In the era of modern day of civilization and economic globalization, lot of changes are taking place with disease distribution, family patterns and social support not only in India but also throughout the whole world. Inappropriate posture at work and improper lifestyle leads to varied musculoskeletal problem.
Chronic LBP is one such prevalent musculoskeletal disorder. LBP refers to pain or stiffness in muscle localised below the costal margin and above the inferior gluteal folds, with or without leg pain [1]. It affects 80 percent of the global population [2] with men developing symptoms much earlier than women [3]. LBP is termed as chronic when it persists beyond 3 months [4]. Disability related to chronic LBP is associated with high social and health costs [5]. The problem of chronic LBP among industrial workers engaged in heavy manual work has been investigated in the Indian context. Approximately 55% jute workers are having chronic LBP [6].
Significant and long lasting pain relief can be achieved with transforaminal epidural steroid injection [7]. Surgery is indicated for those patients with progressive neurological deficits or severe LBP refractory to conservative measures [7]. Objective improvement of treatment and efficacy of transforaminal epidural steroid injection can be adequately estimated by analysing walking pattern of patients with measurement of pelvic angle. In the specialty of pain medicine, literatures on gait analysis are very few. For assessment of back pain, proper gait analysis of the hips as well as the spine [8] is required.
The aim of the study is to evaluate the efficacy of transforaminal epidural steroid injection through pelvic angle measurements, pain and disability measurements. This trial also tried to integrate kinematic study as an objective measurement after transforaminal epidural injection for the patients suffering from low back pain with unilateral radiculopathy.
Materials and Methods
Study Design
This was a prospective, single centre, randomized, controlled clinical trial. The study was reviewed and approved by Research Evaluation committee and the Institutional Ethical Committee. Information about the trial was given comprehensively, both orally and in written form, to the patients. Accordingly all patients gave their written informed consent prior to their inclusion into the study.
Patient Selection
The study was designed as prospective non blinded randomized controlled trial in which treatment efficacy of transforaminal epidural steroid injection was assessed by gait analysis using pelvic angle measurements, pain and disability scores. The study was conducted in the Department of Pain in a city based hospital for the industrial workers at Kolkata, India. Duration of this study was 1 year; from October 2015 to September 2016.
Total 60 patients were recruited in this study. Among them 30 patients were selected as case after disease confirmation and another 30 patients were selected as control. Sample size was determined after reviewing various published journals [9].
Subjects who fulfilled the following criteria were included in this study. They were subjects with age between 18 and 60 years. Patents were having Lumbar disc herniation and unilateral radiculopathy with chronic LBP of more than 3 months with pain intensity limiting function and NRS score above 5. All patients must have been capable of understanding the trial protocol. Only subjects with clinically, radiologically and neuro-physiologically diagnosed disc herniation at L3-4, L4-5 and L5-S1 were included.
Subjects were excluded if they had a history of previous lumbar surgery, Radiculopathy secondary to spinal canal stenosis, amenable for neurosurgery or having red flag signs, Radiculopathy without disc herniation, bilateral radiculitis, uncontrolled medical illnesses and unstable psychiatric disorders. Pregnant and lactating women were also not included. Extremely high dose opioid users not amenable to reductions.
Study Group
Group I: Subjects received single transforaminal epidural steroid injection with methylprednisolone acetate (20mg) and 0.25% bupivacaine (total 2 ml) with tab. Gabapentin (300mg thrice daily orally), tab. Amitriptyline (25mg once daily orally) and spine extension exercises.
Group II: Subjects were given only tab. Gabapentin (300mg thrice daily orally), tab. Amitriptyline (25mg once daily orally) and spine extension exercises.
