.70% | 75.49% |
| Financed BY OSTF/Niramaya | 100% | NA | NA | NA | NA | NA | NA |
| RSBY/BKKY Insurance Scheme | 62.60% | NA | NA | NA | NA | NA | NA |
| Adverse events observed | 100% | NA | NA | NA | NA | NA | NA |
| Hyperphosphataemia | 63.47% | NA | NA | NA | NA | NA | NA |
| Hypokalaemia | 6.08% | 10% | NA | NA | NA | NA | NA |
| Hyponatraemia | 27.82% | 32% | NA | NA | NA | NA | NA |
| Hypoglycaemia | 10.43% | 16% | NA | NA | NA | NA | NA |
In case of an observational study (where we are looking for drug utilisation patterns and there is not much literature showing the prevalence of CKD patients undergoing dialysis), sample size calculation is not much of interest and it can’t proceed over inclusion/exclusion criteria and they are more important than power. Though excluded number of patients were more than 10%, it might have affected the power but criteria could not be compromised. But repeated prescription audit is required with more number of patients and longer duration of time and from multiple centers to assess changes in prescription behaviour.
Limitation
Limitation of the present study include inadequate study duration, point prevalence nature of the collected data and unicentric nature. Evaluation of drug-drug interaction and adherence to therapy in CKD patients on polypharmacy were not included in the study.
Conclusion
In spite of several limitations like inadequate sample size, study duration, point prevalence nature of the collected data and being unicentric, this study provided a profile of drug utilisation pattern in CKD patients compared by class and also individualistic comparison of drugs in the same class. Several variations in utilisation pattern were observed in CKD patients undergoing maintenance haemodialysis. This study will serve as a basis for future comparison. Certain areas like potential drug-drug interaction, AEs and adherence are needed to be explored further.
Fair portion of the drugs were prescribed from the NLEM and all the available medication in hospital were written in generic name. So, it is the need of the hour to avail all the required medication in the institution to prescribe rationally. Continuous prescription audit in both government and corporate sector will definitely improve the utilisation pattern in CKD patients undergoing maintenance haemodialysis. Insurance schemes like RSBY, BKKY and also OSTF are helping a lot to the patients below poverty line.
(ADE is statistically significant with age group >45yrs p < 0.05)