SCHF is not only the most common fracture around paediatric elbow but also one of the most challenging to manage because of its associated complication [1-3]. These fractures account for 55% to 75% of all elbow fractures and approximately 3% of all fractures in children [4-6]. This fracture is dealt practically as an emergency with early reduction and stabilisation being the principle for better outcome. There is a spectrum of treatment modalities available for displaced SCHF in literature [7-10]. Closed reduction and percutaneous pinning has gained the universal acceptance, but consensus is yet to be arrived on the best pin configuration [11-13].
Whatever may be the modality, any delay in treatment leads to bizarre outcomes because of various associated complications. In the developing world, disorganised healthcare system, lack of transportation, psychosocial influence of Traditional Bone Setters (TBS), ignorance makes the delayed presentation inevitable. In developing countries, 10% to 20% of patients presented late for treatment [8,14]. Late presentation in SCHF is defined as approximately more than two days after trauma [7]. SCHF on delayed presentation are often difficult to treat because of massive swelling, blisters, poor soft tissue condition and may be associated with various complications, such as neurovascular injury, compartment syndrome. There is high risk of perioperative and postoperative complications such as iatrogenic nerve injury, Volkmann’s ischaemic contracture, cubitus varus deformity, elbow stiffness and myositis ossificans [3,14].
Materials and Methods
A single-centre, retrospective study was conducted between June 2011 and December 2015 in IMS and SUM hospital, SOA University, Bhubaneswar, Odisha, India, and approved by the Institutional Ethical Committee. Total 257 patients operated for SCHF fracture at our institute were reviewed retrospectively. Out of 257 (146 medial-lateral pin, 111 lateral pin) cases, those met our inclusion criteria were included in this study. Data was collected from medical records and image database. The Inclusion criteria were age between 2 to 12 years, unilateral fracture, closed Gartland type III SCHF, duration of injury beyond two days and not more than 14 days. The exclusion criteria were age less than two years or greater than 12 years, bilateral fracture, presenting less than two days after the injury, associated injury in the ipsilateral limb, previous fracture in the same limb, open fracture, unsatisfactory closed reduction requiring open reduction, associated neurovascular injury requiring surgical exploration.