Transforaminal Procedure
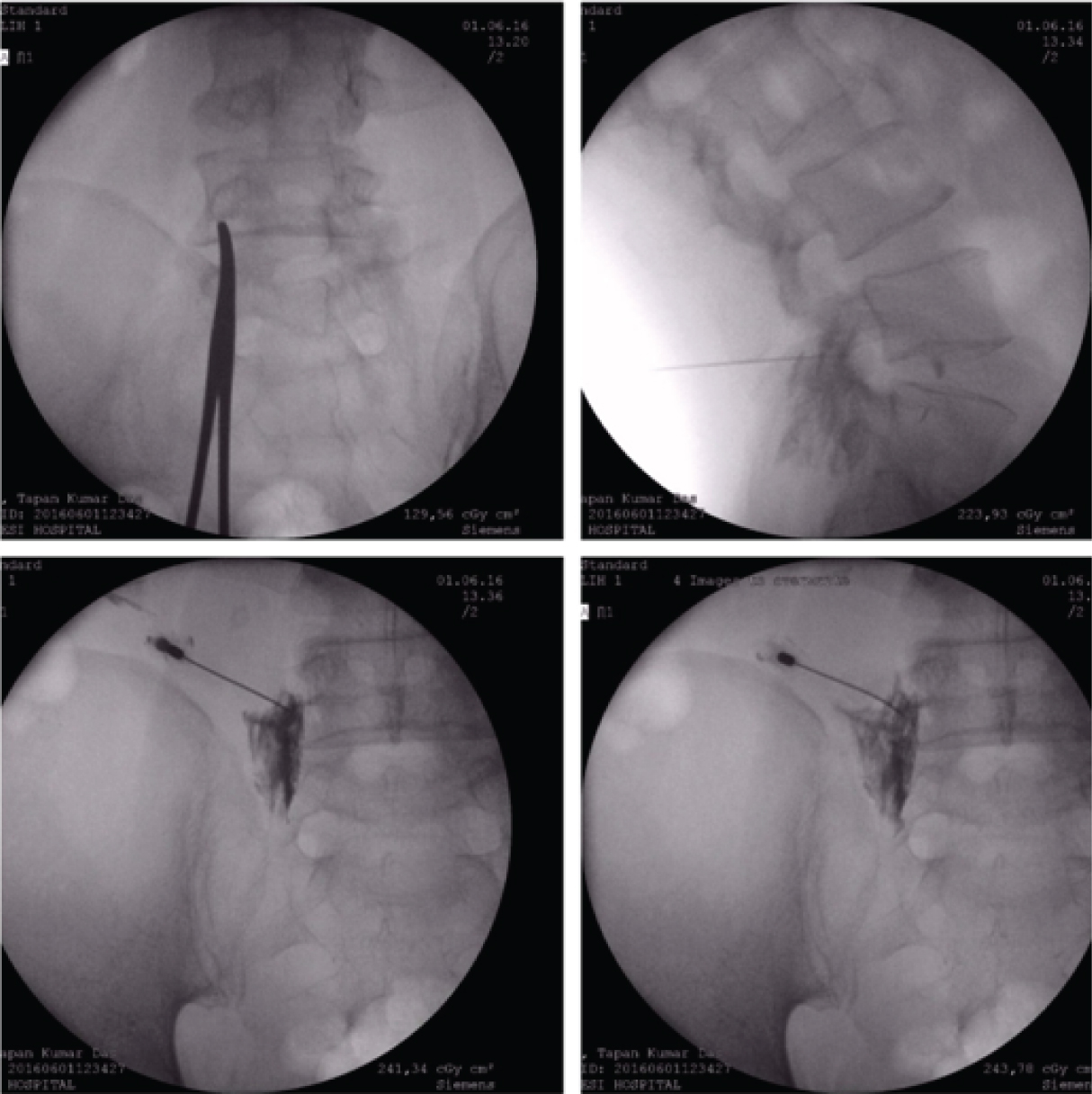
A 22-gauge, 3.5-inch Quincke’s needle was introduced at the level of disc lesion, using first an anteroposterior and, subsequently, an oblique orientation (15-30°) of the fluoroscopy C-arm to achieve the “Scotty Dog” appearance of the lumbar spine and then directed until the needle tip was in the posterior and superior aspect of the intervertebral foramen, as checked in the lateral imaging, and in line with the pedicle on anteroposterior view. Transforaminal epidural was restricted to L3-L4, L4-L5 and L5-S1 depending on the extent of pathology at one or two level and a C- arm fluoroscopy was used to confirm the presence of needle within canal [Table/Fig-1] [10].
Serial fluoroscopic views showing needle inserted at L5 foramina, with dye injected and subsequent fading of dye after drug instillation.
Confirmation of Epidural Steroid Injection
Once the needle was in position, and after negative aspiration for cerebrospinal fluid and blood, 1 ml contrast dye (OMNIPAQUE) was injected to confirm the epidural space distribution in the anteroposterior view. This was followed by further injection of contrast under live fluoroscopy, to confirm the spread of the contrast, as well as to verify that no contrast medium attained the intravascular, subarachnoid, subdural, or intra-discal spread.
