Leiomyoma of Testis –Rare Benign Mimicker of Testicular Malignancy
Asif Baliyan1, Harshi Dhingra2, Ranjeev Bhagat3
1 Ex Resident, Department of Pathology, Government Medical College, Chandigarh, India.
2 Assistant Professor, Department of Pathology, Adesh Institute of Medical Sciences and Research, Bathinda, Punjab, India.
3 Assistant Professor, Department of Pathology, Government Medical College, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Harshi Dhingra, Assistant Professor, Department of Pathology, Adesh Institute of Medical Sciences and Research, Barnala Road, Bathinda-151101, Punjab, India.
E-mail: drharshidhingra@gmail.com
Leiomyomas are benign tumours that originate from any organ containing smooth muscles. The testis is an extremely rare site. We report a case of testicular leiomyoma in a 50-year-old. Testis-associated leiomyomas are a benign and rare disease presenting as a painless, slowly-growing mass. Only histological examination with immunohistochemistry can validate the diagnosis.
Immunohistochemistry, Malignant, Orchidectomy
Case Report
A 50-year-old male presented with an asymptomatic slow growing mass in the right side of his scrotal sac since four years. This was gradually increasing in size with occasional dragging pain in right scrotum. He had no significant past history. On physical examination, his right testis was enlarged with a firm to hard, non tender swelling in the upper pole. Right epididymis and spermatic cord were unremarkable. Left testis, epididymis and spermatic cord were also unremarkable. Patient’s complete blood count and routine blood biochemistry were within normal limits. The scrotal ultrasonography showed hypoechoic lesion in right testis, with possibility of testicular malignant tumour/testicular mass. Minimal amount of fluid was noted in right tunica vaginalis. Left sided testis, epididymis and hemiscrotum were normal. Patient underwent right orchidectomy.
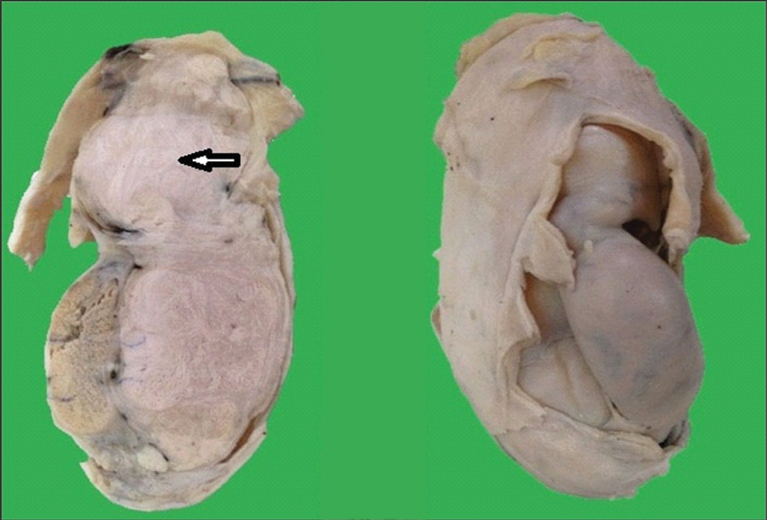
Grossly, it was a large encapsulated tumour measuring 10x6x3 cm compressing the normal testicular parenchyma on one side. Cut section of tumour was grey white, firm and showed whorling [Table/Fig-1]. The epididymis and spermatic cord were not involved.
Gross photograph showing cut surface of the well circumscribed tumour with grey white surface and areas of whorling. Normal testicular parenchyma is compressed on one side by tumour.