Hospital databases were reviewed to determine the time since injury and arrival at hospital (emergency department or outpatient clinics), preoperative and postoperative neurovascular examination, other pertinent physical examination findings (i.e., closed injury versus open injury), reason of delay in treatment or surgery, perioperative complications or postoperative complications, hospital stay in days and resolution of any neurological or vascular compromise. Radiographic evaluation done to determine the type-III nature of the fractures, the classification of those fractures type into posterolateral and posteromedial categories. Preoperative, intraoperative and postoperative radiographs were examined to determine fracture type, accuracy of reduction.
Surgical Technique
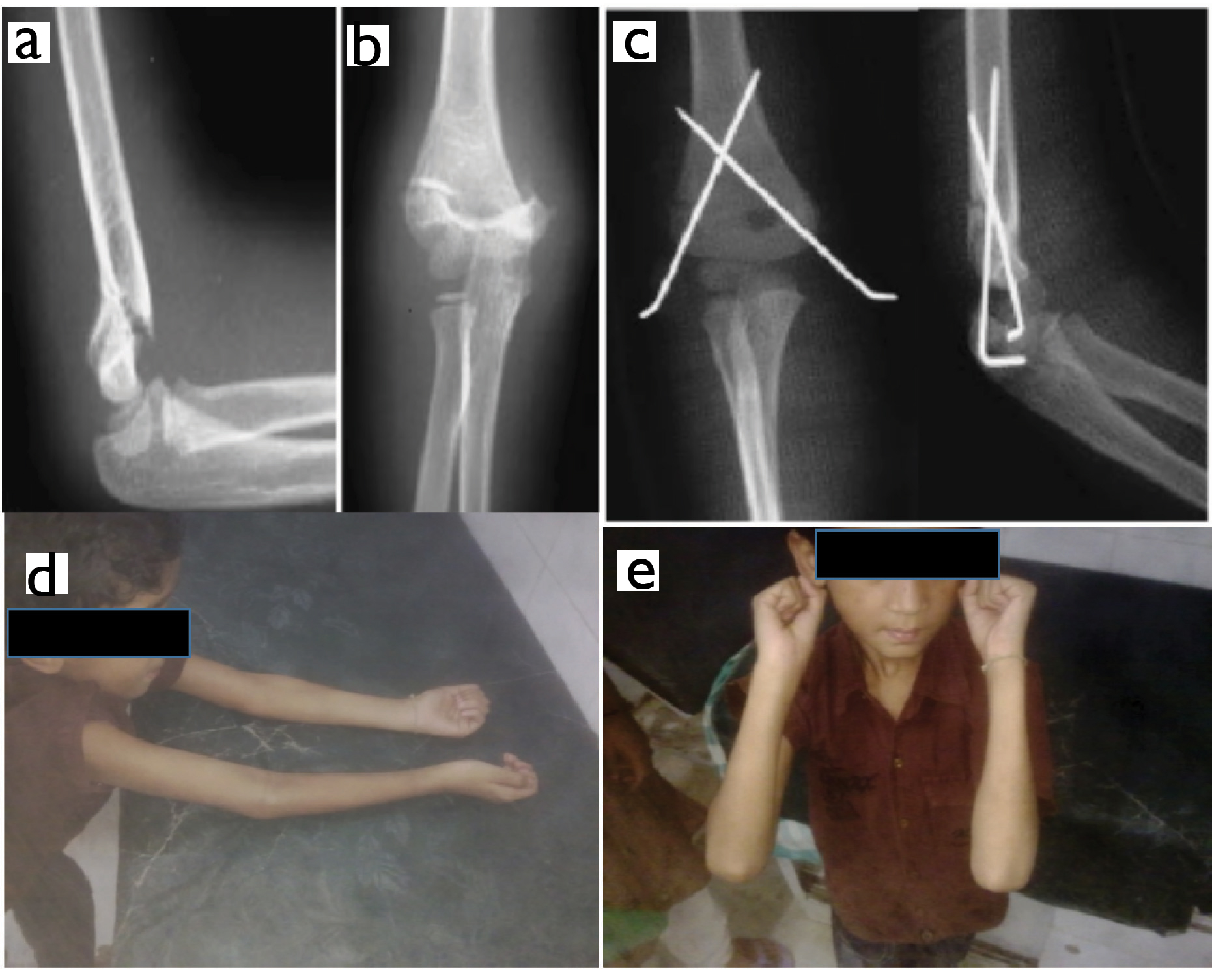
Until October 2013, medial and lateral cross K-wire fixation technique was used for SCHF (Group A). After October 2013 onward all patients were operated with lateral K-wire fixation (Group B) as per preference of surgeons. All the children underwent general anaesthesia, closed reduction and percutaneous pinning done under fluoroscopy. The surgeon selected the pin size to be used according to the age of the child and the size of the arm (usually 1.6 mm for younger (<6 year) children and 1.8 mm to 2.0 mm for older (≥ 6 year) children). In Group A [Table/Fig-1], for this medial and lateral entry technique, one pin was inserted first from the lateral aspect of the elbow across the lateral cortex to engage the medial cortex with the elbow in hyperflexion. The massive swelling in these delayed cases made palpation of medial epicondyle difficult, hence, the elbow kept in <90° to prevent anterior subluxation of ulnar nerve and the medial pin passed through a mini open (mini medial incision) technique across medial condyle to engage lateral cortex as described by Green DW et al., [18].
a,b) Anteroposterior and Lateral radiograph of elbow showing Gartland type III fracture of supracondylar humerus; c) Postoperative anteroposterior and lateral radiograph of two medial-lateral entry cross pinning showing acceptable reduction; d,e) Clinical image showing postoperative range of motion of the elbow.