Lateral images were taken to evaluate the ventral epidural space. Ventral spread was defined as present if contrast travelled along the posterior longitudinal ligament or adjacent to the posterior aspect of the contiguous vertebral body at the level of needle insertion [10]. After epidural space confirmation, deposteroid (20mg) and 0.25% bupivacaine (total 2 ml) were injected. All the patients were monitored for at least 30 minutes after procedure. Post injection, no complication was occurred. Method of pelvic angle measurement Kinematic study was done from human gait by image processing and pelvic angle measurement [4].
Apparatus and Procedure [4,8]. The subjects walked along an approximately 10 feet walkway in his comfortable speed. Among two digital cameras, one was placed along the midline of the walk-way and another at the front of the walk-way. Distance was maintained to take full picture of the patient (can be taken as front and lateral view).
The adhesive colourful markers were attached at the following anatomical landmarks: the greater trochanter at hip joint level, along the ASIS, PSIS and midpoint of patella on both sides. We have asked all patients to walk in a normal speed.
Data were collected after 15 seconds of walking and stored into the computer. Measurements were taken on one selected stance phase of affected limb from a particular gait cycle by slowing down the video using VLC media player. Here, we have measured angle of hip at heel strike, heel off and toe off in a single stance phase. Then, mean was calculated from these three phases.
Data Collection
