Extra-Nasopharyngeal Angiofibroma in a Pre-Pubertal Child
Subhro Ganguly1, Surendra H Gawarle2, Prashant N Keche3
1 Senior Resident, Department of Oto-Rhino-Laryngology, Topiwala National Medical College, Mumbai, Maharashtra, India.
2 Professor, Department of Oto-Rhino-Laryngology, Shri Vasantrao Naik Government Medical CollegeYavatmal, Maharashtra, India.
3 Associate Professor, Department of Oto-Rhino-Laryngology, Government Medical College, Aurangabad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Subhro Ganguly, Senior Resident, Department of Oto-Rhino-Laryngology, Topiwala National Medical College and BYL Nair Hospital, Mumbai, Maharashtra, India.
E-mail: subhro.mck@gmail.com
Nasopharyngeal Angiofibromas (NA) are benign fibro-vascular tumours, predominantly occurring in the region around sphenopalatine foramen of adolescent males. Angiofibromas arising outside nasopharynx are termed as Extra-Nasopharyngeal Angiofibromas (ENA) which often gets misdiagnosed because of its rarity and atypical clinical and biological behaviour.
We present a case of angiofibroma of nasal septum in a seven-year-old boy presenting with two months history of left nasal obstruction and occasional nasal bleeding. CECT revealed a contrast enhanced soft tissue mass in left nasal cavity with no extension into the sinuses and nasopharynx. The mass was completely removed by lateral rhinotomy approach and a follow up of ten months showed no recurrence. Histopathology and immunohistochemistry confirmed the diagnosis of angiofibroma. The age of the patient and the location of the tumour make the case exceptionally