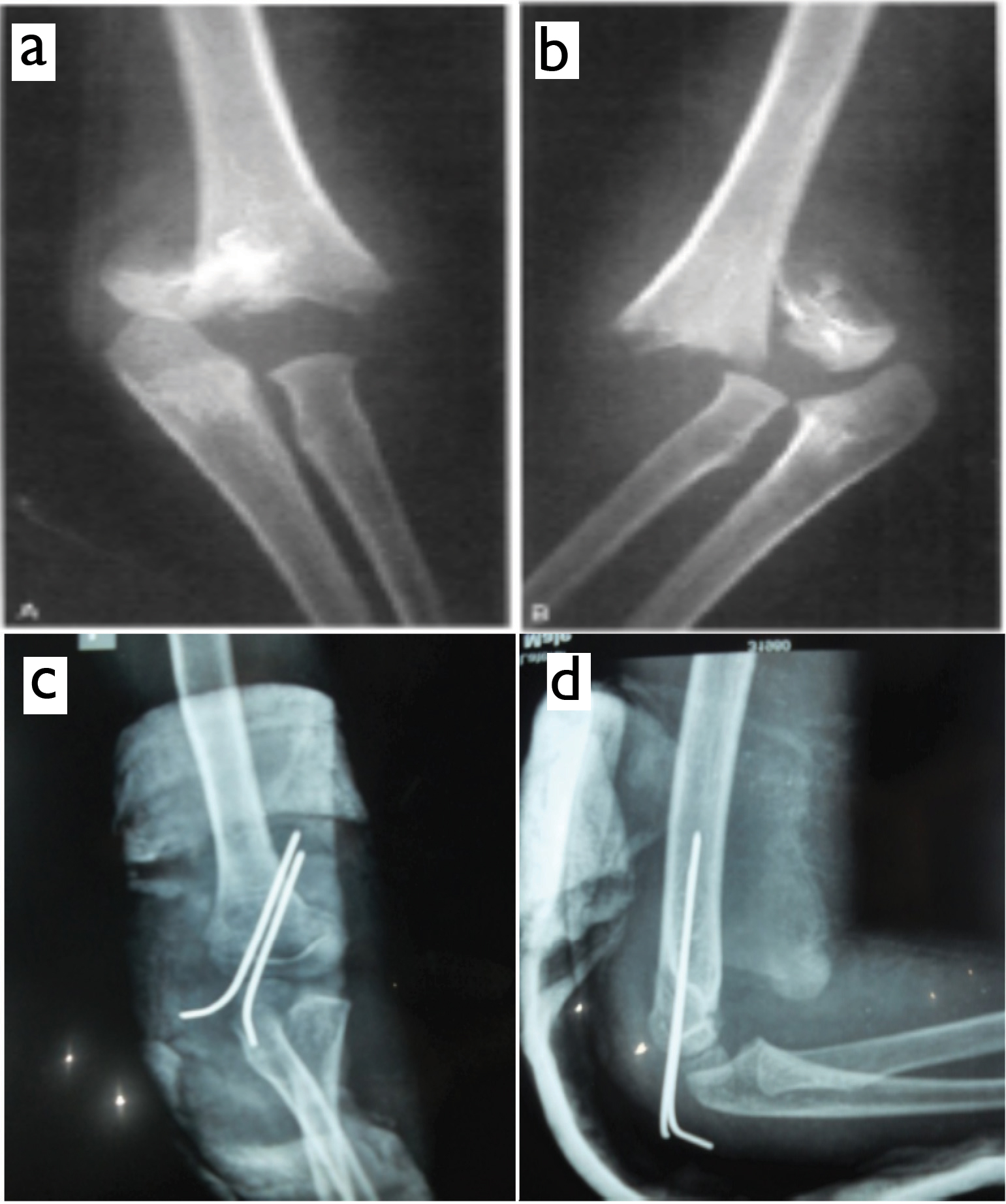
In all Group B, the lateral entry pinning was done according to the technique described by Aronson DD and Prager Bl [19]. Two pins were inserted from the lateral aspect of the elbow across lateral epicondyle to engage the medial cortex with the elbow in hyperflexion. The pins were placed in a parallel or divergent manner. Once K-wires were passed, the elbow was slightly extended, radial pulse palpated, the carrying angle and stability of reduction was confirmed [Table/Fig-2]. The K-wires were left outside the skin after being bent at right angles and immobilised with an above elbow plaster slab in 70° to 90° flexion and neutral forearm rotation. Discharge of patient done on satisfactory healing of wound. At the first follow up thorough radiological and clinical examination was done. After visible callous was evident in radiograph after three to four weeks, slab and pins removed and subsequently active Range Of Motion (ROM) of the elbow encouraged. The patients were re-evaluated as outpatients at three and six months after the surgery. Clinical evaluation included a spectrum of parameters like assessment of the carrying angle, measurement of the passive range of elbow motion, neurovascular examination of the extremity, and determination of any complications such as superficial infection, deep infection and iatrogenic nerve injury. Both anteroposterior and lateral radiograph of the elbows taken at each follow up for comparative analysis such as Baumann angle, change in Baumann angle and loss of reduction. The clinical results were graded according to the criteria of Flynn JC et al., [20], based on the loss of carrying angle and loss of flexion-extension arc of the elbow. Data retrieved whether the child has returned to full function, had minor or major limitations of function. Loss of reduction was determined on the basis of the change in the Baumann angle. No, mild, and major displacement were operationally defined according to the criteria reported by Skaggs DL et al., [17], which were based on the finding that the Baumann angle varies 6° for every 10° of humeral rotation on the anteroposterior radiograph. A change in the Baumann angle of <6° defined as no displacement, a change of 6° to 12° as mild displacement and >12° termed as major displacement [17].
a,b) Anteroposterior and Lateral radiograph of elbow showing Gartland type III fracture of supracondylar humerus; c,d) Postoperative anteroposterior and lateral radiograph of two lateral entry pinning showing acceptable reduction.