All patients attending pain clinic, fulfilling the above criteria, after taking informed consent were included by primary investigator into the above study. Detailed clinical history was taken, according to a prefixed performa, from all the patients. Physical examination, pain intensity rating by NRS scale and disability rating by modified ODI score and kinematic study as pelvic angle measurement were subsequently done for all patients. Then randomization was done by computer generated random number tables. All patients were divided into 2 groups (Group I and II). Proposed treatment was given to each patient on 1st visit (Visit 1). Then they were followed up after one month on next visit i.e., Visit 2: Unfortunately, 4 patients were dropped out from study.
The statistical software SPSS version 20 has been used for the analysis. Categorical variables like gender are expressed as Number of patients and Percentage of patients and compared across the groups using Pearson’s Chi Square test for Independence of attributes. Continuous variables are expressed as Mean±Standard Deviation and compared across the 2 groups using Mann-Whitney U test since the variables does not follow normal distribution. Over time, comparison have been done using Wilcoxon Signed Ranks Test. An alpha level of 5% has been taken, i.e., if any p-value is less than 0.05; it has been considered as significant.
Results
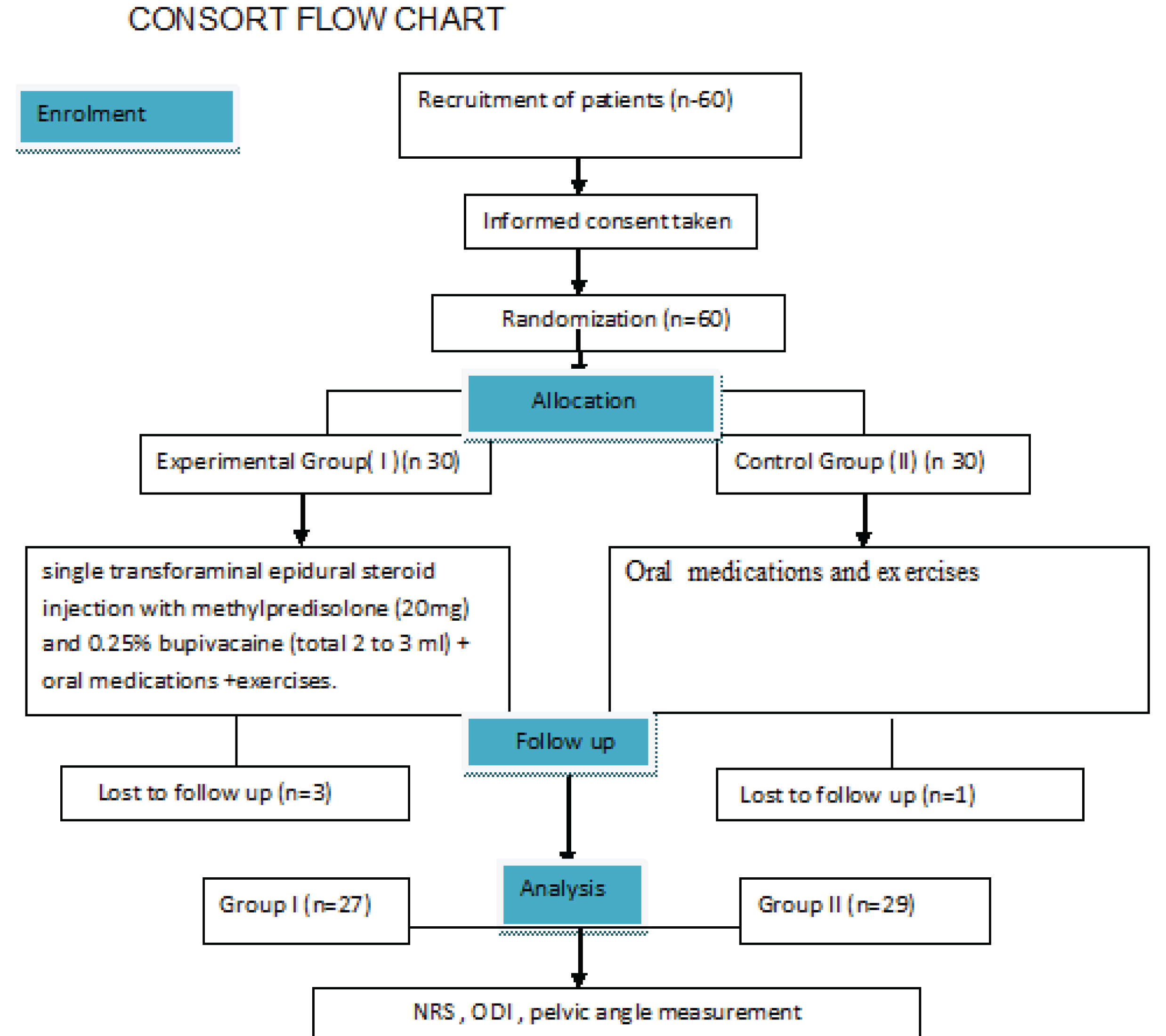
In this randomized controlled trial 60 patients with chronic LBP with unilateral radiculopathy were included into this trial. Of the 60 participants, 3 participants from experimental group and 1 participant from control group discontinued intervention, 27 participants were given transforaminal epidural steroid injection (group I) and 29 participants received conservative treatment (group II) [Table/Fig-2].