rare. We conclude that ENA must be taken into consideration in differential diagnosis of unilateral vascular nasal mass, and nasal septum should be taken into account as a potential, yet exceptional site for the tumour. Furthermore the age and gender of the patient should not be given utmost importance for diagnosis of angiofibromas.
Pre-pubertal child, Nasal septum, Unilateral vascular nasal mass
Case Report
A seven-year-old boy visited the ENT Department of our centre with a three month history of left sided nasal obstruction and recurrent spontaneous, painless epistaxis. Rigid nasal endoscopy was performed and a fleshy mass was seen arising from the antero-inferior part of the left side of the nasal septum and filling the left nasal cavity.
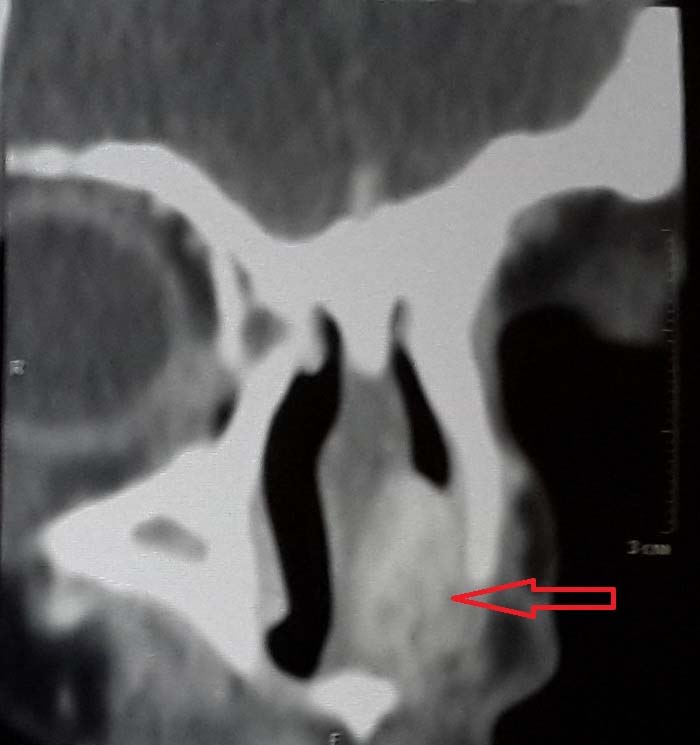
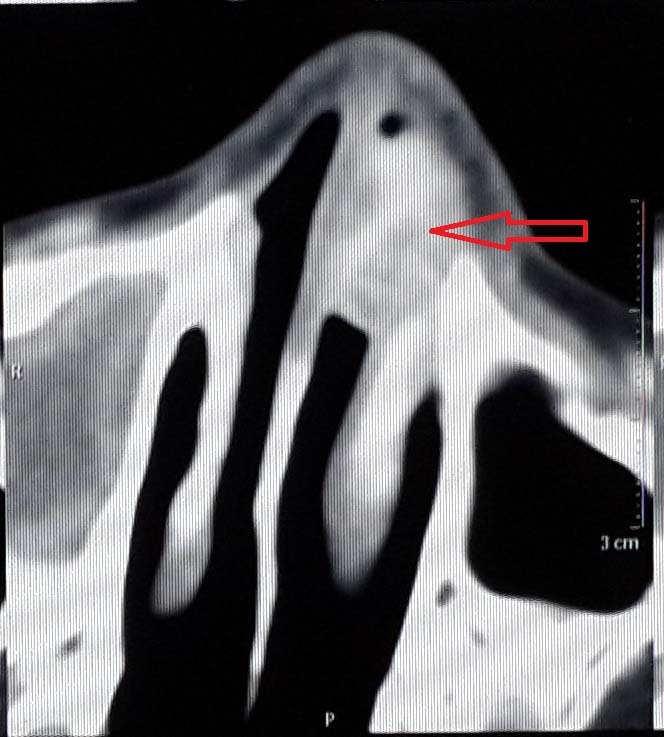
Computerised Tomography (CT) scan of paranasal sinuses showed a homogenous soft tissue lesion measuring 26 x 18 x 14 mm in left nasal cavity. All the paranasal sinuses were clear. No bony erosion was seen on CT scan. On contrast study, there was homogeneous enhancement indicating a vascular tumour [Table/Fig-1,2].
Preoperative CT scan coronal view showing a soft tissue density lesion in left nasal cavity with homogenous contrast enhancement (arrow).
Given the vascularity of the tumour on CT scan, biopsy was not taken and the patient was sent for excision of the nasal mass under General Anaesthesia (GA) after taking informed consent. The mass was removed completely by a standard endoscopic approach with removal of a cuff of septal perichondrium. The intra-operative blood loss was approx. 50 ml. Anterior nasal packing was done and the pack was removed after 48 hours with no episodes of further bleeding. The operative procedure and the postoperative recovery periods were uneventful.