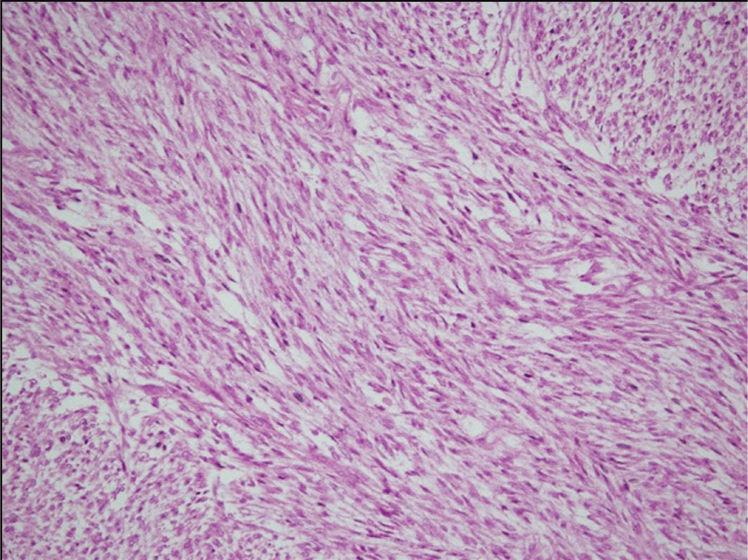
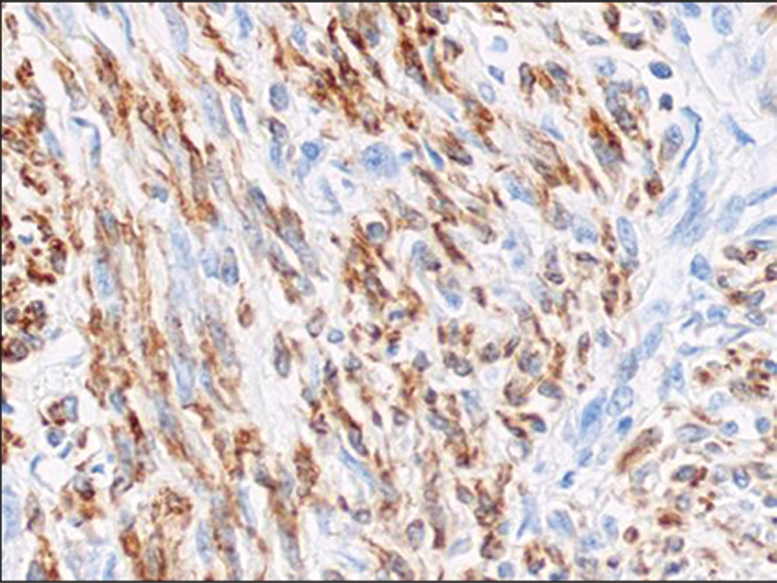
Microscopic examination revealed an encapsulated tumour composed of whorled anastomosing fasciculi and bundles of uniform spindle cells [Table/Fig-2]. The cells had indistinct cell borders and a moderate amount of eosinophilic fibrillary cytoplasm. The nuclei were elongated with blunt or tapered ends, evenly dispersed fine chromatin and small to inconspicous nucleoli. However, no atypia was noted. The mitotic activity was very low (upto 2 mitosis per 10 high power fields). Focal areas of hyalinization and haemorrhage were noted. No areas of coagulative tumour necrosis were identified. Masson trichrome stain was applied to highlight the collagen fibres and smooth muscle cells. The tumour cells were positive for smooth muscle actin and desmin [Table/Fig-3]. Thus, the final diagnosis rendered was “leiomyoma of testis”. There was no further treatment offered and clinical follow up was uneventful.
Photomicrograph shows interlacing and intersecting fascicles of uniform spindle cells having elongated nuclei with blunt ends and moderate eosinophilic cytoplasm (H&E, 10X).
Photomicrograph showing diffuse cytoplasmic staining of tumour cells with Desmin (40X).
Discussion
Leiomyomas are benign tumours that originate from any organ containing smooth muscles [1]. They constitute one of the most common tumours arising in the uterus but have also been reported in the renal pelvis, urinary bladder, spermatic cord, epididymis, prostate, scrotum and the glans penis, however, the testis is an extremely rare site. To the best of our knowledge, less than 50 cases of testicular leiomyomas have been reported in the English literature so far indicating the rarity and uniqueness of this tumour [1,2].
They are typically slow growing tumours, presenting in the fifth decade of life [1,3]. The histogenesis of leiomyoma of testis is not clear [2]. They may originate due to smooth muscle differentiation from myocytes in the wall of seminiferous tubules or from myoid cells or their progenitors present in vascular smooth muscles [4].
Albert and Mininberg testified the first case of testis associated leiomyoma in 1972 [5]. Bilateral leiomyomas have been reported, but are extremely rare. These tumours are particularly slow growing [6]. Clinically, the differential diagnosis includes malignancy, sebaceous cyst, fibroma and schwannoma. The treatment of choice is orchidectomy. The tumour is clinically asymptomatic, painless and has slow growing nature, so patients usually present late, average time being 7.6 years between the patient’s recognition of the tumour and its surgical removal [6-8].
Most of the solid intratesticular masses are malignant. Radiological identification of a testicular solid lesion must raise suspicion of malignancy, initially. However, it is important to note that besides intratesticular cysts, other benign lesions of the testis, do exist [7]. These rare benign intrascrotal tumours may lead to orchidectomies because of suspicion of testicular malignancy [2,9].
Ultrasonography is the imaging modality of choice for evaluating intrascrotal pathology. However, the radiological features of leiomyoma of the testis are undefined. The echogenicity can vary from low to high, depending on the overall sonic output during examination. Leiomyoma can be difficult to distinguish from testicular malignancy on physical examination alone or even with ultrasonography [4,9].