Demographic Characteristics
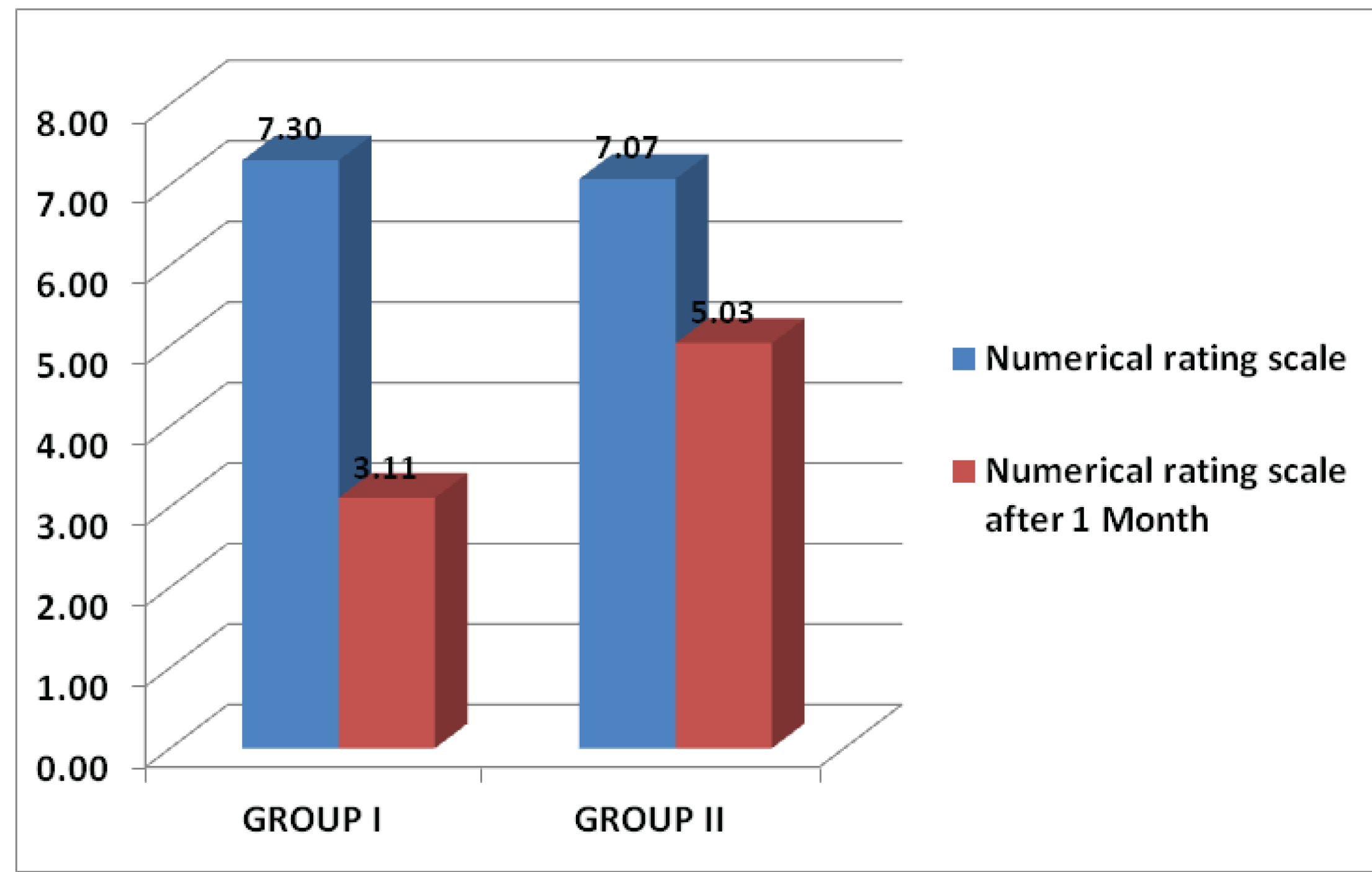
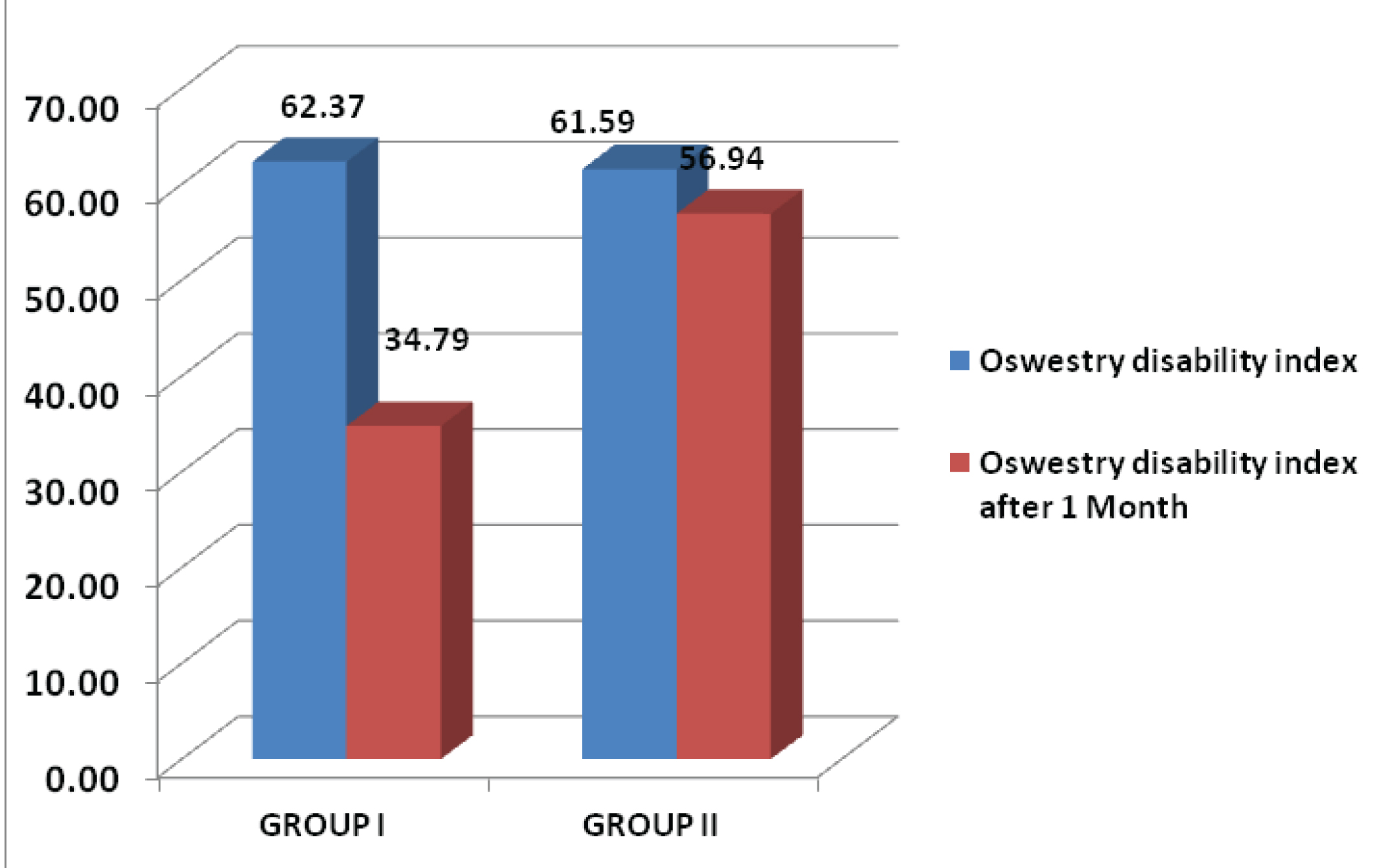
Incidence of LBP was more in males than females. In group I, incidence among males and females were 81.50% and 18.50% respectively. In group II, it was 75.90% and 24.10% for males and females respectively (base line p-value was 0.609). All the subjects were industrial workers. No significant differences between group I and II were found in age distribution (42.11±8.577 Vs 48.38±6.389 years with p-value) respectively. Both NRS scores for pain intensity measurement [Table/Fig-3] and modified Oswestry Disability Index Score after treatment, at visit 2 (V2), was significantly improved over visit 1(V1) (p-value is <0.001) in both the groups [Table/Fig-3,4].
0-10 Numeric Rating scale (NRS) scores for pain intensity measurements in different visits.
Oswestry Disability Index Scores in different visits.
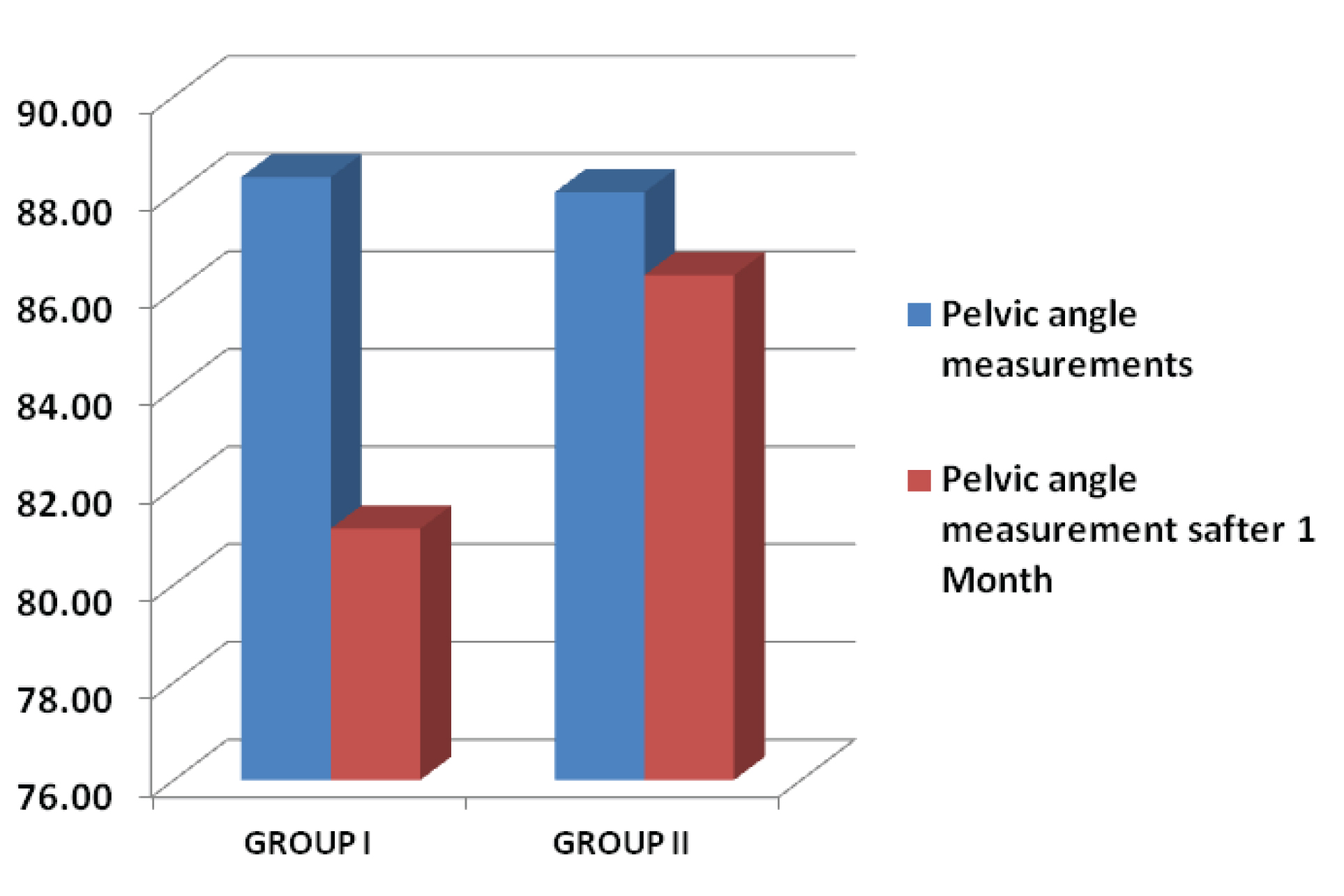
The mean of Pelvic angle measurements of affected side of group I, at visit 1 was 88.33 degrees and of group II, was 87.62 degrees. After treatment, at visit 2, mean of group I was 81.07degrees and of group II was 85.92 degrees. A p-value of group I is <0.001 [Table/Fig-5].
Pelvic angle measurements in two visits in different groups.
Both the groups had exhibited significant changes in all 3 parameters from baseline. But the changes were more pronounced (p-value <0.001) in Group I. To show differences of outcome measurements, we had also compared the changes in the parameters between the 2 groups [Table/Fig-6].
Comparison of differences in 3 parameters in 2 groups after 1 month.