Preoperative CT scan axial view showing a soft tissue density lesion in left nasal cavity with homogenous contrast enhancement (arrow).
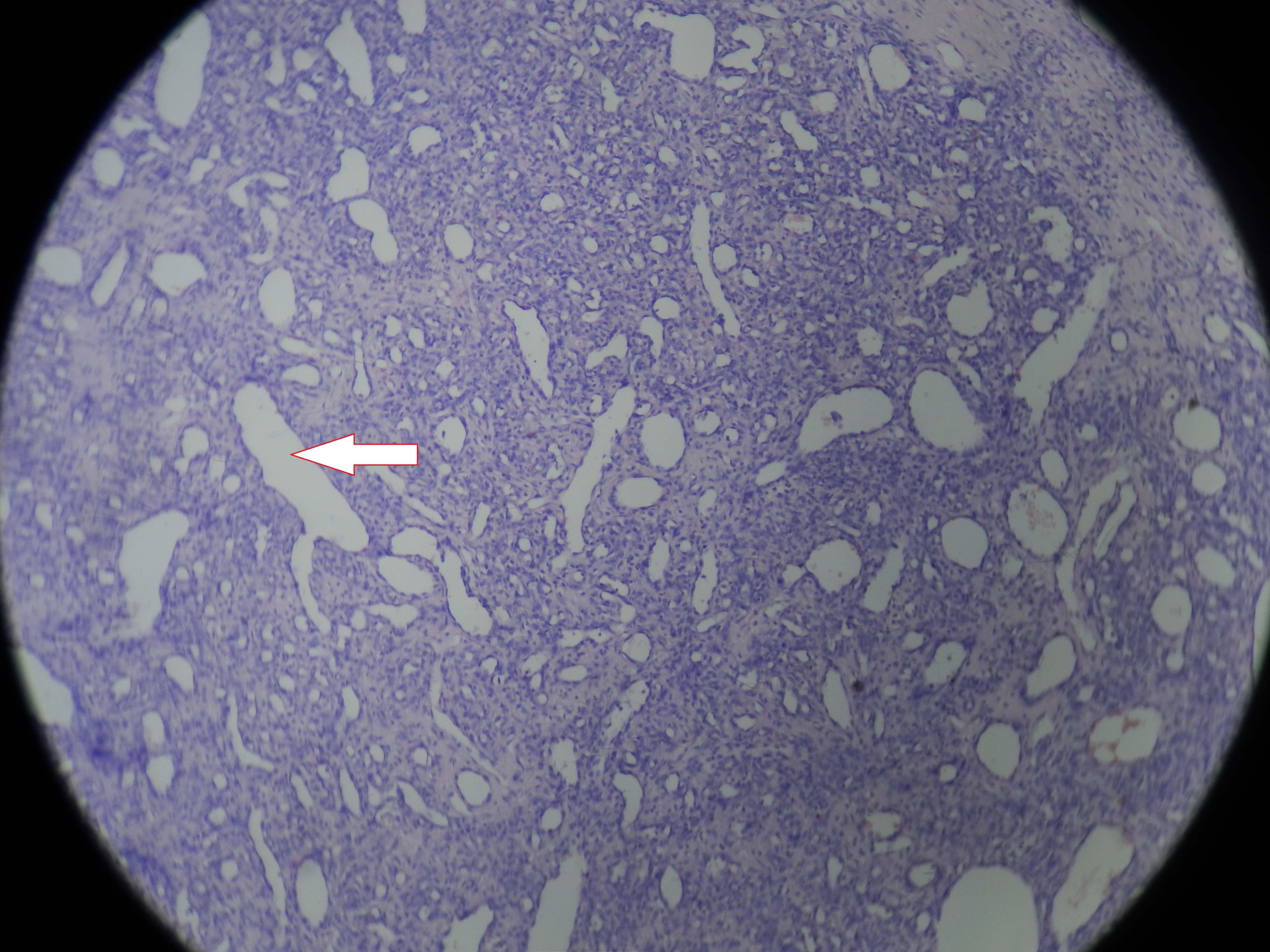
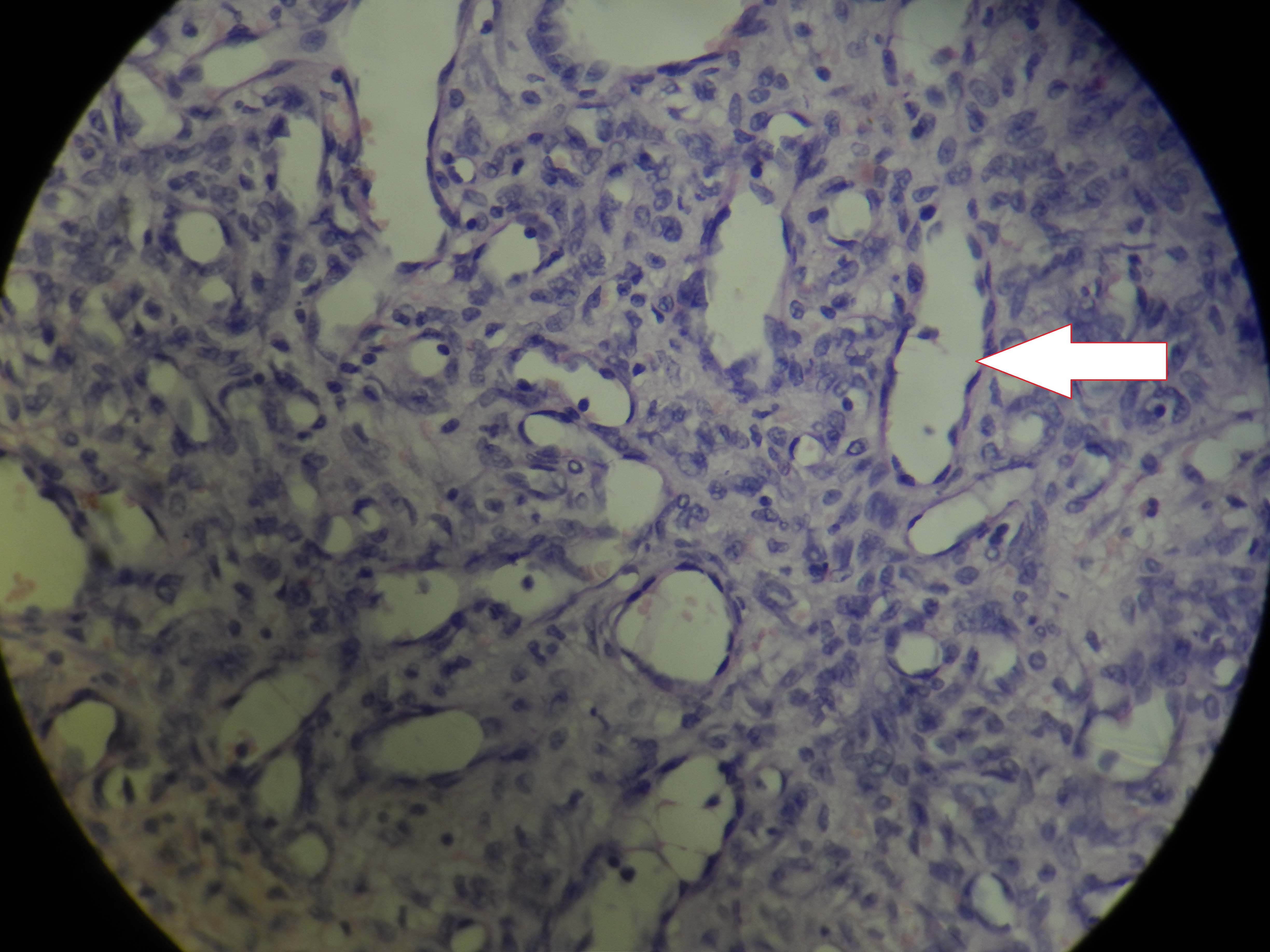
Histopathology of the excised specimen showed endothelial cells without muscular layer with fibrous stroma [Table/Fig-3,4]. The findings were consistent with the diagnosis of angiofibroma. A regular follow-up for a period of one year showed no signs of recurrence.
Histopathology pictures showing dense fibrous stroma with immature blood vessels (arrow) suggestive of angiofibroma (H and E 4X).
Histopathology pictures showing dense fibrous stroma with immature blood vessels (arrow) suggestive of angiofibroma (H and E 40X).
Discussion
NA are benign but locally aggressive non-encapsulated fibro-vascular tumours accounting for only 0.05-0.5% of all head and neck tumours [1]. Angiofibromas that do not originate in the vicinity of sphenopalatine foramen or pterygoid plates are termed as ENA [2].
The term “juvenile NA” was first coined by Chauveau in 1906 [3]. Tumours sharing similar histopathological features with angiofibromas but not originating in the nasopharynx are termed as ENA. De Vincentiis G and Pinelli V reviewed a total of 704 cases of angiofibroma in 1980 and only 13 out of them originated outside nasopharynx thus confirming that ENA is a distinct yet rare entity [4]. Windfuhr JP and Remmert S in 2004 reported 65 cases of ENA [1]. According to Celik B et al., the term ‘Atypical Angiofibroma’ should be reserved for these tumours [5].
Maxillary sinus is the most common site for ENA followed by ethmoid and sphenoid sinus [2,4]. Angiofibromas of the nasal cavity are extremely rare and have been reported to occur in the septum, inferior and middle turbinates, and nasal vestibule. The nasal septum is an extremely rare site with only handful of cases being reported in the literature [4]. Nasal septal Angiofibromas may occur at the anterior one third of the nasal septum, the bony cartilaginous junction, or the etmoidal perpendicular plate.
There are various theories explaining the site of origin of NA. Brunner described fascia basalis as the tissue of origin, which extends over the roof of the nasopharynx to vomer, the palatine bone, the posterior ethmoid, and the medial pterygoid process [6]. Since the site of origin in our case was the antero-inferior septum where there is no fascia basalis, it could have arisen from the ectopic tissue trapped during the growth of nasal septum.
Most literature indicates that the NA originates at the sphenopalatine foramen with recent study identifying pterygoid canal as the site of origin [7].
The exact nature and histogenesis of NA is still unclear. Some data support the vascular malformation hypothesis of NA arising from discontinuous vascular basal laminae, focal lack of pericytes, and pronounced irregularity of the smooth muscle layers [9]. Other data support the angiogenic histogenetic hypothesis of NA [10].