Statistical Analysis
Patients’ demographics and characteristic categorical variables were analysed. Mean±SD (minimum and maximum) for applicable variables were calculated. The Student t-test was used to compare continuous data and the Fisher exact test was used to compare categorical data between the two groups. Statistical analysis was performed with SPSS software (version 20.0; SPSS, Chicago, Illinois). A p-value of <0.05 was considered to be statistically significant.
Results
During this accrual period, 257 children were treated for a completely displaced SCHF. Of these 257 patients, 68 met the inclusion criteria with delayed presentation and 10 patients excluded as they underwent open reduction. Hence, total 58 patients included for this study.
The Group A comprised 31 children and 24 (77.4%) patients were male while 7 (22.6%) patients were female. The mean age of 8.55±2.40 (3-12) years. The involvement of left side was 12 (38.7%) and right was 19 (61.3%). The displacement was posterolateral in 7 (22.6%) and posteromedial in 24 (77.4%) patients. The average delay between the day of injury and day of operation was 4.07±1.14 (3-7) days. The cases delayed due to patronage by TBS were 19 (61.2) %. The mean hospital stay was 3.07±0.78 (2-6) days. Mean duration of follow up was 37.59±9.06 (30-61) weeks.
The Group B comprised 27 patients and 8 (29.6%) patients were female while 19 (70.4%) patients were male. The mean age was 8.19±2.21 (4-12) years. The involvement of left side was 6 (22.2%), while right was 21 (77.8%). The displacement was posterolateral in 4 (14.8%) and posteromedial in 23 (85.2%) children. The mean delay between the day of injury and day of operation was 4.87±1.11 (3-7) days. The cases delayed due to patronage by TBS were 18 (66.7%). The mean hospital stay was 3.32±0.79 (2-5) days. Mean duration of follow up was 38.93±8.77 (31-64) weeks. There were no significant differences (p>0.05) between groups with regard to any of these variables. No patient in either group had a major loss of reduction; (n=1) in Group A and (n=4) patients treated in Group B had a mild loss of reduction; this was not a significant difference (p=0.107). There were no significant differences (p>0.05) between the Groups regarding the Baumann angle, change in the Baumann angle, carrying angle, elbow extension, elbow flexion, total elbow Range of motion, Flynn grade, functional return [Table/Fig-3].
Data Analysis of patients with comparison of variables between groups.
| Variables | Medial-lateral groupGroup A | Lateral groupGroup B | p-value |
|---|
| No. of patient | 31 | 27 | - |
| Age (years) | 8.55±2.40 | 8.19±2.21 | 0.623 |
| Sex |
| Male | 24 | 19 | - |
| Female | 7 | 8 | - |
| Delay in presentation (days) | 4.07±1.14 | 4.87±1.11 | 0.632 |
| Loss of reduction | |
| None | 30 | 23 | 0.107 |
| Mild | 1 | 4 |
| Major | - | - |
| Loss of Range of motion (ROM) degree | 7.77 ±2.02 | 7.87± 3.63 | 0.568 |
| Flexion | -2 | -1.2 |
| Extension | 133.5 | 133.5 |
| Total ROM | 134.5 | 133.9 |
| Baumann angle (degree) | 75.5±1.61 | 76.3±2.44 | 0.271 |
| Change in Baumann angle | 4.77±0.97 | 4.98±1.18 | 0.334 |
| Carrying angle loss (degree) | 3.70±1.46 | 3.85±1.80 | 0.825 |
| Flynn grade |
| Excellent | 28 (90.3%) | 24 (88.9%) | 0.888 |
| Good | 3 (9.7%) | 2 (7.4%) |
| Fair | - | 1 (3.7%) |
| Poor | - | - |
| Return to function |
| Full | 29 (93.5%) | 24 (88.9%) | 0.849 |
| Minor limitation | 2 (6.4%) | 3 (11.1%) |
| Major limitation | - | - |
Average loss of range of motion was 7.77±2.02 (3-12)° in Group A and 7.87±3.63 (4-12)° in Group B. This was not a significant difference (p = 0.568). Average loss of carrying angle in Group A was 3.70±1.46 (2-7)° while in Group B was 3.85±1.80 (2-7.5)°. This was not a significant difference (p=0.825). Baumann angle in Group A was 75.56±1.61 (70.5-80)° and in Group B it was 76.30±2.44 (69.2-81.5)°. This was not a significant difference (p=0.271). Average change in Baumann angle in Group A was 4.77±0.97 (3.1-6.8)° and in Group B was 4.98±1.18 (2.3-7.5)°. This was not a significant difference (p=0.334). According to Flynn criteria final result in Group A, excellent was in 28 (90.3%), good was in 3 (9.7%) and in Group B excellent was in 24 (88.9%), good in 2 (7.4%) and fair in 1 (3.7%) cases. This was not a significant difference (p=0.888). Return to full function in Group A was 29 (93.5%) patient got full functional recover with minor limitation in 2 (6.4%) while in Group B full functional was in 24 (88.9%), with minor limitation in 3 (11.1%). This was not a significant difference (p=0.849) [Table/Fig-3].