| GROUP | | Change in Numerical rating scale after 1 Month | Change in Oswestry disability index after 1 Month | Change in Pelvic angle measurements after 1 Month |
|---|
| GROUP I | Number of Cases | 27 | 27 | 27 |
| Mean | -4.19 | -27.58 | -7.20 |
| Std. Deviation | 1.00 | 5.08 | 3.05 |
| GROUP II | Number of Cases | 29 | 29 | 29 |
| Mean | -1.10 | -4.65 | -1.70 |
| Std. Deviation | 0.77 | 4.49 | 1.21 |
| p-Value | | <0.001 | <0.001 | <0.001 |
Discussion
LBP with unilateral radiculopathy due to lumber disc herniation has now become a real rehabilitation and management challenge in our society. Herniated lumber disc is the most common cause of radicular pain. It has been demonstrated that nerve root exposed to herniated disc causes release of inflammatory mediators and inflammation of surrounding neural structures, which cause low back pain with radiculopathy. This clinical trial aimed to compare the efficacy of two different treatment approaches to unilateral radicular pain due to disc herniation. It was conducted in ESI institute of pain management for the industrial workers at Kolkata, India, comprising age group of 18 to 60 years. Here, incidence among males was more than female and all 60 were industrial workers. Most of them were middle aged. Generally jute workers are habituated with very heavy work. They work also in a particular position (stooping forward) for a long time. So, they may get trauma or fall on back leading to low back pain [6]. For diagnosing radicular pain, electrophysiological studies, radiological imaging and MRI scan are essential along with history taking from patient, physical examination.