Apart from the difference in location the clinical features of ENA along with the age and gender of the patients are in stark contrast with NA. Mean age of presentation of ENA was 22 years as documented by Huang RY et al., and male to female ratio was 3:1 as compared to classical NA which occur typically in adolescent males [11]. The age of our patient fits in the neither group which makes it unique.
Frequent symptoms are unilateral nasal obstruction, recurrent epistaxis, facial deformities and pain. Unlike NA, the symptoms of ENA are much more variable, appear much early and the bleeding episodes are less severe [2,4].
NA has a homogenous contrast enhancing appearance on CT and MRI whereas ENA has heterogeneous appearance and may not show much contrast uptake because of its poor vascular supply [2,4]. Absence of hypervascularity on arteriography does not rule out ENA.
Angiofibromas are histologically composed of a dense fibrous stroma and a proliferating vascular component. The vascular element is characterized by blood vessels of different size ranging from capillaries to venules lined only by single layer of endothelium. A dense acellular stroma and excessive collagen tissue is pathognomic for ENA which also shows less number of vascular elements compared to NA [2,4].
Surgical removal via wide local excision is the treatment of choice and the approach varies with the location of the tumour. Endoscopic approach has several advantages over classical open approaches like reduced morbidity, less operative time, less scar, better exposure and magnified view. Pre-op embolization is beneficial for bulky tumours and unlike NA, radiotherapy has no significant role for the management of ENA [2].
Compared to NA where recurrence is common (50-61%), it is not yet reported in case of ENA [2].
Conclusion
We conclude that ENA should be considered as a separate entity and should be kept in the differential diagnosis of unilateral vascular nasal mass irrespective of the age, gender, site of origin and extent of the tumour. As there are very few case reports available in the literature we need more experience with this rare tumour to make a comprehensive profile and a standard protocol for its management.
[1]. Windfuhr JP, Remmert S, Extranasopharyngeal angiofibroma: etiology, incidence and managementActa Otolaryngol 2004 124:880-89. [Google Scholar]
[2]. Szymanska A, Szymanski M, Morshed K, Czekajska-Chehab E, Szczerbo-Trojanowska M, Extranasopharyngeal angiofibroma: clinical and radiological presentationEur Arch Otorhinolaryngol 2013 270(2):655-60. [Google Scholar]
[3]. Chauveau C, Histoire des Maladies du Pharynx 1906 Paris, FranceJ.B. BalliereetFils [Google Scholar]
[4]. De Vincentiis G, Pinelli V, Rhinopharyngealangiofibroma in the pediatric age group. Clinical-statistical contributionInt J PediatrOtorhinolaryngol 1980 2:99-122. [Google Scholar]
[5]. Celik B, Erisen L, Saraydaroglu O, Coskun H, Atypical angiofibromas: a report of four casesInt J Pediatr Otorhinolaryngol 2005 69:415-21. [Google Scholar]
[6]. Brunner H, Nasopharyngeal fibromaAnn OtolRhinolLaryngol 1942 51:30-65. [Google Scholar]
[7]. Doğan S, Yazici H, Baygit Y, Metin M, Soy FK, Extranasopharyngeal angiofibroma of the nasal septum: a rare clinical entityJ Craniofac Surg 2013 24:390-93. [Google Scholar]
[8]. Liu ZF, Wang DH, Sun XC, Wang JJ, Hu L, Li H, The site of origin and expansive routes of juvenile nasopharyngeal angiofibroma (JNA)Int J Pediatr Otorhinolaryngol 2011 75:1088-92. [Google Scholar]
[9]. Starlinger V, Wendler O, Gramann M, Schick B, Laminin expression in juvenile angiofibroma indicates vessel’s early developmental stageActa Otolaryngol 2007 127:1310-15. [Google Scholar]
[10]. Zhang M, Sun X, Yu H, Hu L, Wang D, Biological distinctions between juvenile nasopharyngeal angiofibroma and vascular malformation: An immunohistochemical studyActa Histochem 2011 113:626-30. [Google Scholar]
[11]. Huang RY, Damrose EJ, Blackwell KE, Cohen AN, Calcaterra TC, ExtranasopharyngealangiofibromaInt J PediatOtorhinolaryngol 2000 56:59-64. [Google Scholar]