Postoperative complications like pin tract infection was found in five cases (n=2 in Group A and n=3 in Group B). Pin tract infection completely healed by short course of antibiotics after removal of pins. Iatrogenic transient ulnar nerve injury was found in three cases in Group A and all fully recovered after three month follow up.
Discussion
In the developing world, proportion of delayed presentation SCHF is much higher because of disorganised healthcare delivery systems, patients reaching the tertiary care centre late because of poor transportation, some traditional incorrect intervention by non-medical personnel or TBS, ignorance of parents and various socioeconomic factors [21]. Majority of this study patients had received some kind of patronage by TBS resulted various complications such as blister, severe swelling, and compartment syndrome, that further complicated or delayed surgical intervention following SCHF in children.
Closed reduction with percutaneous crossed K-wires is the preferred method of treatment for SCHF in children [8,11,17]. But, a major concern with delayed treatment is the inability to achieve satisfactory closed reduction. Because of the severe swelling and the rapid healing of metaphysis in children and presence of soft tissue callus by the end of the first week, renders the fracture irreducible [20]. Thus, these factors produce higher chance of conversion to open reduction. Though, the rate of conversion to open reduction has been reported in literature as ranging from less than 3% to up to 46% [22-24]. In this study, 10 (14%) required open reduction with mean delay in presentation of 8.6 days. Severe tissue oedema and poor skin condition such as blister may cause difficulty in wound closure and healing following open reduction. Though, few study demonstrated open reduction and internal fixation has earned a poor reputation because of elbow stiffness and myositis ossificans which may present as a late complication [25].
Closed reduction with percutaneous crossed K-wires has gained popularity as the preferred method of treatment for SCHF in children [6,9,11,26].
Though various studies compared cross versus lateral pin in fresh cases of SCHF but lacking in delayed cases. However, controversy persists regarding whether two lateral pin or medial and lateral cross pin fixation is the optimal technique in delayed type SCHF. Previous studies have demonstrated that increased biomechanical stability is the advantage of medial and lateral cross pin fixation, although the chance of iatrogenic ulnar nerve injury may result from placement of the medial pin [16,26]. Recent studies demonstrated that two properly placed lateral pins either parallel or divergent pins engaging medial cortex provide sufficient fixation strength with lower the risk of iatrogenic ulnar nerve injury [12,17] [Table/Fig-4]. Summarises the results and conclusions of some similar studies [6,9,27].
Various similar studies for comparison.
| Study | Year | No of case | Mean delay surgery | Operative methods | Result (Flynn’s criteria) | Complication |
|---|
| Dua A et al., [6] | 2011 | 40 | 17.55 hours | CRPPMedial lateral pin | 95% excellent | PI-3 casesMO-2 cases |
| Tiwari A et al., [9] | 2007 | 40 | 4.5 days | Cross k wire | 88 %Satisfactory | MO-5%PI- 6.5% |
| Foead A et al., [27] | 2004 | 55(28-cross pin, 27-lateral pin) | 7-73 hours | CRPP cross versus lateral pin | 21 cases cross, 22 lateral pin) excellent | IN-5 Cross pin2-lateral pinPI-3(2-Cross, 1-lateral pin) |
| Present study | 2017 | 58(31-cross pin, 27-lateral pin) | 4 days cross, 4.8 days lateral pin | CRPP cross versus lateral pin | (90.3% cross,88.9% lateral pin)excellent | IN-3 cross pinPI-(2 cross3-lateral pin) |
CRPP- Closed reduction and percutaneous pinning; ORIF- Open reduction and internal fixation; MO- Myositis ossificans; IN- Iatrogenic nerve injury, PI- Pin tract infection).