According to Coster S et al., in clinical practice, dermatomal radiation, more pain on coughing, sneezing or straining, positive straight leg raising and ongoing denervation on EMG may be used to predict nerve root compression on MRI [11]. Some studies showed that gait analysis has also some role in diagnosis of radicular pain. Zahrae MH et al., conducted a study to analyse asymmetry and loading patterns in patients with nonspecific chronic LBP compared to normal individuals [12], during walking; where he concluded that chronic LBP subjects follow avoidance-endurance model without any limitation during walking. Another study done by JF Seay et al., assessed pelvis and trunk differences during walking and running between runners with LBP, runners with resolved LBP, and subjects with no history of LBP [13]. Shum GL et al., tried to examine differences in the kinematics and joint coordination of the lumbar spine and hips during sit-to-stand and stand-to-sit between healthy subjects and patients with sub-acute LBP [14]. Some angle measurements were significantly altered in back pain subjects; in particular, those with positive straight leg raise sign. Yokogawa N et al., performed a study on 2015 to differentially diagnose thigh pain from lumbar spinal stenosis (particularly lumbar fourth nerve root radiculopathy) and osteoarthritis of the hip [15]. They have demonstrated differences in gait characteristics of L4 radiculopathy and hip osteoarthritis by using a very simple gait analysis method of treadmill and motion analysis. Above studies showed that gait analysis can differentiate lumber spinal stenosis and lumber disc herniation and also can predict how normal body ergonomics can change with such diseases.