On ultrasonography, the tumour displays a homogenous echogenicity, the differential diagnosis of which, includes chronic hydroceles and others tumours such as adenomatoid tumours, lymphoma, germ cell tumours and fibroma [4,10].
Scrotal smooth muscle tumours arising from dartos smooth muscle can further be categorized as leiomyoma, atypical leiomyoma and leiomyosarcoma [5]. Morphological features to grade the scrotal smooth muscle tumours include: 1) size ≥five cm in greatest dimension; 2) infiltrating margin; 3) ≥five mitotic figures per 10 high-power field; and 4) moderate cytological atypia. Tumours showing only one of the features are considered benign; those showing two features are atypical leiomyomas whereas tumours showing three to four of these features are leiomyosarcomas [10].
Immunohistochemistry is required to determine the nature of spindle cells and to reach a final diagnosis. The spindled tumour cells have smooth muscle nature indicated by their cytoplasmic positivity for Smooth Muscle Actin (SMA) and are negative for S100. Other markers for smooth muscle differentiation include desmin, caldesmon, calponin and smooth muscle myosin, however, the latter two are rarely used for this purpose [1,3]. All markers show cytoplasmic staining in smooth muscle cells, however staining can be lost in poorly differentiated leiomyosarcomas [1,3,7].
The origin of the intratesticular leiomyoma is controversial. Chen YC et al., in an extensive review of literature pertaining to leiomyoma found that, broad term such as intra-testicular leiomyoma was used when testis was not involved and leiomyoma of tunica vaginalis or tunica albuginea was used when the lesions involved testis. Hence, they proposed a term “testis associated leiomyoma” even though the case was of tunica albuginea origin. They further found 41.2% of reported cases to be of tunica origin, 11.8% to be of vascular origin, 5.8% where origin was not available and 41.2% of leiomyoma with the involvement of testicular parenchyma [11].
Despite the benign nature of the lesion, treatment usually consists of radical inguinal orchidectomy with preservation of the other testis as it is difficult to differentiate this innocuous condition from other malignant entities of the testis [3].
Conclusion
Testis-associated leiomyoma is a benign and rare disease presenting as a painless, slowly-growing mass with normal alpha fetoprotein and beta-Human Chorionic Gonadotropin (β-hCG) levels. It is very challenging to make an exact preoperative diagnosis. Only histological examination with immunohistochemistry can validate the diagnosis of testicular leiomyoma.
[1]. Bremmer F, Kessel FJ, Behnes CL, Trojan L, Heinrich E, Leiomyoma of the tunica albuginea, a case report of a rare tumour of the testis and review of the literatureDiag Pathol 2012 7:140 [Google Scholar]
[2]. Kullolli VS, Kullolli S, Pawar S, Gautam D, Leiomyoma of testis –a case reportIndian J Surg 2011 73:233-35. [Google Scholar]
[3]. Chiaramonte RM, Leiomyoma of tunica albuginea of testisUrology 1988 31:344-45. [Google Scholar]
[4]. O’Brien J, Loftus B, Barrett C, Torreggiani W, Leiomyoma of the testis: a rare testicular massJ Clin Ultrasound 2008 36:240-42. [Google Scholar]
[5]. Albert PS, Mininberg DT, Leiomyoma of tunica albugineaJ Urol 1972 107:869-71. [Google Scholar]
[6]. Rakshith V, Vidyavathi K, Leiomyoma of tunica albuginea: A case report with review of literatureClin Cancer Investig J 2016 5:37-39. [Google Scholar]
[7]. Thomas J, Rifkin M, Nazeer T, Intratesticular Leiomyoma of the Body of the TestisJ Ultrasound Med 1998 17:785-87. [Google Scholar]
[8]. Cakiroglu B, Ozcan F, Ates L, Aksoy SH, Leiomyoma of the epididymis treated with partial epididymectomyUrol Ann 2014 6:356-58. [Google Scholar]
[9]. Frates MC, Benson CB, DiSalvo DN, Brown DL, Laing FC, Doubilet PM, Solid extratesticular masses evaluated with sonography: Pathologic correlationRadiology 1997 204:43-46. [Google Scholar]
[10]. Gowda KK, Rao RN, Intra-scrotal extra-testicular leiomyoma, a common mesenchymal tumour at a rare site: emphasizing the need for awareness of its occurrenceOpen Journal of Pathology 2015 5:8-11. [Google Scholar]
[11]. Chen YC, Li MH, Tsai WM, Clinical characteristics of a testis associated leiomyoma: A case report and literature reviewJTUA 2007 18:157-60. [Google Scholar]