Though few studies [11,15-17,27,28] have been compared the efficacy of medial and lateral cross pinning with lateral pinning for percutaneous fixation of displaced supracondylar fractures of the humerus in children. All of these studies found no significant difference between the two methods in terms of loss of reduction. Only few shows significant difference in favour of lateral entry pinning method in terms of iatrogenic nerve injury [16,17].
A study by Wang X et al., demonstrated that crossed pinning is biomechanically more stable than lateral pinning in rotational testing as well as varus and valgus forces [26]. The reported risk of loss of reduction following lateral pin fixation has also varied widely.
Skaggs DL et al., reported no loss of reduction in lateral pin fixation group and found no difference in term of stability between crossed and lateral pins [17]. The rate of displacement following lateral entry pin fixation was 2.1% as reported by Kocher MS et al., [11]. In this study, none of our patients had a major loss of reduction during follow up. Therefore, we found no difference in the stability of fixation either the medial-lateral cross pin fixation or two lateral pin fixation especially in the delayed conditions. The primary concern with medial lateral cross pinning is the risk of injury to ulnar nerve by the medial pin. Injury to the ulnar nerve could be due to local irritation or pressure from the medial pin especially during insertion. The bony landmarks are obscured due to massive swelling and the risk of injury to the ulnar nerve becomes higher in delayed presentation [6,21]. The necessity to hyperflex the elbow during the reduction, tendency of the hypermobile ulnar nerve to subluxation anteriorly and blind passage of the medial pin all contribute to ulnar nerve injury. In a systematic review, Brauer CA et al., reported the risk of iatrogenic ulnar nerve injury was 1.84 times higher with medial and lateral cross pins than with lateral entry pin alone [29]. Tiwari A et al. demonstrated nil cases of iatrogenic ulnar nerve injury among patients treated even with a mean delay of 4 days [9]. Skaggs DL et al., reported iatrogenic ulnar nerve injury was seen in 10.6% (17 cases) of total 160 cases treated with a medial pin placement [28]. In a recent study by Lee KM et al., the risk of iatrogenic ulnar nerve injury was 0–6.8 % [16]. However, Green DW et al., minimized the iatrogenic ulnar nerve injury by adapting miniopen technique [18]. In this study, and due to fact that the fixation was done after miniopen technique, still three patients had transient ulnar nerve involvement postoperatively though resolved spontaneously. We assume that the transient ulnar nerve palsy in three cases may be due to local irritation or pressure of medial pin. Although medial-lateral cross pin fixation produced more incidence of iatrogenic ulnar nerve injury as compared to lateral pin fixation, this observation could show a trend but that could only be verified with a larger sample size. This value is too small to be analysed and to reach to any conclusion.
Unlike other studies, deep infections, compartment syndrome and osteomyelitis following fixation of supracondylar fracture are rare [6,9,11,28]. While pin tract infections and superficial skin infections are common, which usually heal well with short course oral antibiotics and after K-wire removal. In this study, 5 (8.6%) out of 58 patients developed pin tract infection at K-wires insertion site but healed with short course of oral antibiotics after K-wire removal. Although, pinning techniques have reduced the incidence of cubitus varus deformity, still it is the most common complication accounting 10%-30% of cases regardless of the method of treatment and does not improve with remodelling [14].
Limitation
The limitations of our study were related to the retrospective design. As with other studies that occur at a single institute and retrospective in nature, a number of elements may have biased result. However, a prospective randomised study required to substantiate the claim.
Conclusion
Delayed presentation with its associated complications no more a deterrent to early surgical management of displaced supracondylar fractures. The results of the present study endorse the fact that with slight modifications in skill, both cross pinning or lateral pinning produce promising outcomes in terms of good reduction, improvement of function. We recommend closed reduction and percutaneous skeletal stabilisation for displaced SCHF in children presenting even upto seven days after injury. Although both the techniques appear to be equally effective, in term of stability and outcomes but lateral pinning has a definite edge over cross pinning in respect to reduced incidence of iatrogenic ulnar nerve injury, especially in late presenters with poor soft tissue conditions and massive swelling.
CRPP- Closed reduction and percutaneous pinning; ORIF- Open reduction and internal fixation; MO- Myositis ossificans; IN- Iatrogenic nerve injury, PI- Pin tract infection).