A multi-disciplinary approach is required in managing unilateral radicular pain due to lumber disc herniation. According to Collinghan N and Gupta S steroid delivery to lumbar epidural space is an effective mode of treatment [16]. Transforaminal approach rather than intralaminar or caudal route is more specific and amount of steroid requirement is also less under fluoroscopic guidance. Transforaminal epidural injection is commonly used in LBP with unilateral radiculopathy refractory to other conservative treatment options. Manchikanti L et al., published a systematic review article in pain physician journal, 2012 on effectiveness of transforaminal steroid injections in lumber spinal pain the evidence is good for radiculitis secondary to disc herniation with local anaesthetics and steroids and fair with local anaesthetic only [17]. Buenaventura RM et al., tried to evaluate the effect of transforaminal lumbar epidural steroid injections in managing lumbar (low-back) and sciatica (leg) pain and said that transforaminal lumbar epidural steroid injections are Level II- 1 for short-term relief and Level II-2 for long-term improvement in the management of lumbar nerve root [18]. Kim JH et al., evaluated and compared the efficacy of transforaminal epidural block in far lateral herniation of the lumbar disc (FHLD) and the intraspinal herniation of lumbar disc (iHLD) patients [19]. He noted, approximately no failure for TFESI in the both the groups, but better result on iHLD group. They have used particulate steroid for transforaminal epidural injections. In these studies, we tried to investigate that the transforaminal epidural injection was superior to conservative treatment.
Epidural steroid are used in the treatment of radicular pain with discogenic origin. Methylprednisolone acetate is a particulate steroid. Methylprednisolone have particles consistently smaller than a red blood cell (7.5–7.8 mm) and has both glucocorticoid and mineralocorticoid activity [16]. In an article, Collinghan N and Gupta S [16] mentioned that, the particulate steroid preparation (triamcinolone) showed greater pain relief than dexamethasone. In some other studies [17,19] also methylprednisolone or particulate steroid has been used for transforaminal injection and improvement was noted. Here, in our clinical trial, we have also used methylprednisolone acetate for transforaminal injection along with local anaesthetic and good pain relief was occurred. Post intervention, no complications were noted. For measurement of outcome of our study, we have used 0-10 numerical rating scale for measuring pain prior and after the treatment. Most of the studies used NRS Score for pain outcome measurement [20]. Modified Oswestry Disability Index (ODI) score [21] was utilised in our clinical trial for assessment of quality of life changes with treatment in two visits. This index is designed to describe how much a subject’s back pain has affected the ability to manage their daily activities. Seyed Masoud Hashemi et al., conducted study where he compared between transforaminal and parasagittal epidural steroid injection in patient with radicular LBP [22]. They have used NRS for pain intensity measurement and ODI scores for functional assessment. In our study, NRS for pain intensity measurement and Modified ODI score were significantly decreased in group I than group II with p-value <0.001.
We have calculated pelvic angles at side with radiculopathy as a part of kinematic study and seen changes after intervention. The most plausible explanation in present study of the altered pelvis angulations after transforaminal injection on affected side was that to maintain near normal stride length by altering pelvic angulation. In our study, in group I patients, their pelvic angulations were decreased significantly with p-value of 0.017 after treatment. So, we can predict that, transforaminal epidural steroid injection produces a significant improvement in gait by altering pelvic angles after 1 month. Further multicentric randomized controlled trials and long term follow up are needed to evaluate the efficacy of transforaminal steroid injection.
Limitation
The limitation of this study is its small sample size.
Conclusion
Disability related to chronic LBP is a multifactorial phenomenon, associated with high social and health costs. Treatment regimens in most of the times for lumbar radicular pain for disc herniation include oral medications and exercises. Transforaminal epidural steroid injection is an effective adjunct to this usual conservative treatment protocol. It causes improvement not only in Numerical rating scale of pain intensity measurements and Modified Oswestry disability index scores significantly but also improved walking pattern by changing pelvic angulations significantly.